Immediate pharmacologic and surgical stabilization is essential to promote maximum neurological recovery in acute spinal cord injury.
Mr. Ethan Kosco, University of Toledo College of Medicine and Life Sciences, Toledo, Ohio. E-mail: ekosco@rockets.utoledo.edu
Introduction: Spinal cord injury (SCI) is most common following trauma, typically involving motor vehicle incidents. The clinical prognosis depends on many factors, most importantly the initial grade of injury.
Case Report: We present a 26-year-old male who presents to the emergency department after a motor vehicle accident. He sustained significant injuries with an initial Glasgow Coma Scale of 3 and signs of complete SCI. A computed tomography scan demonstrated cervicomedullary transection caused by C6-C7 facet distraction with C6 retrolisthesis on C7. The patient recovered the ability to track with eyes, utilize facial expression, and unilateral trapezius function to command. Neurological recovery was not made despite aggressive treatment.
Conclusion: Patients with complete SCI typically have poor outcomes despite aggressive treatment. We present a unique mechanism, treatment, and outcome of a cervicomedullary SCI through C6 retrolisthesis on C7.
Keywords: Cervicomedullary, spinal cord injury, transection, retrolisthesis, trauma.
Spinal cord injury (SCI) has a global incidence of 133,000–226,000 cases annually, most commonly occurring in males after motor vehicle collision [1]. The degree of SCI is determined by neurological evaluation and can be classified by the American Spinal Injury Association Impairment Scale. Grade A is a complete SCI or no motor and sensory innervation including sacral roots, distal to the injury site [1]. Retrolisthesis of the spine occurs when a single vertebra displaces posteriorly below a disc. It is caused by osteoporosis, malnutrition, and arthritis, but can also be a result of trauma and congenital abnormalities. Symptoms can present as pain, weakness, or numbness in the extremity supplied by the nerve root [2].
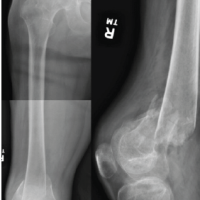
A 26-year-old male presented to the emergency department through emergency medical services (EMS) after a motor vehicle accident (MVA). The patient had been found unrestrained and partially ejected from the vehicle. On initial presentation, the patient was in asystole, EMS resuscitated, and subsequently intubated. Neurologically he presented with mid position, non-reactive pupils, and a Glasgow Coma Scale of 3. With evidence of spine trauma, a computed tomography scan was obtained revealing a C6-C7 facet distraction and high-grade C6 retrolisthesis on C7 in addition to numerous fractures (Fig. 1).
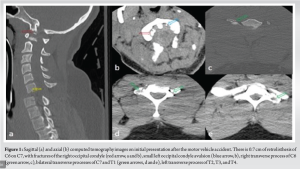
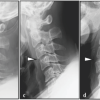
Magnetic resonance imaging revealed a transected spinal cord just below the cervical-medullary junction (Fig. 2). Associated edema throughout the medulla and spinal cord, intramedullary blood product, and extensive bleeding within the spinal canal were also seen. Complete ligamentous tearing and C6-C7 disc rupture with posterior protrusion were also noted at the level of distraction.

Several days later, the patient could track with eyes, blink, and raise eyebrows on command, but no lower cranial nerve function was present. The family decided to pursue aggressive management. A C6-C7 reduction was performed along with C4-T2 instrumentation and fusion (Fig. 3). Two months after the incident the patient had minimal neurological improvement with the gain of symmetric facial movement and some motor of the right trapezius.
