This case highlights the complex challenges of managing long-term complications in patients with multiple hip arthroplasty revisions, emphasizing the need for an adaptable surgical approach and the impact of external factors like the COVID-19 pandemic on patient outcomes
Dr. Navdeep Singh Keer, Central Institute of Orthopaedics, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi - 110029, India. E-mail: drnavdeepsinghkeer@gmail.com
Introduction: Avascular necrosis (AVN) of the femoral head and its subsequent management through total hip arthroplasty (THA) remains a significant challenge in orthopedic surgery, especially in cases with long-term complications. This case report is crucial as it documents the unprecedented journey of a 69-year-old female patient who underwent multiple revision surgeries over three decades, culminating in a complex surgical intervention during the COVID-19 pandemic. To the best of our knowledge, only a handful of cases have been reported in the literature that explores the compounded effects of delayed surgical intervention due to a global pandemic on a patient with a history of multiple hip arthroplasty revisions.
Case Report: The patient, a 69-year-old female, initially presented with AVN of the left femoral head in 1994, for which she underwent an isoelastic cemented total hip replacement. Over the years, she required two revision surgeries due to implant loosening. In 2021, she presented with a dislocated femoral head and loosening of the cemented acetabular cup. The COVID-19 pandemic delayed operative intervention, leading to worsening complications, including proximal migration of the dislocated components. In 2022, a complex surgical procedure was performed, involving acetabular defect reconstruction and femoral shortening osteotomy, with the implantation of a new prosthetic body and a bipolar head. The surgery successfully restored hip stability, allowing the patient to walk with reduced risk of further complications.
Conclusion: This case underscores the complexities of managing long-term complications in patients with a history of multiple revision hip arthroplasties, particularly when external factors like the COVID-19 pandemic delay necessary interventions. The successful outcome of the case highlights the importance of personalized treatment strategies and adaptive surgical approaches in addressing severe complications. This case provides valuable insights for orthopedic surgeons and may have broader implications for managing similar cases in the future, especially in scenarios where timely surgical intervention is compromised by external challenges.
Keywords: Avascular necrosis, total hip arthroplasty, revision hip arthroplasty, COVID-19, orthopedic surgery.
This case report discusses the intricate and multifaceted case of a 69-year-old female patient who endured a series of complications following avascular necrosis (AVN) of the left femoral head for which primary total hip arthroplasty (THA) was done 30 years ago. The management of her condition involved multiple surgical interventions, each presenting its own set of challenges, compounded by the unprecedented circumstances of the COVID-19 pandemic. This report aims to provide a comprehensive overview of the patient’s clinical history, the management strategies employed, the outcomes, and the broader implications for clinical practice.
Clinical history
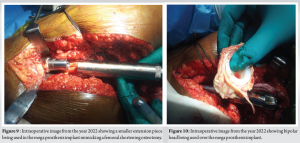
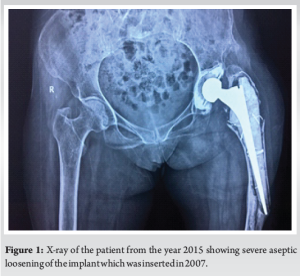
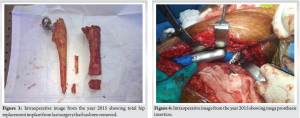
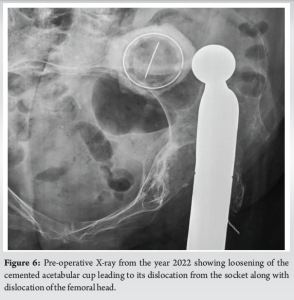
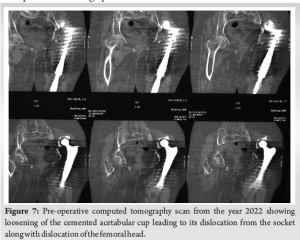
In 1994, the patient, then experiencing significant symptoms from AVN of the left femoral head, underwent an isoelastic cemented total hip replacement. Over time, the implant loosened, necessitating a revision cemented THA in 2007. Unfortunately, this intervention did not prevent further complications; by 2015, the revised implant exhibited severe aseptic loosening and proximal femoral bone loss (Fig. 1). During the second revision surgery in 2015, it was discovered that the proximal femur could not be salvaged even with intraoperative impaction bone grafting. Given that the cemented acetabular cup remained well-fixed, only proximal femoral resection was performed, and a tumor mega-prosthesis was applied to restore hip joint stability (Fig. 2-4). The patient remained under follow-up until 2019, during which she walked comfortably without support. In 2021, the patient presented with a new complication that is loosening and dislocation of the cemented acetabular cup as well as dislocation of the femoral head. Due to the constraints imposed by the COVID-19 pandemic, no operative intervention was immediately feasible, resulting in the patient walking with a dislocated hip. This led to proximal migration of the dislocated cup and femoral head over the ilium bone (Fig. 5-7).


