The management of individuals with Maffucci syndrome requires a comprehensive approach that includes meticulous surgical planning and routine screening for associated conditions.
Dr. Amit Kumar Yadav, Department of Orthopaedics Wrightington Hospital, Wigan, UK. E-mail: amit_aur09@yahoo.com
Introduction: Maffucci syndrome (MS) is a rare disorder with enchondromatosis associated with multiple hemangiomas in soft tissue and internal organs. Enchondromas in the long bone lead to limb length discrepancy, deformity, and pathological fractures that usually need corrective osteotomies and limb lengthening.
Case Report: A female in her late adolescence with MS presented with significant varus deformity of the distal femur and left lower limb shortening of 11.5 cm. She underwent an acute correction of the varus with a distal femur osteotomy and gradual femoral lengthening using a monolateral fixator. She sustained a pathological fracture through the regenerate, needing an intramedullary nail stabilisation during follow-up. At a 2-year follow-up, the patient was left with a residual shortening of 5 cm, corrected with a shoe raise. She could walk full weight bearing and independently with her day-to-day activities and function.
Conclusion: MS can present with significant limb length discrepancy and angular deformities. This case aims to inform clinicians of the diagnosis and management of this rare condition and highlight the importance of regular follow-up after complex surgery, and the impact coronavirus disease-19 lockdowns had on the inability of patients to do so.
Keywords: Limb lengthening, Maffucci syndrome, deformity correction.
Maffucci syndrome (MS) is a rare non-hereditary disorder characterised by multiple enchondromatosis associated with several hemangiomas in soft tissue and internal organs [1]. There are <200 cases reported to date since its first-ever description by Angelo Maffucci in 1881 [2]. Ollier’s disease (OD) is a similar condition of multiple enchondromatosis without soft-tissue involvement. MS is due to a somatic gain of function mutation in the isocitrate dehydrogenase 1 (IDH1 and IDH2) genes located on chromosome 2q34 [3]. These patients are at increased risk of brain and abdominal malignancies and secondary chondrosarcoma. In a multicenter European study on 144 Olliers and 17 MS patients, classifying them into three groups based on affection of hands and feet, long bones, and pelvis, and a combination of the two, found the risk of Chondrosarcoma to be 43% and 46% in Group 2 and 3, respectively [4]. The presence of pelvic enchondromatosis significantly increased the risks of malignancy (odds ratio 3.8). Enchondromas in the long bones of the lower limb led to limb length discrepancy, deformity, and pathological fractures that usually required correction with osteotomies and limb lengthening. While the natural history of these is better known in OD, the scarcity of reports of MS makes limb-lengthening procedures unpredictable [5].
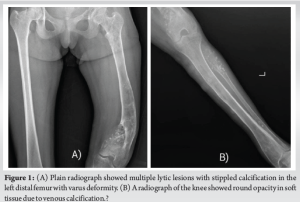
A female in her late adolescence presented with painless progressive deformity and shortening of the left lower limb, ongoing for several years. On examination, multiple reddish pea-sized soft lumps were seen over the left lower limb and the trunk. There was a significant true shortening of 11.5 cm of the left lower limb, along with genu varum deformity arising primarily from the distal femur. The knee range of motion (ROM) was limited to 60° flexion. There was no neurovascular deficit and asymmetric involvement of the left upper limb with lesions but no deformity. The plain radiograph showed multiple lytic lesions with stippled calcification in the left distal femur (Fig. 1a) and multiple rounded opacity in soft tissue due to venous calcification (Fig. 1b). A Scannogram of both lower limbs showed distal femur varus deformity and shortening of 8 cm in the femur and 3.5 cm in the tibia. Magnetic resonance imaging (MRI) showed multiple well-defined lesions in the left femur, tibia, and fibula, predominantly in the meta-diaphyseal region. The lesions were hyperintense on T2-weighted images, isointense on T1-weighted images, and showed heterogonous post-contrast enhancement.
