Caudal epidural steroid injection is a simple, safe, and efficacious technique comparable to transforaminal selective nerve root block in the management of unilateral L5-S1 paracentral discogenic radicular pain with significantly less procedural time and fluoroscopy usage.
Dr. Sathish Muthu, Department of Orthopaedics, Government Medical College, Karur, Tamil Nadu, India. E-mail: drsathishmuthu@gmail.com
Introduction: Epidural steroid injection (ESI) is one of the key management strategies in the management of discogenic radicular pain. This study aims to compare the efficacy and safety of fluoroscopy-guided ESI through caudal (cESI) and transforaminal (tfESI) routes for unilateral paracentral L5-S1 discogenic radicular pain.
Materials and Methods: This prospective non-randomized comparative study conducted between January 2023 and January 2024 in a tertiary care hospital included patients presenting with unilateral paracentral L5-S1 discogenic radicular pain who failed 6 weeks of conservative care. The pain and functional outcome was analyzed using numerical pain rating scale (NPRS) and Oswestry disability index, respectively, at baseline, 3-week, 6-week, and 6-month post-intervention. Procedure failure is defined as NPRS score improvement <50% or ODI improvement <40% of baseline. Other outcomes analyzed were the duration of the procedure, and fluoroscopy shots used during the procedure.
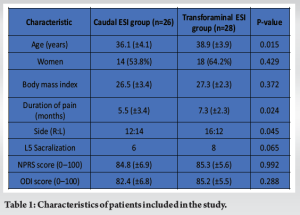
Results: We enrolled 60 patients in the study, 54 patients were available till the final follow-up with 26 patients in the cESI group and 28 patients in the tfESI group. The mean age of the cESI group (M: F 12:14) and tfESI group (M:F 10:18) was 36.1 (±4.1) years and 38.9 (±3.9) years, respectively. The pain and functional scores were significantly reduced compared to the baseline scores in both the groups (P < 0.001) and the reduction between the two groups was comparable at every follow-up. The tfESI group experienced significantly more failures (n = 8) at 6 months compared to the cESI group (n = 2) (P = 0.048). The tfESI group had significantly longer mean procedure time (18.8 min) and more fluoroscopy usage (16 shots) compared to cESI group with mean procedure time of 13 min (P = 0.014) and fluoroscopy usage of 10 shots (P = 0.023), respectively. No major adverse events were reported for either of the groups.
Conclusion: cESI is a simple, safe, and efficacious technique comparable to tfESI in the management of unilateral L5-S1 paracentral discogenic radicular pain with significantly less procedural time and fluoroscopy usage. Further, large-scale studies are needed to validate the study results.
Keywords: Radicular pain, epidural steroid injection, caudal epidural, selective nerve root block, discogenic pain.
Low back pain (LBP) constitutes one of the major health problems with a lifetime prevalence as high as 80% and an annual prevalence of up to 45% [1]. Based on the WHO estimates, 1 in 13 people suffered from LBP amounting to 619 million, which is a 60% rise compared to 1990 and it is expected to rise to 843 million by 2050 [2]. Studies analyzing the estimates of LBP noted that >25% of patients report high-intensity pain with significant disability in their day-to-day living [3,4]. Not only younger adults suffer from discogenic LBP, but the elderly also suffer from the disease due to degenerative disc disorders and it stands as an independent factor that affects the functional capacity [5-7]. Further, LBP has serious economic, societal, and health impacts that made the WHO release global guidelines on LBP management [8]. Intervertebral discs, ligaments, facet joints, muscles, fascia, and nerve roots were identified as structures capable of producing LBP [9]. Of all the mentioned structures, intervertebral disc commonly results in discogenic LBP secondary to disruption of the disc resulting in herniation and nerve root compression [10,11]. Apart from disrupted disc, root compression can also be caused by degenerative stenosis of the foramen due to facetal hypertrophy and facetal osteoarthritis [12]. Disc disruption results in chemical radiculitis resulting in radicular LBP [11,13]. Management of LBP with epidural injections has been one of the commonly preferred non-surgical treatment methods [14]. However, the role of injecting steroid and local anesthetic in the epidural space in managing neurogenic pain is still not well understood. The transient neural blockage achieved with the injection is considered to alter or interrupt the nociceptive input and the reflex mechanisms involved in the afferent pain fibers, along with its self-sustaining activity and patterning of the central neuronal activities [1,15,16]. The corticosteroids have been shown to decrease neuronal inflammation through inhibition of either the production or release of pro-inflammatory cytokines resulting in a reversible anesthetic effect [17,18]. Further, the local anesthetic combined with the corticosteroid in the epidural injections was shown to