The current study provides data on the demographics and the one-year mortality to the clinicians, health policymakers, and health administrators
Dr. Vivek Kumar David, Department of Orthopaedics, Gouri Devi Institution of Medical Science and College, Durgapur, West Bengal, India. E-mail: davidvivekkumar@gmail.com
Introductions: Proximal femur fractures are a significant public health issue and a leading cause of morbidity and mortality in the elderly. It poses a remarkable burden on healthcare resources.
Materials and Methods: Records of patients with proximal femur fracture operated during the study period (July 01, 2017–May 31, 2020) in our institution were obtained from hospital management system and analyzed retrospectively.
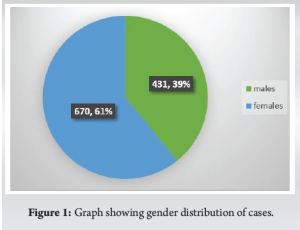
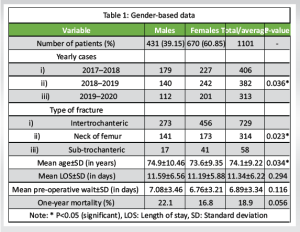
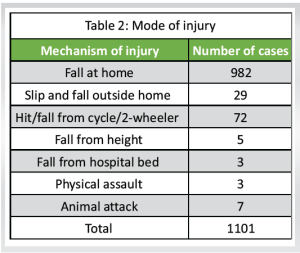
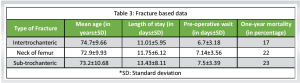
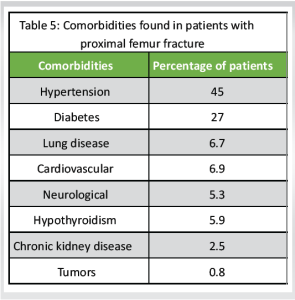
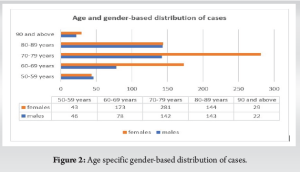
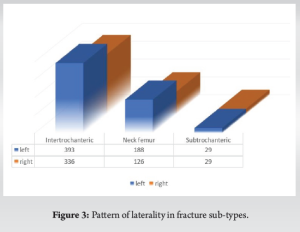
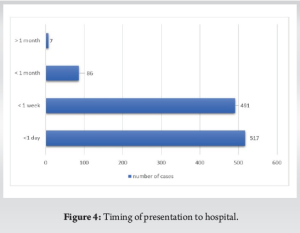
Results: Out of 1189 patients, 1101 met the inclusion criteria. About 66.21% were intertrochanteric, 28.52% were neck femur, and 5.26% were sub-trochanteric fractures. About 60.85% of patients were female. The mean age was 74.1 ± 9.22 years. Most injuries were domestic falls (89%) and left-sided (55%). The average delay in presentation to the hospital was 2.5 ± 6.62 days with mean length of stay being 11.34 ± 6.22 days and average pre-operative wait being 6.89 ± 3.34 days. Hypertension was the most common comorbid condition associated (45%) followed by diabetes (27%). About 4% also sustained other fractures; most common were distal end radius and proximal humerus fracture. Majority (63.7%) were operated between 3 and 7 days post-admission and the most common surgery performed was osteosynthesis with proximal femoral nail (39.69%). For mortality assessment, 34 patients died during hospital stay, 785 patients could be assessed and 282 were lost to follow-up. In-hospital mortality was 3.08%, 30-day mortality was 8.05% and 1-year mortality was 18.92%.
Conclusion: An integrated multidisciplinary approach with fall prevention awareness should be promoted to decrease the overall rate.
Keywords: One-year mortality, proximal femur fracture, demography.