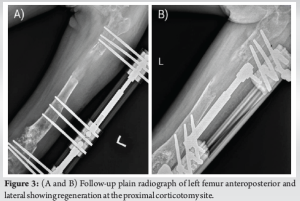
The patient was discussed in a multidisciplinary treatment meeting involving a musculoskeletal radiologist, a pediatric orthopedic surgeon, and a limb reconstruction surgeon. The diagnosis of MS was based on clinical and radiological appearances; however, a confirmatory biopsy was performed for the bony lesion in the distal femur using a bone biopsy needle and an open excision biopsy of one of the subcutaneous soft-tissue lesions from the lower leg. Enchondromatosis involving the metaphyseal region of long bones might lead to deformity in either coronal/sagittal plane or be associated with significant limb length discrepancy. Solitary enchondromas are not uncommon, but multiple enchondromatosis is usually associated with either Ollier’s or Maffucci’s syndrome. MS can be differentiated from Olliers disease by the presence of multiple cavernous hemangiomas associated with enchondromatosis. No other differential diagnosis was considered. The patient underwent a distal femur lateral closing wedge osteotomy for varus correction along with proximal femur corticotomy and application of a monolateral external fixator spanning the entire femur Limb reconstruction system (LRS) (Fig. 2). Gradual distraction at a rate of one mm/day was commenced on day seven and continued for 65 days. Follow-up radiographs of the left femur could only be obtained at 5 months as the patient belonged to a remote rural location, and this showed reasonable regeneration at the proximal corticotomy site (Fig. 3a and b). The patient was subsequently lost to follow-up due to coronavirus disease-19 (COVID-19) pandemic, causing significant restrictions of movements with strict lockdowns, fear of contracting COVID, and lack of access to public transport for the patient to travel to our center. She got her fixator removed at a local hospital at 7 months postoperatively without adequate surveillance of regenerate quality.

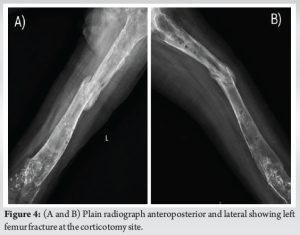
Eleven months after the index surgery, the patient presented with pain in mid-thigh and inability to bear weight on the leg, which had been an ongoing issue for over 2 months. A plain radiograph showed a fracture through the consolidate site in the left femur (Fig. 4a and b). The Patient was also diagnosed with a granulosa cell tumor of the ovary in the interim, confirmed on biopsy and managed later with chemoradiotherapy. The femur fracture was treated with open reduction and intramedullary interlock nail (9 mm × 360 mm, S.H. PITKAR.). Had the patient presented to us for follow-up as expected, we would have perhaps added a prophylactic intramedullary nail at the time of fixator removal if there was any doubt about the consolidation of the regeneration.
The fracture healed 6 months post-surgery (Fig. 5a and b). The patient had a residual shortening of 5 cm, which was compensated with a shoe raise. At the final follow-up (2 years following the index surgery), the patient was fully weight-bearing and used a walking aid when traveling long distances. She was able to carry out all her activities of daily living independently. At the last follow-up with us, the patient completed treatment for her ovarian tumor.