Management
In September 2022, after prognosticating the patient regarding her general health, risks associated with operative intervention, potential for dislocation of the implant, the presence of more than 10 cm of shortening along with tissue contractures, and a possible underlying abductor insufficiency, a surgical intervention was planned. Intra-operatively, a posterior acetabular defect (Paprosky type IIIA) was noted, which was reconstructed using tri-cortical bone grafting and a reconstruction plate (Fig. 8). On the femoral side, the cemented stem piece of the mega-prosthesis remained well-fixed in the cement mantle and thus was not changed. The extension piece of 70 mm was reduced to 20 mm, effectively performing a femoral shortening osteotomy (Fig. 9), which made the hip joint reducible. A new prosthetic body was then implanted over the extension piece, and a bipolar head was fitted (Fig. 10), allowing for the hip to be reduced. This choice was made to provide better stability considering the weak abductors and reduce operative time, which was crucial given the patient’s general health. The challenges faced in this case were related to the general health of the patient due to her age, long-standing dislocation of the femoral component and the patient walking with it making it difficult to reduce the hip joint, expected femoral and acetabular bone loss and future stability of the hip joint.
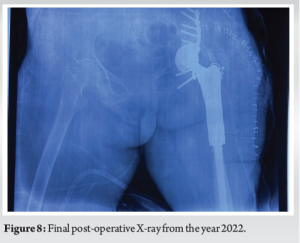
Following the surgery, the patient experienced improved hip stability and was able to walk with a reduced risk of further complications. The use of a bipolar head, while unconventional in some scenarios, proved beneficial in this case due to its stability and the decreased operative time required.
This case highlights the complexities inherent in managing long-term complications of total hip replacement, particularly in patients with a history of revision surgery. Research indicates that achieving stable acetabular fixation during revision THA in patients with a non-supportive superior dome and proximal migration of the acetabular component (Paprosky type III A defect) is unreliable when using only a hemispherical porous-coated component. A significant failure rate has been observed when such components are implanted without the addition of structural grafts. This elevated failure rate is thought to result from inadequate superior dome support, leading to component micro-motion and/or superolateral migration [1]. Thus, to restore the bone stock, tri-cortical iliac crest bone grafting was done and a reconstruction plate was applied since, autografts are superior to allografts with respect to their incorporation capacity [2]. Literature suggests that proximal displacement of the femoral head results in laxity and weakening of the abductor muscles, which can lead to early fatigue and insufficiency [3]. Treating patients with high hip dislocations presents numerous challenges and may require different surgical approaches based on individual cases. The new center of rotation (COR) established after cup placement plays a crucial role in determining hip biomechanics, leg length, and femoral reconstruction. If the cup is placed in the pseudo-acetabulum, it can result in high dislocation rates, persistent limping, and increased component loosening. Therefore, it is essential to restore the new COR as close as possible to the true acetabulum, ideally within 1 cm of the anatomical hip center, to reduce hip contact stresses. In addition, shortening of the femur may be necessary to facilitate the reduction of the prosthetic hip joint [4-6]. In this case, since the cemented stem piece of the mega-prosthesis remained well-fixed in the cement mantle, thus was not changed but, the extension piece of 70 mm was reduced to 20 mm, effectively performing a femoral shortening osteotomy to aid in the reduction of the hip joint. Research indicates that bipolar prostheses can be beneficial in cases of recurrent dislocation following THA. This is because movement occurs at two bearing surfaces, allowing for a greater range of motion that can prevent the head from dislodging from the acetabulum. In addition, the bipolar head is larger than a standard total hip femoral component, meaning that a greater volume needs to be displaced from the acetabulum for a dislocation to occur [7, 8]. Thus, a bipolar head was used in our case after the dislocation of the implant to reduce the risk of dislocation in the future, provide better stability considering the weak abductors and reduce the operative time, which was crucial given the patient’s age and general health.
