A Clay shoveler is rare in pediatric patients. A detailed history and physical examination are crucial to differentiate from other causes of spinal pain. Imaging studies such as X-rays are essential for confirming the diagnosis. Recognizing this fracture in children on imaging can be challenging due to differences in bone development and ossification. Treatment is typically conservative, involving rest, immobilization, and pain management. Understanding the importance of growth plates in children is critical when planning treatment to avoid long-term complications.
Dr. Panagiotis Antzoulas, Department of Orthopaedic, Medical School, University of Patras, Patras, Greece. E-mail: p.antzoulas@hotmail.com
Introduction: A clay-shoveler’s fracture is a relatively uncommon stress-type avulsion fracture typically affecting the lower cervical or upper thoracic spinous processes. Historically named after clay shovelers due to their predisposition to such injuries, this type of fracture is now more frequently observed in individuals participating in sports activities that entail rotational movements of the upper spine.
Case Report: A 13-year-old patient, while performing agricultural work and using a manual shovel to excavate an area, experienced cramping in the cervical spine, neck pain, and a significant limitation in the range of motion. The patient presented with a history and physical examination suggestive of a clay-shoveler’s fracture. Subsequent X-ray images demonstrated an acute soft-tissue avulsion of the spinous process at C7. With non-operative therapy, the patient returned to work within 2 months, experiencing occasional, intermittent discomfort 6 months after the injury, which did not limit any activities. After 2 years of follow-up, the patient reported no pain.
Conclusion: A clay-shoveler’s fracture is a rare stress-type avulsion fracture, particularly in children. Diagnosis necessitates clinical suspicion, a targeted history, and a thorough physical examination. Radiographs play a crucial role, and in challenging cases, magnetic resonance imaging may be warranted to detect soft-tissue avulsions. Treatment typically involves cervical immobilization of the cervical spine for 4–6 weeks.
Keywords: Cervical spine fracture, spinous process, spine, clay-shoveler’s fracture, children
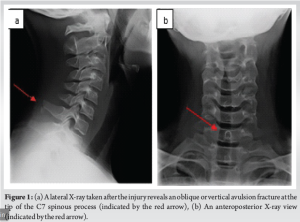
The clay-shoveler’s fracture, named after Australian clay shovelers from the 1930s, occurs due to high-energy, repetitive pulling actions often associated with shoveling or digging [1]. This type of fracture was first documented in 1875 among workers performing repetitive tasks that strained the upper back muscles [2]. It is characterized by sudden, violent pain in the upper back, often accompanied by a crunching sensation, which incapacitates the worker [1]. In the early twentieth century, numerous cases were reported worldwide under various names [1]. However, it was consistently noted that the affected workers were involved in activities such as shoveling or digging [1]. In 1940, with studies like that of McKellar, the term “Clay Shoveler Fracture” was established [2]. The avulsion mechanism, resulting from stress on the spinous processes, typically occurs due to high shear forces generated by the contraction of the trapezius and rhomboid muscles [3]. These forces act on the lower cervical and upper thoracic spinous processes during activities that involve sudden or forceful movements of the neck and/or shoulders, such as those seen in clay shoveling [4]. Recently, spinous process avulsion fractures have been reported because of various recreational activities, including weightlifting, baseball, volleyball, golfing, lambada dancing, and even gaming [4-9]. Usually, patients with clay-shoveler’s fractures present with radiographs showing a bony avulsion fracture at the tip of the spinous process, most frequently occurring at the levels of C6, C7, and T1 [3,5,6,9,10]. This condition is typically visualized as a clear bony avulsion of the spinous process on lateral radiographs or as a “double spinous process” sign on anterior-posterior radiographs [10]. In contrast, in adolescents, the literature indicates that the ossification center of the spinous process appears vaguely “around the time of puberty,” with complete ossification typically occurring around the third decade of life [11]. Thus, in adolescents, the apophysis at the tip of the spinous process may not be ossified, making it potentially invisible on standard radiographs [4]. Consequently, in adolescents with a history and physical examination findings consistent with clay-shoveler’s fracture, alongside “normal” radiographs, magnetic resonance imaging (MRI) may be warranted [4]. Whereas in the past this condition was considered an occupational injury primarily seen in laborers shoveling heavy loads, it is now mostly encountered in athletes or as recreational injuries. Here, we report a case of an adolescent sustaining a clay-shoveler’s fracture “the old-fashioned way,” during his agricultural work.