provide short and long-term pain relief by direct suppression of the nociceptive discharge [19,20], inhibition of the sympathetic reflex arch [19], and its related axonal transport [21,22] along with blockade of sensitization [23] and anti-inflammatory effects [24]. The additive effects of these two components have been shown to demonstrate long-lasting effects in various nerve blocks [25,26], especially in discogenic LBP scenarios [27]. The commonly employed routes of epidural injections include caudal, lumbar interlaminar, and transforaminal planes. While the interlaminar route is considered to deliver the drug at the site of the disc herniation, the transforaminal route is considered more specific and requires the least volume of injectate to address the root involved. The caudal epidural route although considered non-specific and requires increased usage of injectate is one of the safest and easiest procedures to address discogenic LBP. Previous studies have shown comparable efficacy of the techniques described above [1,28,29]. Despite the available evidence in the literature including systematic reviews, guidelines, health technology assessments, and medical review policies, there exists a disparity in the recommendations varying from indeterminate to strong based on the scenario where it is employed [30-33]. Further, the ideal route of epidural for a given scenario remains controversial requiring the need for ongoing trials in this regard [34]. The L4-L5 remains the commonly affected level due to discogenic LBP in both men and women followed by L5-S1 [35,36]. In unilateral discogenic LBP at L4-L5, although the transforaminal route is preferred for its selectivity and low drug volume, the criticism for the caudal epidural route remains an indirect route with large volume of drug needed [37]. Further, the clinician is not sure whether the drug ascends to reach the target level to be effective. Whereas, at the L5-S1 level, both routes have their own advantages and disadvantages. Despite the advantages noted earlier for the transforaminal route, there is an anatomical disadvantage at this level due to the lumbarization, sacralization, or lumbosacral transitional vertebrae [38,39]. Further, in the caudal epidural route despite retaining the procedural advantage, the L5-S1 level remains in close proximity to the site of injection alleviating the need for skepticism on drug ascent with the volume used. However, noted procedural complications with both routes include dural puncture, post-puncture headache, intra-venous injection, and so on [37]. Although previous studies have analyzed the efficacy of both transforaminal and caudal epidural routes in discogenic LBP,[1,28,29], none of them selectively analyzed the L5-S1 level for the given advantages and disadvantages with either of the epidural routes. This study aims to selectively analyze the efficacy and safety of transforaminal epidural steroid injection (tfESI) and caudal epidural steroid injection (cESI) for unilateral L5-S1 paracentral discogenic LBP. We hypothesize that cESI would be more advantageous than tfESI in addressing L5-S1 paracentral discogenic LBP.
The study was conducted following approval of the protocol of conduct by the Institutional Ethical Committee (KMC/IEC/2022/6-1). This is a prospective non-randomized comparative cohort study conducted in patients with unilateral radiculopathy due to paracentral L5-S1 disc disease who have been treated with cESI or tfESI between January 2023 and January 2024.
Eligibility criteria
The study enrolled adult patients >18 years of age of both sexes presenting with unilateral radiculopathy with corresponding magnetic resonance imaging confirmed paracentral L5-S1 disc disease who failed other conservative lines of management for a duration of 6 weeks. Patients with multilevel disease, bilateral radiculopathy, prior back surgery, cauda equina syndrome, back pain due to other degenerative causes involving facet or spinal canal stenosis, back pain due to spinal fractures, and back pain of neoplastic and vascular causes were excluded along with pregnant and lactating mothers.
Patient screening
All the patients who consented to participate in the study were subjected to preliminary screening for drug/dye allergy. Patients deemed fit for the procedure were enrolled in the study and their baseline numerical pain rating scale (NPRS) [40] and Oswestry disability index (ODI) scores were recorded [41].
Treatment allocation
Patients considered for inclusion into the study were sequentially allocated to either one of the two treatment groups: cESI or tfESI following written and informed consent for participation in the study. The cESI group received an injection cocktail consisting of 2 mL of triamcinolone acetonide (40 mg/mL) with 2 mL of 2% lignocaine diluted with normal saline to make 20 mL. The tfESI group received an injection cocktail consisting of 2 mL of triamcinolone acetonide (40 mg/mL) with 2 mL of 2% lignocaine diluted with normal saline to make 5 mL.