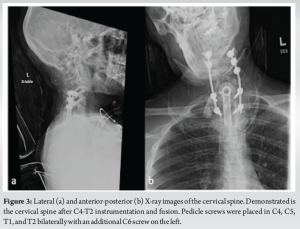
Approximately 30–60% of spinal cord injuries are initially neurologically complete, with up to 30% of these patients converting to incomplete within 30 days [2]. Patients with complete SCI typically have the least amount of motor score improvement in 1 year. We present a patient with a complete SCI due to a traumatic MVA. His critical condition and cervicomedullary location of SCI led to a poor outcome. Primary indicated measures of acute SCI include airway management, maintaining mean arterial pressure at 85–90 mmHg, and immediate spinal cord decompression and stabilization through minimizing neck movement [3-5]. Unstable cervical injury often utilizes a fusion of the vertebrae and internal fixation with metal plates and screws [6], which is the procedure used in this patient. There are several therapies including corticosteroids and neuroprotective agents, but there is little evidence to guide these treatment modalities [3-5, 7, 8]. The outcomes of cervical SCI depend on the severity of disruption as well as other associated injuries, head trauma, and age [6]. In addition to acute care in SCI patients, it is also crucial to address long-term care, rehabilitation strategies, and the psychosocial and economic problems associated with serious disability and the loss of work. These factors are often managed by physiotherapists, occupational therapists, dieticians, psychologists, social workers, and the patient’s family [4]. This team can constantly monitor and modify the best treatment course for the patients while considering each aspect of health. Although complete neurological recovery is not expected – especially in complete SCI patients, the greatest social, physical, and domestic benefits are associated with the realization of independent mobilization during the chronic period [9,10].
The most common cause of SCI is trauma from a MVA. Patients with spinal cord transection or complete injury typically have the least neurological recovery and poor outcomes despite aggressive treatment courses. We present the case of a unique mechanism of complete SCI, specifically C6 retrolisthesis on C7 causing spinal cord avulsion. Management includes rapid dopamine and norepinephrine pressors and reduction/decompression of the C6 and C7 segments with posterior fusion for stabilization. Unfortunately, the patient did not achieve a significant gain in neurological function. Moreover, the patient is unlikely to have further improvement due to the minimal neurological recovery achieved at 2 months. However, new research is emerging regarding alternative types of management for this type of injury mechanism. Rapid corticosteroid administration and the use of neuroprotective and neurodegenerative agents are potential management strategies. Additional research is warranted to determine the efficacy of these treatment modalities in this type of severe neurological trauma.
We present the diagnosis, stabilization, management, and outcome of a cervicomedullary transection caused by C6-C7 facet distraction with C6 retrolisthesis on C7 caused by a MVA. Although the patient became quadriplegic due to the injuries sustained by the accident, this manuscript lays the foundation for the immediate steps a spine surgeon must take to increase the likelihood of neurological recovery. We believe continuing to follow this protocol can result in a tremendous improvement in the quality of life of patients who would have otherwise become severely incapacitated.
References
- 1.Roberts T, Leonard G, Cepela D. Classifications in Brief: American Spinal Injury Association (ASIA) impairment scale. Clin Orthop Relat Res 2017;475:1499-504. [Google Scholar | PubMed]
- 2.Kawasaki M, Tani T, Ushida T, Ishida K. Anterolisthesis and retrolisthesis of the cervical spine in cervical spondylotic myelopathy in the elderly. J Orthop Sci 2007;12:207-13. [Google Scholar | PubMed]
- 3.Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte DW, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One 2012;7:32037. [Google Scholar | PubMed]
- 4.Rouanet C, Reges D, Rocha E, Gagliardi V, Silva GS. Traumatic spinal cord injury: Current concepts and treatment update. Arq Neuropsiquiatr 2017;75:387-93. [Google Scholar | PubMed]
- 5.Vazquez RG, Sedes PR, Farina MM, Montoto Marqués A, Ferreiro Velasco ME. Respiratory management in the patient with spinal cord injury. Biomed Res Int 2013;2013:168757. [Google Scholar | PubMed]
- 6.Torlincasi AM, Waseem M. Cervical injury. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. [Google Scholar | PubMed]
- 7.Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE. Guidelines for the management of acute cervical spine and spinal cord injuries. Neurosurgery 2013;60:82-91. [Google Scholar | PubMed]
- 8.Wilson JR, Forgione N, Fehlings MG. Emerging therapies for acute traumatic spinal cord injury. CMAJ 2013;185:485-92. [Google Scholar | PubMed]
- 9.Nas K, Yazmalar L, Şah V, Aydın A, Öneş K. Rehabilitation of spinal cord injuries. World J Orthop 2015;18:8-16. [Google Scholar | PubMed]
- 10.Kirshblum S, Snider B, Eren F, Guest J. Characterizing natural recovery after traumatic spinal cord injury. J Neurotrauma 2021;1:1267-84. [Google Scholar | PubMed]