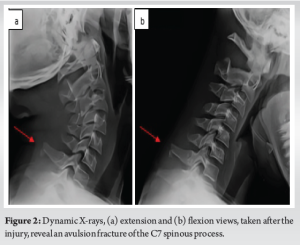
A 13-year-old male felt a “pop” in his neck and pain down his left arm while performing agricultural work and using a manual shovel to excavate an area. He consults the emergency department for experienced cramping in the cervical spine, neck pain, and a significant limitation in the range of motion. We examined the patient after the injury. Tenderness was localized to the posterior elements of C7, with no other abnormalities detected on examination, presenting pain in the posterior cervical region without improvement, and on physical examination, the patient felt pain on rotation and extension of the neck. On palpation of the lower cervical and upper thoracic spine with trigger point, for which plain radiographs were requested (Figs. 1 and 2), where there is evidence of a fracture line that compromises the spinous process of C7. Dynamic views, such as flexion and extension radiographs, are also crucial for assessing the stability of the cervical spine. These views help identify any abnormal movement or instability that may not be visible on static imaging. Based on all these findings, it was concluded that the patient exhibited an adolescent version of a clay-shoveler’s fracture. In this condition, the apophysis of the spinous process or other soft tissue had detached from the tip of the spinous process. We recommended a cessation of activities until the patient became pain-free. The parents were hesitant to consent to a computed tomography (CT) scan due to concerns about exposing their young child to radiation. Despite the doctor’s efforts to explain the nature of the fracture and the importance of imaging for a more detailed assessment, the parents ultimately declined the procedure. Since the child was 13 years old and did not present with any neurological problems, we decided not to perform a CT scan for further investigation.
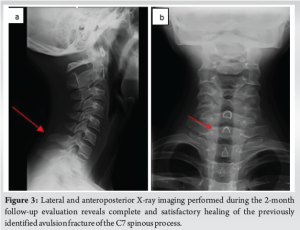
Without instability or connection of the spinal canal, this condition does not necessitate neurosurgical intervention. Medical management with a semirigid cervical collar was ordered for 1 month, analgesia with NSAIDs (paracetamol and ibuprofen), rest, ambulatory follow-up by algology, physiatry, and control appointment with orthopedics by outpatient consultation. With non-operative therapy, the patient returned to work within 2 months, experiencing occasional, intermittent discomfort 6 months after the injury, which did not limit any activities. Lateral and anteroposterior (AP) X-ray imaging performed during the 2-month follow-up evaluation reveals complete and satisfactory healing of the previously identified avulsion fracture of the C7 spinous process (Fig. 3). The images confirm the restoration of normal anatomical alignment and the absence of any residual deformity or complications, such as non-union or malunion (Fig. 3). After 2 years of follow-up, the patient reported no pain. He was fully engaged in all activities, including sports, without any restrictions.