Intervention
The intervention is done in a sterile fashion in the operating room under fluoroscopy guidance. All the intervention is done by a fellowship-trained spine specialist with a trained fluoroscopy technician. The patient lies prone on the operating table with bolsters under the chest and iliac crest. The entry point for cESI is the sacral hiatus. The entry point is marked and 2 mL of lignocaine is infiltrated to anesthetize the injection site following sterile aseptic precautions. An 18G spinal needle is passed to enter the sacral canal at 45° angle in lateral view and its entry is confirmed with dye under fluoroscopy guidance as shown in Fig. 1a and b. Before injection of the drug cocktail, the needle is aspirated to check for intra-vascular or intra-dural entry. Based on the side of radiculopathy, the bevel of the needle is tilted to the affected side for preferential distribution of dye as shown in Fig. 1c. 4 mL of iohexol dye (350 mg/mL) is injected to confirm the epidural placement followed by injection. Confirmation of dye tracking till S1 root is ensured followed by injection of the drug cocktail as shown in Fig. 1d. The time taken for the procedure from the first-final fluoroscopy shots was recorded along with the number of fluoroscopy shots used.

The entry point for tfESI is based on the oblique view to visualize the Scotty-dog appearance of the vertebra after adjusting the cephalo-caudal tilt to align the endplate appropriately [39,42]. The entry point is marked visualizing the sacral foramen in the neck of the scotty-dog in the oblique view and 2 mL of lignocaine is infiltrated at the injection site under sterile aseptic precautions. A 18G spinal needle is directed to reach the foramen which is confirmed to be adjacent to the sacral canal in the lateral view. Before injection of the drug cocktail, the needle is aspirated to check for intra-vascular or intra-dural entry. 4 mL of iohexol dye (350 mg/mL) is injected to confirm the epidural placement and tracking of the S1 root followed by injection. The time taken for the procedure from the first-final fluoroscopy shots was recorded along with the number of fluoroscopy shots used.
Post-operative protocol
Patients were observed for 1 h in the observation room and discharged for review at 3 weeks, 6 weeks, and 6 months with subsequent recording of their NPRS and ODI scores. Any complications observed during the study period are recorded. Procedure failure is defined as the NPRS score improvement <50% or ODI improvement <40% at any of the follow-up time points compared to the baseline.
Statistical analysis
We presented continuous variables using mean and standard deviation and categorical variables using percentages. Improvements from the baseline were analyzed with a paired t-test, and comparisons between groups were made using one-way analysis of variance for continuous variables and Fisher-exact or Chi-square tests for categorical variables appropriately. A P-value below 0.05 was deemed statistically significant. The statistical analysis was performed with IBM SPSS Version 25 (Armonk, USA).
Characteristics of patients
We enrolled 60 patients in the study, 54 patients were available till the final follow-up with 26 patients in the cESI group and 28 patients in the tfESI group as shown in Fig. 2. The mean age of the cESI group (M: F 12:14) and tfESI group (M:F 10:18) was 36.1 (±4.1) years and 38.9 (±3.9) years, respectively. The baseline characteristics of the included patients are presented in Table 1.

Clinical outcome
The mean NPRS score of the cESI group reduced from 84.8 (±6.9) to 16.6 (±5.0) at 3 weeks and 20.3 (±9.6) at 6 weeks and 21.1 (±16.5) at 6 months, respectively. Similarly, the mean ODI score of the cESI group reduced from 82.4 (±6.8) to 28.2 (±9.1) at 3 weeks and 32.1 (±11.7) at 6 weeks and 29.3 (±24.9) at 6 months, respectively. The mean NPRS score of the tfESI group reduced from 85.3 (±6.9) to 19.6 (±8.3) at 3 weeks and 26.4 (±20.2) at 6 weeks and 26.7 (±23.2) at 6 months, respectively. Similarly, the mean ODI score of the tfESI group reduced from 85.2 (±5.5) to 29.6 (±10.3) at 3 weeks and 35.3 (±17.1) at 6 weeks and 17.2 (±33.2) at 6 months, respectively. A significant decrease in pain and ODI scores were noted following the procedure at all time points compared to the baseline for both techniques as shown in Table 2. The difference in the pain and functional score reduction between the two groups was comparable at all time points as shown in Table 3.