Osteoporotic or fragility fractures around hip, spine, and wrist are a major health concern in the elderly population. Hip fractures contribute to significant morbidity and have a high rate of mortality (16–27%) in 1st year after fracture [1-4]. Elderly patients with hip fracture constitute the single largest group of emergency orthopedic admissions and significant department workload [5,6]. Proximal femur fracture comprises neck femur and intertrochanteric fractures (over 90%) and sub-trochanteric fractures (5–10%). Most of these occur following a fall with a lifetime risk being 23.3% in men and 11.2% in women [7]. The incidence of fracture and their economic impact on public health are necessary to assess and devise preventive strategies [8,9]. Unlike other countries, India lacks data for fragility hip fractures, thus incidence and the magnitude of this public health issue are not known, the treatment is not standardized and there is no universal treatment protocol [10]. According to report in 2004 estimated an annual incidence of 600,000 osteoporotic hip fractures, and this was expected to increase significantly by 2026, as the share of people over 60 years rises to 12.4% of 1.36 billion population [11]. It has been estimated that by 2030, 45.4% of the health burden in India is expected to be of older adults [12]. By 2050,323 million people in India are expected to be 60 years and older and half of hip fractures will occur in Asia [8-15]. Most of the expenses are paid out of pocket and not through insurance. According to the National Family Health Survey-3, the private medical sector remains the primary source of healthcare for 70% and 63% of households in urban and rural areas, respectively and public sector for the poor [11]. In the present study, we have assessed the demographics of proximal femur fractures of the last 3 years (June-2017-May-2020) in a 983-bedded primary-referral-center located in East Singhbhum district of Jharkhand state of India. The aim is to provide information on the demographics in play and the 1-year mortality to the clinicians, health policymakers and administrators.
Between June 01, 2017 and May 31, 2020, patients aged 50 years or more, diagnosed with proximal femur fractures (neck, intertrochanteric and sub-trochanteric) and operated in our hospital were included in the study. The data acquisition is from the hospital management system after taking clearance from the institutional ethics committee. Patients were excluded from the study if the fracture was pathological due to metastatic disease or primary bone tumors. Patients <50 years of age, operated for implant failure/revision surgeries, managed conservatively on traction owing to very high risk associated with surgery, or who did not consent for surgery or died preoperatively due to medical complications were also excluded from the study. Patients who did not visit for regular follow-ups were reached telephonically to calculate 1-month and 1-year mortality. The data collected were entered in Microsoft Excel and Statistical Package for the Social Sciences v23 was used for and statistical analysis. Continuous variables were analyzed using student t-test for two independent groups and analysis of variance for more than two groups. Discrete variables were analyzed using Chi-square where applicable. A P ≤ 0.05 was considered as significant.
During the study period, 1189 patients with proximal femur fractures were operated. Of these, 1101 patients met the inclusion criteria. About 66.21% were intertrochanteric fractures (n = 729; proximal femoral nailing [PFN] in 387, dynamic hip screw [DHS] in 339, dynamic condylar screw [DCS] in 3), 28.52% neck femur fractures (n = 314; Bipolar hemiarthroplasty in 297, cannulated cancellous screw fixation in 16, total hip replacement in 1) and 5.26% were sub-trochanteric fractures (n = 58; PFN in 50, DCS in 5, interlocking nailing in 2, DHS in 1). Thirty-four patients died during the hospital stay, 337 patients had regular follow-ups beyond 1 year, 448 patients who did not follow-up could be contacted and 282 were lost to follow-ups out of 1101 patients, no statistically significant differences were observed among patients.
Characteristics of study population
Wide range of age distribution exists from 50 to 106 years, the average age (and standard deviation) was 74.1 ± 9.22 years with mean being 74.9 ± 10.46 years in males and 73.6 ± 9.35 years in females (P < 0.03) Table 1 & Fig. 1. Among females, a major proportion (41.94%) of patients presented in their 7th decade of life, whereas in males, the presentation was similar in their 7th (32.9%) and 8th decade (33.1%) (Fig. 2). The majority (n = 710, 64.48%) were in the age group of 70–89 years with lowest numbers in 90 and above age group (n = 51, 4.63%). Around 55% (n = 610) sustained injury to the left side (Fig. 3). The most common injuries were domestic falls (89%). Other modes of injury are described in Table 2. The average delay in the presentation of the patient to the hospital after sustaining injury was 2.5 ± 6.62 days, range extending from 0 to 120 days (Fig. 4). During hospitalization, all the patients were managed based on standard institutional protocols for age, type, and location of fracture. The most common surgical procedure performed was internal fixation with PFN (n = 437, 39.69%). The mean length of stay (LOS) was 11.34 ± 6.22 days with the average pre-operative stay being 6.89 ± 3.34 days. Majority (n = 702, 63.7%) were operated between 3 and 7 days post-admission. The variable-based cumulative figures are entered in Tables 1 and 3. About 4% of patients (n = 47) sustained other injuries as well, majority being distal end radius and proximal humerus fracture (Table 4). Hypertension (45%, n = 496) and diabetes (27%, n = 298) were the most common comorbidities (Table 5). Majority (86.6%) had up to two comorbidities and the rest had more than two. Only 38% (n = 423) dint have any associated comorbid conditions.