The first documentation of spinous process fractures in laborers after repetitive pull of the upper back muscles allegedly dates from around 1875 [7]. Clay-shoveler’s fractures became a clinically recognized entity in western Australia in the 1930s and are, since then, referred to as such [1]. The spinous processes of the C7 and T1 vertebrae have a longer and thinner structure that makes them less resistant to stress forces, predisposing them to destabilize and fracture [1]. Their horizontal orientation and the perpendicular direction of the muscular forces contribute to the development of this type of injury, which can also, though less frequently, occur at any lower cervical or upper thoracic level [2]. Forced unilateral traction, especially created by the trapezius and rhomboid minor muscles, along with increased tension caused by stress on the nuchal ligament, plays an essential role in the avulsion of the C7 or T1 spinous processes [1]. This causes posterior displacement of the fracture, with the distal fragment being oriented in the direction of the caudal and lateral traction exerted by these muscles [2]. The clinical features of a clay-shoveler’s fracture can vary depending on the severity of the injury and the location of the fracture. The most frequent clinical presentation involves a sudden onset of pain in the lower part of the neck or upper part of the back, specifically around the affected spinous processes [5]. Classic clay-shoveler’s fractures are considered stable [1]. However, if the fracture extends to the vertebral body or other regions of the vertebra, evaluation for spinal cord involvement is necessary [11]. This includes checking for spinal instability, spinal cord compression, or radiculopathy. The clinical examination and radiological diagnosis of a clay-shoveler’s fracture are crucial for the accurate identification and management of this condition. Clinically, patients may present with localized pain, tenderness over the cervical or upper thoracic spine, and limited range of motion, often exacerbated by activity or palpation. Neurological deficits are typically absent due to the fracture’s stable nature. Radiologically, the diagnosis is typically confirmed using simple radiographs. Standard AP and lateral views are sufficient to visualize the fracture, which usually appears as an avulsion of the spinous process, most commonly in the lower cervical or upper thoracic vertebrae (e.g., C7 or T1). Dynamic views, such as flexion and extension radiographs, are also crucial for assessing the stability of the cervical spine. These views help identify any abnormal movement or instability that may not be visible on static imaging. The lateral view often provides the clearest depiction of the displaced bony fragment, whereas the AP view may assist in confirming the level of injury and ruling out additional abnormalities [4]. CT scans and MRI of the cervical and thoracic spine provide a more detailed characterization of the fracture and any associated injuries, especially in high-impact trauma scenarios [2]. Conservative treatment is the standard approach for managing a clay-shoveler’s fracture, primarily involving rest from activities that cause pain, with most patients recovering after a period of relative rest [4,12]. However, in some cases, delayed union or non-union fractures can result in persistent symptoms [12]. Options for such cases are limited, but surgical excision of the fracture fragment has been reported in some instances [13]. Yamaguchi et al. presented two cases involving a 14-year-old baseball player and a 16-year-old wrestler, both of whom experienced acute posterior neck pain following sports activities [4]. Despite the lack of radiographic evidence of injury, subsequent MRI scans revealed acute soft-tissue avulsion of the spinous process at C7 in one patient and T2 in the other. Both patients underwent non-operative therapy and returned to sports within 4 months, although they experienced occasional, intermittent discomfort a year post-injury, which did not restrict their activities. In another case, Hasley et al. described a 14-year-old competitive swimmer who, after initial treatment failure, received an ultrasound-guided anesthetic/corticosteroid injection at the site of the avulsion fracture [12]. This intervention led to rapid symptom relief and allowed the athlete to return to sport. The authors suggested that such an injection might serve both diagnostic and therapeutic purposes before considering surgical excision in cases of delayed union or non-union clay-shoveler’s fractures. While clay-shoveler’s fractures in athletes are typically treated conservatively with rest, activity modification, and a return to activities when symptoms subside, non-union of these fractures can occur due to the ligamentous attachments and muscular forces acting on the fracture fragment. Surgical treatment for recalcitrant symptomatic non-unions in adolescent athletes has not been well-documented in the literature. Murphy et al. examined the medical records and radiographs of adolescent athletes with persistent symptoms related to a T1 spinous process non-union [13]. Three adolescent athletes who underwent surgical excision of a non-united ossicle following a T1 spinous process fracture after conservative treatment failed were identified [13]. All patients experienced complete pain relief and returned to sports post-surgery, with no surgical complications reported. This case series was the first to document surgical excision of the non-united ossicle in athletes unable to return to play due to persistent disabling pain at the non-union site [13]. Surgical excision should be considered for patients with persistent pain following this injury, with the expectation of complete symptom resolution after surgery [13].
In the case we describe, the patient sustained the injury while shoveling in an occupational setting. Our case aligns with previously published reports, with radiographs confirming the diagnosis and a purely conservative treatment approach consisting of rest, analgesics, and a return to activity after symptom resolution. While we are hesitant to recommend treatment based on a single case, the lack of other recommendations in the literature warrants some discussion.