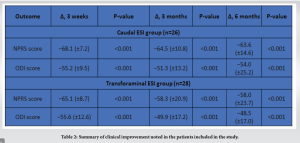

The tfESI group experienced significantly more failures (n = 8) at 6 months compared to the cESI group (n = 2) (P < 0.001). Among the 8 failures noted in the tfESI group, 5 patients (63%) had L5 sacralization while none of the 2 failures noted in the cESI group had L5 sacralized.
Further, the tfESI group had a significantly longer mean procedure time of 18.8 min compared to the cESI group with a mean procedure time of 13 min (P = 0.014). Similarly, the tfESI group used significantly more mean fluoroscopy usage of 16 shots compared to the cESI group with mean fluoroscopy usage of 10 shots (P = 0.023) as shown in Fig. 3. No major adverse events were reported for either of the procedures.

Despite the mechanical compression due to the herniated disc, chemical neuritis due to pro-inflammatory mediators triggers ectopic neuronal firing resulting in radicular pain [1,15,16]. Epidural injection of steroids and local analgesia is considered to reduce the inflammation and reverse the pain-induced neuronal plasticity [17,18]. The current study analyzed the efficacy and safety of ESI through caudal and transforaminal routes for unilateral paracentral L5-S1 discogenic pain. The main results are as follows:
- Both cESI and tfESI are efficacious in significantly reducing radicular pain and disability
- Both cESI and tfESI are comparable in their efficacy and safety
- The tfESI group had significantly longer procedural time and fluoroscopy usage compared to the cESI group
- The tfESI group experienced significantly more failures than the cESI group at 6-month follow-up.
Our study is in alignment with the previous studies that compared the efficacy and safety of the two routes of ESI in the management of LBP of various etiologies [29,43-46]. Although there were controversies about the superiority of one route over the other, their efficacy is clearly established in the literature as noted in our study. Although we noted the resurgence of pain and discomfort with ongoing follow-up, the increase in NPRS and ODI noted between the follow-up time points in both the routes was not statistically significant (P = 0.532) or clinically relevant. There has been a recent shift in the practice preference from cESI to tfESI due to the selective nature of the latter [47]. Although Ackerman et al. [48] found tfESI to be superior to the caudal and interlaminar routes, their intervention was performed mostly at the L5 level. Similarly, most of the studies comparing cESI and tfESI lack homogenous patient groups to derive meaningful conclusions for a given scenario such as L5-S1 discogenic pain [29,43-46]. Sacralization is considered a risk factor that reduces the success rate of tfESI at the L5-S1 level [49]. Although both the groups analyzed had comparable patients with sacralization as shown in Table 1, considering the procedural difficulty, the significantly increased failures noted in the tfESI group could be accounted on this confounding factor. Further, cESI is not affected either by sacralization, lumbarization, or lumbosacral transitional vertebrae and could be considered the route of choice for L5-S1 ESI for this reason. The reported complications of ESI with corticosteroids include suppression of the pituitary-adrenal axis, epidural lipomatosis, osteoporosis, steroid myopathy, avascular necrosis of bone, steroid psychosis, weight gain, fluid retention, hyperglycemia along with procedural complications such as infection, epidural hematoma, intra-vascular injection, and dural puncture [10,50-52]. However, at therapeutic dosage that is administered with ESI, with fluoroscopy guidance, complications due to both the drug and the procedure could be limited [33,53]. The commonly encountered complication with the L5-S1 tfESI is the location of the dorsal S1 foramen; likewise higher risk of intravascular uptake that prolongs the procedural time [54-56]. On the contrary, cESI is relatively safer with least risk of dural puncture, spinal cord injury, or risk of bleeding. Simon et al. [57] reported no adverse reactions among the 392 cESI and recommended its use safely even in patients on anti-thrombotic agents. Further, the risk of symptomatic hematoma is minimal due to the reduced vascularity in the sacral