Mortality assessment
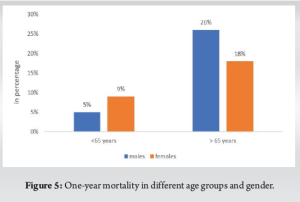
The in-hospital mortality (death in post-operative phase before discharge) was 3.08% (n = 34) with 31 among>65-year-old group. The average 1-year mortality was 18.92% (n = 155) and the 1-month mortality was calculated to be 8.05% (n = 66). The 1-year mortality rate was significantly higher in ≥65-years-old age group (Fig. 5). Furthermore, it was more in patients with LOS more than the mean value (P < 0.0001). Type of fracture or operative intervention (Table 3), delay in presentation did not have a statistically significant difference over the 1-year mortality. However, the mortality rate in males was high, 22% (Table 1). It was significantly more in males more than 65 years old (P = 0.01) and with medical comorbidities (P = 0.001) when compared to females. It was also more in patients where the surgery was delayed more than the mean pre-operative period (27%). Older males (>65 years) with medical comorbidities had the highest rates (31%).
Incidence of hip fracture differs between and within countries, between rural and urban areas, between different races. We could find only a few epidemiological studies on hip fractures with a sample size of more than 500 patients published from India but none of these have estimated the 1-year mortality in PubMed database [9,10,16]. The highest rates in the world were found in studies from Oslo, Norway [10,17]. India inhabiting 1.2 billion people is expected to overtake China in a decade to become the world’s most populous country. 65% of the aged individuals, especially elderly females (more than 80%) are dependent on others for their day-to-day maintenance [10,18]. A decrease in bone mineral density with aging, particularly in women leads to an increased prevalence of osteoporosis and the highest rate of hip fractures in older women [19]. The demographic of our study is similar to the statistics of the hip fracture globally, average age ≥65 years (n = 915, 83.1%) and about two-thirds occurring in women. This is, however, in contrast to other studies from India where the mean age was found under 60 years, and it was postulated that the occurrence of osteoporosis in India occurs a decade earlier compared to Western countries [9,16]. Most common cause of hip fracture was domestic fall, from a standing height (89%). The various reasons patients enumerated included slip on a wet or an uneven surface or stairs, fall in bathroom, loss of control while getting up from bed/raising from chair, and giddiness. Many elderly have poor balance, diminished vision, and neurological diseases which cause the fall. Majority (53%, n = 584) presented to the hospital after 24 h of sustaining injury. Several factors contribute to the delayed presentation such as lack of resources including financial and transportation constraints, illiteracy, ignorance, lack of care of elderly, practice of quackery and home-based treatment, and delay in referral to a well-equipped treatment center after initial treatment at local hospitals. The LOS varies significantly by region. Studies from North America reported the shortest mean LOS (6.4 days), whilst studies from Asia had the longest LOS (32.1 days) [19]. There are conflicting studies which associate increased LOS to an increased 1-year mortality [20,21,22]. In our study, patients with a shorter LOS had a significantly lower 1-year mortality. Furthermore, it has been observed that males with hip fracture are usually older, with more medical comorbidities, and thus, have an increased LOS and cost of treatment [19,23]. We did not find any gender based statistical difference in average LOS (P = 0.29) but the 1-year mortality was more in males, significantly in above 65-year-old age group. On the contrary, more females were diagnosed to have associated medical comorbidities (65%, n = 435). Dhanwal et al., who conducted the first incidence study from India, found the highest rates of hip fracture in males in 85–90 year age group [9]. We observed that the proportion of males under our study increased in the age group of 80–89 years relative to females. The mean pre-operative wait was 6.89 days, like other studies from India [11,16]. Factors contributing to delay include medical comorbidities, fixed operative days in a week due to the structural organization of the department, delays in financial clearance by the patient attendants (as many belong to lower and middle-class families lacking medical insurance), etc. A longer time to surgery was associated with an increased LOS. In recent times, studies suggest a decreasing incidence or a plateau of hip fractures, albeit the total proportion of patients is on a rise [4, 24-26]. The patients admitted during the study period show a significant declining trend (Table 1) but we attribute the decrease in 3rd year to SARS-CoV-2 pandemic when the total number of admissions and surgeries was drastically reduced. The in-hospital mortality rate in our study was 3%. Nikkel et al. and Schnell et al. reported similar rates [20,27]. The 1-month mortality rate was comparable to other published data [28]. Older adult patients with hip fractures are 3–4 times more likely to die within 1-year after surgery than the general population [29]. Increasing age above 65, male sex with associated comorbidities, prolonged LOS and excessive delay in surgery are the negative predictive factors of the survival 1 year after surgery in our study. International guidelines suggest fixation of proximal femur fractures preferably within 24–48 h and relate it to decreased 1-year mortality. There are studies citing a positive, negative, or neutral correlation of early surgical intervention to 1-year mortality [30]. The timing of surgery in our study was delayed on an average to a week’s time, yet the short-term and 1-year mortality rate are comparable to most of the studies published. Proper evaluation and pre-operative optimization were required as the general population is not completely aware of their pre-existing medical conditions. However, undue delay is not warranted. The primary care physicians in the remote locations where the specialists are deficient and who usually are the first line of contact can raise awareness among families to maintain a healthy well-being and good nutrition, educate them on how to minimize the risks of falls, to identify and seek treatment of various comorbidities, diagnose and refer the cases of fracture to prevent unwarranted delays. Multicentric trials and prospective studies are required to assess factors contributing to 1-year mortality and help in framing definitive protocols to decrease the rate in Indian population.