The patient’s journey underscores the importance of continuous monitoring and the need for flexible, patient-tailored treatment plans. The impact of the COVID-19 pandemic on patient care is also evident, with delayed interventions leading to exacerbated complications. In the United States, a retrospective analysis of revision knee and hip arthroplasties was performed in a healthcare system containing 5 hospitals in a time period of 8 months before and 8 months after the cessation of elective surgeries. It was found that there had been a 30.1% decrease in revision TKA and a 6.80% decrease in revision THA during that period alone [9, 10]. Thus, emphasis should be laid on the necessity for healthcare systems to develop alternative strategies to ensure ongoing patient management during such unprecedented times.
The presented case illustrates the unpredictable and challenging nature of hip arthroplasty revisions. It underscores the importance of personalized treatment approaches and continuous follow-up to optimize patient outcomes, and the need to develop alternative strategies in the face of external challenges such as a global pandemic so that patient care is not hindered.
The clinical message of the case report is that managing long-term complications in patients with a history of multiple hip arthroplasty revisions requires adaptable, patient-centric surgical approaches, particularly in the face of external challenges like the COVID-19 pandemic, which can delay essential interventions and worsen patient outcomes. Continuous monitoring and personalized care are crucial to optimize outcomes in such complex cases.
References
- 1.Shon WY, Santhanam SS, Choi JW. Acetabular reconstruction in total hip arthroplasty. Hip Pelvis 2016;28:1-4. [Google Scholar]
- 2.Mancino F, Cacciola G, Di Matteo V, De Marco D, Greenberg A, Perisano C, et al. Reconstruction options and outcomes for acetabular bone loss in revision hip arthroplasty. Orthop Rev 2020;12:8655. [Google Scholar]
- 3.Siwach I, Krishna LG, Talwar J, Rustagi A, Keer NS. Clinical outcomes of post-surgery osteoporosis treatment in elderly intertrochanteric fracture patients: a prospective study . Int J Res Orthop [Internet]. 2024 Oct. 25 [cited 2025 Jan. 15];10(6):1284-9. [Google Scholar]
- 4.Talwar J, Agarwal S, Agarwal S, Krishna LG, Rustagi A. Step-cut subtrochanteric osteotomy combined with total hip arthroplasty for neglected traumatic hip dislocations. Clin Orthop Surg 2022;14:205. [Google Scholar]
- 5.Hartofilakidis G, Stamos K, Karachalios T. Treatment of high dislocation of the hip in adults with total hip arthroplasty. Operative technique and long-term clinical results. J Bone Joint Surg Am 1998;80:510-7. [Google Scholar]
- 6.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: An analysis of risk factors and treatment options. J Bone Joint Surg Am 2002;84:1788-92. [Google Scholar]
- 7.Ries MD, Wiedel JD. Bipolar hip arthroplasty for recurrent dislocation after total hip arthroplasty. Clin Orthop Relat Res 1992;278:121-7. [Google Scholar]
- 8.Takatori Y, Ninomiya S, Umeyama T, Yamamoto M, Moro T, Nakamura K. Bipolar revision arthroplasty for failed threaded acetabular components: Radiographic evaluation of cup migration. J Orthop Sci 2002;7:467-71. [Google Scholar]
- 9.Rizkalla JM, Gladnick BP, Bhimani AA, Wood DS, Kitziger KJ, Peters PC. Triaging total hip arthroplasty during the COVID-19 pandemic. Curr Rev Musculoskelet Med 2020;13:416-24. [Google Scholar]
- 10.Wilson JM, Schwartz AM, Farley KX, Roberson JR, Bradbury TL, Guild GN 3rd. Quantifying the backlog of total hip and knee arthroplasty cases: Predicting the impact of COVID-19. HSS J 2020;16:85-91. [Google Scholar]