canal [58]. The radiation exposure that the surgeon receives with the lateral-based procedures such as tfESI was more compared to anteroposterior-based procedures such as cESI as noted in our study [59]. EC Ozturk et al. [60] conducted a similar study analyzing tfESI and cESI in S1 radiculopathy and found both routes to be beneficial and recommended cESI since it required shorter fluoroscopy time and radiation exposure. The major limitation of the study is short follow-up of 3 months. Our study noted increased failures in the tfESI group at 6-month follow-up. Further, we analyzed the impact of risk factors for failure such as sacralization between the two groups. The drug cocktail used in the above study was a mixture of 12 mg of dexamethasone, 1 mL of 0.5% bupivacaine, and 2 mL of saline amounting to 6 mL. Whereas, we used a high-volume cocktail consisting of 2 mL of triamcinolone acetonide (40 mg/mL) with 2 mL of 2% lignocaine diluted with normal saline to make 20 mL to ensure adequate drug spread. Further, high-volume blocks have been shown to demonstrate sustained benefits [61]. Although ESI has beneficial effects in the management of LBP due to discogenic back pain, their use is reserved for cases who failed a minimum 6–8 weeks of other conservative first-line management regimens because using ESI in acute sciatica <6–8 weeks for pain relief is not found to be cost-effective on a societal perspective [62]. However, before surgery, ESI could be considered as a cost-effective treatment method in the treatment regimen with comparable clinical benefits of surgery such as micro-discectomy without the risk of surgical complications [63]. The study has limitations to acknowledge. First, the small sample size and short-term follow-up limit the generalizability of the findings noted. We recommend larger randomized studies of longer follow-up to validate the findings noted in the given scenario. Second, we did not account for the frequency and dose of oral pain medications used during the follow-up period. However, the included patient cohort with S1 radiculopathy who represents greater possibility of successful management with cESI than oral analgesics makes the study design ideal and valuable. Finally, we did not collect the back and leg pain scores individually, hence the failure reported during the follow-up could not delineated to either residual radiculopathy not addressed by the ESI or axial pain following resolution of radiculopathy.
cESI is a simple, safe, and efficacious technique comparable to tfESI in the management of unilateral L5-S1 paracentral discogenic radicular pain with significantly less procedural time and fluoroscopy usage. Further, large-scale studies are needed to validate the study results.
- Both cESI and tfESI result in significant pain and functional improvement in patients with unilateral L5-S1 paracentral discogenic radicular pain
- The tfESI group experienced significantly more failures compared to the cESI group
- The tfESI group had significantly longer mean procedure time and more fluoroscopy usage compared to cESI group and fluoroscopy usage
- No major adverse events were reported for either of the groups
References
- 1.Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, Abdi S, et al. Interventional techniques: Evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician 2007;10:7-111. [Google Scholar | PubMed]
- 2.World Health Organization. WHO Guidelines on Chronic Low Back Pain Management. Geneva, Switzerland: World Health Organization; 2023. [Google Scholar | PubMed]
- 3.Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: A World Health Organization study in primary care. JAMA 1998;280:147-51. [Google Scholar | PubMed]
- 4.Hu Y, Ma J, Chen B, Pang J, Liang W, Wu W. The duration of chronic pain can affect brain functional changes of the pain matrix in patients with chronic back pain: A resting-state fMRI study. J Pain Res 2024;17:1941-51. [Google Scholar | PubMed]
- 5.Hoy D, March L, Brooks P, Woolf A, Blyth F, Vos T, et al. Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol 2010;24:155-65. [Google Scholar | PubMed]