There are limited research articles published in South-Asian countries worked up on osteoporotic hip fractures. The estimation of incidence, prevalence, mortality, and the economic costs incurred are not known. Thus, there is a lack of standardization in methodology to estimate the burden of the disease. With the increasing population, especially the proportion of elderly and unavailability of data, there is a need for more research so that policies can be made to lay out standard protocols and healthcare plans in the management of osteoporotic hip fractures. There is a need to raise awareness to prevent falls in the high-risk population by increasing information accessibility and reducing risk factors. Implementing integrated care in elderly who fell, a thorough evaluation, early intervention, and decreasing in-hospital stay are a few propositions we believe should be considered in a standard healthcare plan for the management. This study highlights that there is an increasing burden of the geriatric population and with the medical facilities being more accessible, number of such fractures being diagnosed and managed is bound to increase. As these fractures occur following a trivial fall on an osteoporosis skeletal system, there is a need to raise awareness to decrease the incidence of fall, especially domestic injuries. An early diagnosis and management of medical comorbidities by the primary care physicians in the pre-fall status can decrease the pre-operative time and post-operative stay of the patient which has a direct relation to 1-year survival rate post-surgery. Further multi-centric trials are required to help frame definite management protocols.
Given the significant mortality rates and healthcare burden, a proactive, integrated multidisciplinary approach is essential. Efforts should be focused on early surgical intervention to minimize delays, comprehensive management of comorbidities and fall preventions to enhance survival rates and quality of life among elderly patients with proximal femur fractures.
References
- 1.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 2006;17:1726-33. [Google Scholar]
- 2.De Laet CE, van Hout BA, Burger H, Weel AE, Hofman A, Pols HA. Incremental cost of medical care after hip fracture and first vertebral fracture: The Rotterdam study. Osteoporos Int 1999;10:66-72. [Google Scholar]
- 3.Berecki-Gisolf J, McClure R, Seubsman SA, Sleigh A, Thai Cohort Study Team. Reporting of lifetime fractures: Methodological considerations and results from the Thai cohort study. BMJ Open 2012;2:e001000. [Google Scholar]
- 4.Adeyemi A, Delhougne G. Incidence and economic burden of intertrochanteric fracture: A Medicare claims database analysis. JBJS Open Access 2019;4:e0045. [Google Scholar]
- 5.Parker M, Johansen A. Hip fracture. BMJ 2006;333:27-30. [Google Scholar]
- 6.Lee YH, Lim YW, Lam KS. Economic cost of osteoporotic hip fractures in Singapore. Singapore Med J 2008;49:980-4. [Google Scholar]
- 7.Filipov O. Epidemiology and social burden of the femoral neck fractures. J IMAB 2014;20:516-8. [Google Scholar]
- 8.Maghbooli Z, Hossein-Nezhad A, Jafarpour M, Noursaadat S, Ramezani M, Hashemian R, et al. Direct costs of osteoporosis-related hip fractures: Protocol for a cross-sectional analysis of a national database. BMJ Open 2017;7:e014898. [Google Scholar]
- 9.Dhanwal DK, Siwach R, Dixit V, Mithal A, Jameson K, Cooper C. Incidence of hip fracture in Rohtak district, North India. Arch Osteoporos 2013;8:135. [Google Scholar]
- 10.Dash SK, Panigrahi R, Palo N, Priyadarshi A, Biswal M. Fragility hip fractures in elderly patients in Bhubaneswar, India (2012-2014): A prospective multicenter study of 1031 elderly patients. Geriatr Orthop Surg Rehabil 2015;6:11-5. [Google Scholar]