MS was first reported in 1881 and is characterized by multiple enchondromatosis associated with numerous cavernous hemangiomas [1]. MS presents with multiple subcutaneous vascular swellings, joint deformity, limb length discrepancy, scoliosis, and pathological fractures [6]. Enchondromas usually affect one side of the body in 46% of patients, and the upper limb is more commonly affected than the lower limb. The most common location of enchondroma is the femur, followed by the tibia, humerus, and pelvis [7]. Enchondromas in the metaphyseal region of long bones result in deformities and limb asymmetry. MS should be differentiated from Ollier disease (OD), characterized by enchondromatosis alone. Both are attributed to somatic mutations of IDH 1 or 2. MS and OD are isolated cases with no familial history and germline variants reported to date. Malignancies such as chondrosarcoma, glioma, astrocytoma, granulosa cell tumor of the ovary, liver adenocarcinoma, acute myeloid leukemia, and chronic myeloid leukemia have been reported in the literature.[7]. A whole-body MRI at diagnosis is recommended to screen the brain, abdomen, and pelvis for malignancy [4,6]. The rate of malignant transformation of enchondromas to chondrosarcomas is highly variable in patients with MS, ranging from 52% to 57.1%, much higher than OD [4,8]. Surgery is the only treatment for complications like oversized enchondromas, limb length discrepancy, and deformity correction. Märtson et al. reported a case of limb length discrepancy in OD, which was 22 cm in the femur and 10 cm in the tibia, corrected with Ilizarov fixator in a 14-year-old male [9]. Pandey et al. stated that distraction osteogenesis through predominantly cartilaginous nests of enchondroma converted rapidly into mature corticalized bone with no evidence of delayed healing of regenerate [10]. Madan et al. reported ten patients who had lengthened and corrected deformities with the external fixator in OD [5]. The mean age of the patients was 10.7 years, with lengthening of 42.3 mm and 164.8 days with external fixation and a minimum follow-up of 2 years. The healing index was 32.5 days/cm. According to their observation, there is a tendency for corticotomy to unite prematurely, so distraction should be started early and at a faster rate, thus proving that the bone with enchondroma has a normal osteogenic capacity and good healing potential. In our case, the lengthening was 65 mm, and the external fixator was removed after 210 days. Madan et al. started distraction early on 4–5 days, whereas we started distractions on the 7th day. Our case had delayed regeneration healing and a fracture that needed intra-medullary stabilization. Verma et al. reported a left-side genu valgus deformity in a 12-year-old girl with MS, which was treated with supracondylar osteotomy and reported a good clinical outcome [11]. However, their patient had no limb lengthening, hence none of the complications associated with an external fixator or regenerate consolidation. A Recent systematic review concluded that there’s no clear consensus regarding the ideal surgical technique and choice of implants for the management of limb deformities in patients with enchondromatosis. An external fixator is preferred to correct these deformities gradually but comes with an overall complication rate of 27.9% [12]. Very few case reports have managed the deformity in such patients rather than described the diagnostic criteria. This case report highlights the management of femoral deformity in a patient with MS on the broad principles of deformity correction. Limb length discrepancy associated with angular deformity is one of the presenting features of this condition. The treatment modalities of deformity correction and limb lengthening can be broadly divided into two categories – (1) using an external fixator and (2) using internal fixation methods. There are different forms of external fixators, each having its pros and cons; the author’s preferred modality was to use a mono-lateral external fixator (LRS) due to familiarity and less complexity in using this technique. Internal devices such as motorized nails and other implantable devices are available in the market, which have their advantages, but the main limitation is cost. Hence, we preferred to use the LRS system [13]. The two common complications of using an external fixator for limb lengthening are pin-tract site infection ± loosening and regenerate fracture. The authors pragmatically dealt with the later complications described in the manuscript. We were fortunate in this case as there were no concerns for pin-tract infection. The regenerate fracture has definitely affected the final result, or else we would have achieved better correction for this LLD, but considering the above-mentioned circumstances, the remnant of 5 cm of shortening was accepted. The evidence is clear that bone healing is usually not an issue in patients with enchondromatosis; the most logical explanation that the authors could give for this complication might be the premature removal of the external fixator with a lack of appropriate follow-up due to the pandemic lockdown. The patient eventually mobilized fully weight-bearing with minimal limping due to residual shortening, which was not the case during the first presentation. The knee ROM slightly improved, and the patient could flex up to 80° without discomfort. After a thorough review of the literature, there is no consensus on the definitive treatment in these patients, but this case report highlights treatment of limb-length discrepancy and deformity in patients with MS with acceptable outcomes based on formal deformity correction principles. This report also describes one of the complications while considering limb lengthening in such patients and the authors’ preferred rescue method in that situation.
The management of individuals with MS requires a comprehensive approach that includes meticulous surgical planning and routine screening for associated conditions. Addressing the challenges posed by the COVID-19 pandemic is crucial to ensure that patients receive timely and adequate care, particularly those in remote areas. Optimal functional outcomes can be achieved through targeted interventions and a focus on overall health.