- 6.GBD 2021 Diseases and Injuries Collaborators. Global Incidence, Prevalence, Years Lived with Disability (YLDs), Disability-Adjusted Life-Years (DALYs), and Healthy Life Expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: A systematic analysis for the global burden of disease study 2021. Lancet 2024;403:2133-61. [Google Scholar | PubMed]
- 7.Rudy TE, Weiner DK, Lieber SJ, Slaboda J, Boston JR. The impact of chronic low back pain on older adults. Pain 2007;131:293-301. [Google Scholar | PubMed]
- 8.World Health Organization. WHO Guideline for Non-Surgical Management of Chronic Primary Low Back Pain in Adults in Primary and Community Care Settings. Geneva, Switzerland: World Health Organization; 2023. [Google Scholar | PubMed]
- 9.Kuslich SD, Ulstrom CL, Michael CJ. The tissue origin of low back pain and sciatica: A report of pain response to tissue stimulation during operations on the lumbar spine using local anesthesia. Orthop Clin North Am 1991;22:181-7. [Google Scholar | PubMed]
- 10.Manchikanti L, Singh V, Pampati V, Damron KS, Barnhill RC, Beyer C, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician 2001;4:308-16. [Google Scholar | PubMed]
- 11.Genevay S, Finckh A, Payer M, Mezin F, Tessitore E, Gabay C, et al. Elevated levels of tumor necrosis factor-alpha in periradicular fat tissue in patients with radiculopathy from herniated disc. Spine (Phila Pa 1976) 2008;33:2041-6. [Google Scholar | PubMed]
- 12.Wu L, Munakomi S, Cruz R. Lumbar spinal stenosis. In StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. [Google Scholar | PubMed]
- 13.Zhang X, Wang X, Gao L, Yang B, Wang Y, Niu K, et al. TNF-ɑ induces methylglyoxal accumulation in lumbar herniated disc of patients with radicular pain. Front Behav Neurosci 2021;15:760547. [Google Scholar | PubMed]
- 14.Conn A, Buenaventura RM, Datta S, Abdi S, Diwan S. Systematic review of caudal epidural injections in the management of chronic low back pain. Pain Physician 2009;12:109-35. [Google Scholar | PubMed]
- 15.Kushnerik V, Altman G, Gozenput P. Pharmacology of steroids used during epidural steroid injections. Tech Reg Anesth Pain Manage 2009;13:212-6. [Google Scholar | PubMed]
- 16.Manchikanti L. Role of neuraxial steroids in interventional pain management. Pain Physician 2002;5:182-99. [Google Scholar | PubMed]
- 17.Byröd G, Otani K, Brisby H, Rydevik B, Olmarker K. Methylprednisolone reduces the early vascular permeability increase in spinal nerve roots induced by epidural nucleus pulposus application. J Orthop Res 2000;18:983-7. [Google Scholar | PubMed]
- 18.Lundin A, Magnuson A, Axelsson K, Nilsson O, Samuelsson L. Corticosteroids peroperatively diminishes damage to the C-Fibers in microscopic lumbar disc surgery. Spine (Phila Pa 1976) 2005;30:2362-7; discussion 2368. [Google Scholar | PubMed]
- 19.Mao J, Chen LL. Systemic lidocaine for neuropathic pain relief. Pain 2000;87:7-17. [Google Scholar | PubMed]
- 20.Pasqualucci A, Varrassi G, Braschi A, Peduto VA, Brunelli A, Marinangeli F, et al. Epidural local anesthetic plus corticosteroid for the treatment of cervical brachial radicular pain: Single injection versus continuous infusion. Clin J Pain 2007;23:551-7. [Google Scholar | PubMed]
- 21.Lavoie PA, Khazen T, Filion PR. Mechanisms of the inhibition of fast axonal transport by local anesthetics. Neuropharmacology 1989;28:175-81. [Google Scholar | PubMed]
- 22.Bisby MA. Inhibition of axonal transport in nerves chronically treated with local anesthetics. Exp Neurol 1975;47:481-9. [Google Scholar | PubMed]
- 23.Melzack R, Coderre TJ, Katz J, Vaccarino AL. Central neuroplasticity and pathological pain. Ann N Y Acad Sci 2001;933:157-74. [Google Scholar | PubMed]
- 24.Cassuto J, Sinclair R, Bonderovic M. Anti-inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaesthesiol Scand 2006;50:265-82. [Google Scholar | PubMed]
- 25.Sato C, Sakai A, Ikeda Y, Suzuki H, Sakamoto A. The prolonged analgesic effect of epidural ropivacaine in a rat model of neuropathic pain. Anesth Analg 2008;106:313-20. [Google Scholar | PubMed]
- 26.Tachihara H, Sekiguchi M, Kikuchi S, Konno S. Do Corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation? Spine (Phila Pa 1976) 2008;33:743-7. [Google Scholar | PubMed]
- 27.Manchikanti L, Nampiaparampil DE, Manchikanti KN, Falco FJ, Singh V, Benyamin RM, et al. Comparison of the efficacy of saline, local anesthetics, and steroids in epidural and facet joint injections for the management of spinal pain: A systematic review of randomized controlled trials. Surg Neurol Int 2015;6:S194-235. [Google Scholar | PubMed]