- 11.Rath S, Yadav L, Tewari A, Chantler T, Woodward M, Kotwal P, et al. Management of older adults with hip fractures in India: A mixed methods study of current practice, barriers and facilitators, with recommendations to improve care pathways. Arch Osteoporos 2017;12:55. [Google Scholar]
- 12.Chatterji S, Kowal P, Mathers C, Naidoo N, Verdes E, Smith JP, et al. The health of aging populations in China and India. Health Aff (Millwood) 2008;27:1052-63. [Google Scholar]
- 13.Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop 2011;45:15-22. [Google Scholar]
- 14.Boufous S, Finch C, Close J, Day L, Lord S. Hospital admissions following presentations to emergency departments for a fracture in older people. Inj Prev 2007;13:211-4. [Google Scholar]
- 15.Leslie WD, Metge CJ, Azimaee M, Lix LM, Finlayson GS, Morin SN, et al. Direct costs of fractures in Canada and trends 1996-2006: A population-based cost-of-illness analysis. J Bone Miner Res 2011;26:2419-29. [Google Scholar]
- 16.Bishnoi M, Kirmani TT, Huda N, Chahal G, Bishnoi S. Epidemiological analysis of hip fractures at a tertiary care center: A retrospective study. Int J Res Orthop 2018;4:568-71. [Google Scholar]
- 17.Bjørgul K, Reikerås O. Incidence of hip fracture in Southeastern Norway: A study of 1,730 cervical and trochanteric fractures. Int Orthop 2007;31:665-9. [Google Scholar]
- 18.Elderly in India; 2016. Available from: https://mospi.nic.in/sites/default/files/publication_reports/ElderlyinIndia_2016.pdf [Last accessed on 2020 Dec 30]. [Google Scholar]
- 19.Williamson S, Landeiro F, McConnell T, Fulford-Smith L, Javaid MK, Judge A, et al. Costs of fragility hip fractures globally: A systematic review and meta-regression analysis. Osteoporos Int 2017;28:2791-800. [Google Scholar]
- 20.Nikkel LE, Kates SL, Schreck M, Maceroli M, Mahmood B, Elfar JC. Length of hospital stay after hip fracture and risk of early mortality after discharge in New York State: Retrospective cohort study. BMJ 2015;351:h6246. [Google Scholar]
- 21.Nordström P, Gustafson Y, Michaëlsson K, Nordström A. Length of hospital stay after hip fracture and short term risk of death after discharge: A total cohort study in Sweden. BMJ 2015;350:h696. [Google Scholar]
- 22.Yoo J, Lee JS, Kim S, Kim BS, Choi H, Song DY, et al. Length of hospital stay after hip fracture surgery and 1-year mortality. Osteoporos Int 2019;30:145-53. [Google Scholar]
- 23.Barnea R, Weiss Y, Abadi-Korek I, Shemer J. The epidemiology and economic burden of hip fractures in Israel. Isr J Health Policy Res 2018;7:38. [Google Scholar]
- 24.Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Järvinen M. Nationwide decline in incidence of hip fracture. J Bone Miner Res 2006;21:1836-8. [Google Scholar]
- 25.J u DG, Rajaee SS, Mirocha J, Lin CA, Moon CN. Nationwide analysis of femoral neck fractures in elderly patients: A receding tide. J Bone Joint Surg Am 2017;99:1932-40. [Google Scholar]
- 26.Zhang C, Feng J, Wang S, Gao P, Xu L, Zhu J, et al. Incidence of and trends in hip fracture among adults in urban China: A nationwide retrospective cohort study. PLoS Med 2020;17:e1003180. [Google Scholar]
- 27.Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL. The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil 2010;1:6-14. [Google Scholar]
- 28.Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, et al. Effect of early surgery after hip fracture on mortality and complications: Systematic review and meta-analysis. CMAJ 2010;182:1609-16. [Google Scholar]
- 29.Morri M, Ambrosi E, Chiari P, Orlandi Magli A, Gazineo D, D’Alessandro F, et al. One-year mortality after hip fracture surgery and prognostic factors: A prospective cohort study. Sci Rep 2019;9:18718. [Google Scholar]
- 30.Matassi F, Carulli C, Munz G, Lualdi C, Civinini R, Innocenti M. Preliminary results of an early versus delayed timing of surgery in the management of proximal femur fragility fractures. Clin Cases Miner Bone Metab 2015;12:11-7. [Google Scholar]