- The diagnosis of MS is made from clinical, radiological, and histopathological evidence and is characterised by hallmark findings of enchondromatosis in association with multiple hemangiomas.
- Individuals with MS presenting with disabling angular deformities and limb length discrepancy can be appropriately managed with limb reconstructive procedures using an external fixator.
- Meticulous surgical planning and application of the principles of deformity correction in managing these complex deformities should lead to optimal functional outcomes.
- Routine whole-body screening with appropriate imaging is essential to identify associated malignancies affecting multiple organs.
References
- 1.Kaplan RP, Wang JT, Amron DM, Kaplan L. Maffucci’s syndrome: Two case reports with a literature review. J Am Acad Dermatol 1993;29:894-99. [Google Scholar | PubMed]
- 2.Khan MT, Arooj S, Mukhtar MU, Raman R. Maffucci syndrome: Case report and review of diagnostic signs of the rare disease. Radiol Case Rep 2022;17:3674-7. [Google Scholar | PubMed]
- 3.Amary MF, Damato S, Halai D, Eskandarpour M, Berisha F, Bonar F, et al. Ollier disease and Maffucci syndrome are caused by somatic mosaic mutations of IDH1 and IDH2. Nat Genet 2011;43:1262-5. [Google Scholar | PubMed]
- 4.Verdegaal SH, Bovée JV, Pansuriya TC, Grimer RJ, Ozger H, Jutte PC, et al. Incidence, predictive factors, and prognosis of chondrosarcoma in patients with Ollier disease and Maffucci syndrome: An international multicenter study of 161 patients. Oncologist 2011;16:1771-9. [Google Scholar | PubMed]
- 5.Madan SS, Robinson K, Kasliwal PD, Bell MJ, Saleh M, Fernandes JA. Limb reconstruction in Ollier’s disease. Strategies Trauma Limb Reconstr 2015;10:49-54. [Google Scholar | PubMed]
- 6.Kumar A, Jain VK, Bharadwaj M, Arya RK. Ollier disease: Pathogenesis, diagnosis, and management. Orthopedics 2015;38:e497-506. [Google Scholar | PubMed]
- 7.El Abiad JM, Robbins SM, Cohen B, Levin AS, Valle DL, Morris CD, et al. Natural history of Ollier disease and Maffucci syndrome: Patient survey and review of clinical literature. Am J Med Genet A 2020;182:1093-103. [Google Scholar | PubMed]
- 8.Schwartz HS, Zimmerman NB, Simon MA, Wroble RR, Millar EA, Bonfiglio M. The malignant potential of enchondromatosis. J Bone Joint Surg Am 1987;69:269-74. [Google Scholar | PubMed]
- 9.Märtson A, Haviko T, Kirjanen K. Extensive limb lengthening in Ollier’s disease: 25-year follow-up. Medicina (Kaunas) 2005;41:861-6. [Google Scholar | PubMed]
- 10.Pandey R, White SH, Kenwright J. Callus distraction in Ollier’s disease. Acta Orthop Scand 1995;66:479-80. [Google Scholar | PubMed]
- 11.Verma GG, Jain VK, Iyengar KP. Monomelic Maffucci syndrome. BMJ Case Rep 2021;14:e239619. [Google Scholar | PubMed]
- 12.Angelini A, Baracco R, Dolci A, Vigo M, Mavrogenis AF, Ruggieri P. Limb lengthening for deformities in Ollier’s disease: A systematic review. Eur J Orthop Surg Traumatol 2020;30:1325-32. [Google Scholar | PubMed]
- 13.Huser AJ, Hoellwarth JS, Coppa V, Feldman DS, Paley D. Lengthening the lower extremities of children with Ollier’s and Maffucci’s enchondromatosis using implantable lengthening nails. Children (Basel) 2021;8:502. [Google Scholar | PubMed]