- 28.Abdi S, Datta S, Trescot AM, Schultz DM, Adlaka R, Atluri SL, et al. Epidural steroids in the management of chronic spinal pain: A systematic review. Pain Physician 2007;10:185-212. [Google Scholar | PubMed]
- 29.Singh S, Kumar S, Chahal G, Verma R. Selective nerve root blocks vs. Caudal epidural injection for single level prolapsed lumbar intervertebral disc - A prospective randomized study. J Clin Orthop Trauma 2017;8:142-7. [Google Scholar | PubMed]
- 30.Oliveira CB, Maher CG, Ferreira ML, Hancock MJ, Oliveira VC, McLachlan AJ, et al. Epidural corticosteroid injections for lumbosacral radicular pain. Cochrane Database Syst Rev 2020;4:CD013577. [Google Scholar | PubMed]
- 31.Manchikanti L, Singh V, Derby R, Schultz DM, Benyamin RM, Prager JP, et al. Reassessment of evidence synthesis of occupational medicine practice guidelines for interventional pain management. Pain Physician 2008;11:393-482. [Google Scholar | PubMed]
- 32.Armon C, Argoff CE, Samuels J, Backonja MM, Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Assessment: Use of epidural steroid injections to treat radicular lumbosacral pain: Report of the therapeutics and technology assessment subcommittee of the American Academy of Neurology. Neurology 2007;68:723-9. [Google Scholar | PubMed]
- 33.Manchikanti L, Knezevic NN, Navani A, Christo PJ, Limerick G, Calodney AK, et al. Epidural interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) comprehensive evidence-based guidelines. Pain Physician 2021;24:S27-208. [Google Scholar | PubMed]
- 34.Osman A, Hu W, Jianhua-Sun, Li J, Luo X, Han N, et al. Caudal epidural steroid injections versus selective nerve root blocks for single-level lumbar spinal stenosis: A study protocol for a randomized controlled trial. Trials 2021;22:524. [Google Scholar | PubMed]
- 35.Teraguchi M, Yoshimura N, Hashizume H, Muraki S, Yamada H, Minamide A, et al. Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: The Wakayama spine study. Osteoarthritis Cartilage 2014;22:104-10. [Google Scholar | PubMed]
- 36.Schliessbach J, Siegenthaler A, Heini P, Bogduk N, Curatolo M. Blockade of the sinuvertebral nerve for the diagnosis of lumbar diskogenic pain: An exploratory study. Anesth Analg 2010;111:204-6. [Google Scholar | PubMed]
- 37.Andreisek G, Jenni M, Klingler D, Wertli M, Elliott M, Ulbrich EJ, et al. Access routes and reported decision criteria for lumbar epidural drug injections: A systematic literature review. Skeletal Radiol 2013;42:1683-92. [Google Scholar | PubMed]
- 38.Konin GP, Walz DM. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol 2010;31:1778-6. [Google Scholar | PubMed]
- 39.Kanna RM, Shetty AP, Rajasekaran S. Predictors of successful outcomes of selective nerve root blocks for acute lumbar disc herniation. Global Spine J 2019;9:473-9. [Google Scholar | PubMed]
- 40.Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005;30:1331-4. [Google Scholar | PubMed]
- 41.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy 1980;66:271-3. [Google Scholar | PubMed]
- 42.Kang RA, Sim WS, Choi JW, Kang S, Lee S, Jee HS, et al. Comparison between anteroposterior and oblique “Scotty Dog” approach during S1 transforaminal epidural steroid injection: A randomized controlled trial. Medicine (Baltimore) 2020;99:e22895. [Google Scholar | PubMed]
- 43.Manchikanti L, Singh V, Pampati V, Falco FJ, Hirsch JA. Comparison of the efficacy of caudal, interlaminar, and transforaminal epidural injections in managing lumbar disc herniation: Is one method superior to the other? Korean J Pain 2015;28:11-21. [Google Scholar | PubMed]
- 44.Parr AT, Manchikanti L, Hameed H, Conn A, Manchikanti KN, Benyamin RM, et al. Caudal epidural injections in the management of chronic low back pain: A systematic appraisal of the literature. Pain Physician 2012;15:E159-98. [Google Scholar | PubMed]
- 45.Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Effect of fluoroscopically guided caudal epidural steroid or local anesthetic injections in the treatment of lumbar disc herniation and radiculitis: A randomized, controlled, double blind trial with a two-year follow-up. Pain Physician 2012;15:273-86. [Google Scholar | PubMed]