Conservative treatment remains the primary option for managing clay-shoveler’s fractures, typically yielding favorable clinical outcomes with adequate analgesic management, combined with cervical immobilization for 4–6 weeks and regular follow-ups. An ultrasound-guided anesthetic/corticosteroid injection at the avulsion fracture site may be beneficial for both diagnostic and therapeutic purposes before considering surgical excision in cases of delayed union or non-union. Surgical excision should be considered for patients with persistent pain post-injury, with an expectation of complete symptom resolution following surgery.
Early recognition and diagnosis of Clay-shoveler’s fracture are crucial. This condition should be considered in the differential diagnosis of upper thoracic or lower cervical spinal pain following trauma or excessive muscular exertion. Proper imaging, such as X-rays, is essential for identifying the avulsion fracture, particularly in pediatric patients, where skeletal immaturity can obscure findings. These fractures typically have a good prognosis with conservative treatment, including rest, immobilization, and pain management, making early and accurate diagnosis vital to avoid unnecessary interventions.
References
- 1.Reyes Bello JS, Castiblanco Varón DF, Rozo Saavedra JL, Restrepo Lugo CM, Perez Mendez JN, Moscote Salazar LR. The clay-shoveler’s fracture, a rare occupational injury in the modern era: A case report. Egypt J Neurosurg 2023;39:23. [Google Scholar | PubMed]
- 2.Posthuma de Boer J, Van Wulfften Palthe AF, Stadhouder A, Bloemers FW. The clay shoveler’s fracture: A case report and review of the literature. J Emerg Med 2016;51:292-7. [Google Scholar | PubMed]
- 3.Hall RD. Clay-shoveler’s fracture. J Bone Joint Surg 1940;22:63-75. [Google Scholar | PubMed]
- 4.Yamaguchi KT Jr., Myung KS, Alonso MA, Skaggs DL. Clay-shoveler’s fracture equivalent in children. Spine (Phila Pa 1976) 2012;26:1672-5. [Google Scholar | PubMed]
- 5.Herrick RT. Clay-shoveler’s fracture in power-lifting: A case report. Am J Sports Med 1981;9:29-30. [Google Scholar | PubMed]
- 6.Thomson LP, Stein LA, Fish WW. Lambada fracture. N Engl J Med 1991;324:852. [Google Scholar | PubMed]
- 7.Hestroni I, Mann G, Dolev E, Morgenstern D, Nyska M. Clay shoveler’s fracture in a volleyball player. Phys Sportsmed 2005;33:38-42. [Google Scholar | PubMed]
- 8.Brown CN, McKenna P. A Wii-related clay-shoveler’s fracture. ScientificWorldJournal 2009;9:1190-1. [Google Scholar | PubMed]
- 9.Kang DH, Lee SH. Multiple spinous process fractures of the thoracic vertebrae (clay-shoveler’s fracture) in a beginning golfer: A case report. Spine (Phila Pa 1976) 2009;34:534-7. [Google Scholar | PubMed]
- 10.Matar LD, Helms CA, Richardson WJ. “Spinolaminar breach”: An important sign in cervical spinous process fractures. Skeletal Radiol 2000;29:75-80. [Google Scholar | PubMed]
- 11.Lustrin ES, Karakas SP, Ortiz AO, Cinnamon J, Castillo M, Vaheesan K, et al. Pediatric cervical spine: Normal anatomy, variants, and trauma. Radiographics 2003;23:539-60. [Google Scholar | PubMed]
- 12.Hasley IB, Gruner MP, Soma DB, Sellon JL. Persistent pain after clay shoveler’s fracture delayed union: The role for ultrasound-guided corticosteroid injection. Int J Sports Exerc Med 2021;7:189. [Google Scholar | PubMed]
- 13.Murphy RF, Hedequist D. Excision of symptomatic spinous process nonunion in adolescent athletes. Am J Orthop (Belle Mead NJ) 2015;44:515-7. [Google Scholar | PubMed]