- 46.Manchikanti L, Pampati V, Benyamin RM, Boswell MV. Analysis of efficacy differences between caudal and lumbar interlaminar epidural injections in chronic lumbar axial discogenic pain: Local anesthetic alone vs. local combined with steroids. Int J Med Sci 2015;12:214-22. [Google Scholar | PubMed]
- 47.Helm Ii S, Harmon PC, Noe C, Calodney AK, Abd-Elsayed A, Knezevic NN, et al. Transforaminal epidural steroid injections: A systematic review and meta-analysis of efficacy and safety. Pain Physician 2021;24:S209-32. [Google Scholar | PubMed]
- 48.Ackerman WE, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg 2007;104:1217-22. [Google Scholar | PubMed]
- 49.Sencan S, Azizov S, Celenlioglu AE, Bilim S, Gunduz OH. Effect of sacralization on the success of lumbar transforaminal epidural steroid injection treatment: Prospective clinical trial. Skeletal Radiol 2023;52:1949-57. [Google Scholar | PubMed]
- 50.Stitz MY, Sommer HM. Accuracy of blind versus fluoroscopically guided caudal epidural injection. Spine (Phila Pa 1976) 1999;24:1371-6. [Google Scholar | PubMed]
- 51.Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Hanna A, Rittenberg J, et al. Complications of fluoroscopically guided caudal epidural injections. Am J Phys Med Rehabil 2001;80:416-24. [Google Scholar | PubMed]
- 52.Fogel GR, Cunningham PY, Esses SI. Spinal epidural lipomatosis: Case reports, literature review and meta-analysis. Spine J 2005;5:202-11. [Google Scholar | PubMed]
- 53.Park CH, Jang YH, Lee SH. Comparison of pain reduction and changes in serum cortisol and glucose levels to different doses of lumbar epidural dexamethasone: A prospective study. Pain Physician 2022;25:E1081-5. [Google Scholar | PubMed]
- 54.Chang A, Ng AT. Complications associated with lumbar transforaminal epidural steroid injections. Curr Pain Headache Rep 2020;24:67. [Google Scholar | PubMed]
- 55.Park SJ, Kim SH, Kim SJ, Yoon DM, Yoon KB. Comparison of incidences of intravascular injection between medial and lateral side approaches during traditional S1 transforaminal epidural steroid injection. Pain Res Manag 2017;2017:6426802. [Google Scholar | PubMed]
- 56.Hong J, Kim JS, Lee YH. Comparison of intravascular injection incidences and technical easiness between anteroposterior and oblique approaches during S1 transforaminal epidural injection. Pain Physician 2021;24:E1129-35. [Google Scholar | PubMed]
- 57.Simon JI, Gehret J, Larsen ES, Hummerston KS, Koehler Iii PJ, Kitei PM. Caudal epidural steroid injections in the setting of remaining on antithrombotics: A retrospective study. Pain Physician 2021;24:E821-8. [Google Scholar | PubMed]
- 58.Liu J, Zhou H, Lu L, Li X, Jia J, Shi Z, et al. The effectiveness of transforaminal versus caudal routes for epidural steroid injections in managing lumbosacral radicular pain. Medicine (Baltimore) 2016;95:e3373. [Google Scholar | PubMed]
- 59.Yoo SH, Kim WJ, Jue MJ, Lee MJ. Comparison of radiation exposure to physicians between anteroposterior and lateral real-time fluoroscopy when performing lumbar transforaminal epidural steroid injections: A randomized controlled trial. Medicine (Baltimore) 2022;101:e29684. [Google Scholar | PubMed]
- 60.Ozturk EC, Sacaklidir R, Sencan S, Gunduz OH. Caudal epidural steroid injection versus transforaminal ESI for unilateral S1 radiculopathy: A prospective, randomized trial. Pain Med 2023;24:957-62. [Google Scholar | PubMed]
- 61.Chae JS, Kim WJ, Choi SH. Effects of local anesthetics with or without steroids in high-volume transforaminal epidural blocks for lumbar disc herniation: A randomized, double-blind, controlled trial. J Korean Med Sci 2022;37:e137. [Google Scholar | PubMed]
- 62.Ter Meulen BC, Maas ET, van der Vegt R, Haumann J, Weinstein HC, Ostelo RW, et al. Cost-effectiveness of transforaminal epidural steroid injections for patients with ACUTE sciatica: A randomized controlled trial. BMC Musculoskelet Disord 2024;25:247. [Google Scholar | PubMed]
- 63.Wilby MJ, Best A, Wood E, Burnside G, Bedson E, Short H, et al. Microdiscectomy compared with transforaminal epidural steroid injection for persistent radicular pain caused by prolapsed intervertebral disc: The NERVES RCT. Health Technol Assess 2021;25:1-86. [Google Scholar | PubMed]









