This article presents an effective solution for providing fixation in the pubis with a Curvafix implantation for a pathologic fracture and a concurrent and ipsilateral total hip arthroplasty for osteoarthritis.
Dr. Alex Bassil, Department of Orthopaedic Surgery Duke University School of Medicine, Durham, North Carolina, USA. Email: alex.bassil@duke.edu
Introduction: The pelvis is one of the most common sites for metastatic spread to bone. Ensuing pathologic fractures pose major issues to patients. Fixation becomes essential to decrease pain and allow for weight-bearing. However, the pelvis poses a unique challenge as there are certain portions like the pubis that, because of their natural curve, are not amenable to plate or screw fixation.
Case Report: A 76-year-old female with known bone metastases presented to clinic with right hip pain. Computed tomography (CT) of the chest, abdomen, and pelvis revealed a new lesion in the lateral superior ramus involving the medial acetabulum. She also had osteoarthritis of the hip, for which she had an upcoming total hip arthroplasty scheduled. We performed intramedullary fixation of the lesion in the lateral superior ramus with a Curvafix nail concurrently with total hip arthroplasty.
Conclusion: This case report demonstrates the utilization of a Curvafix nail in the oncologic context of an anterior column acetabular fracture along with a concurrent ipsilateral total hip arthroplasty.
Keywords: Curvafix nail, THA, pubis, acetabulum, pathologic fracture.
Prophylactic fixation of metastatic lesions to the pelvis is performed to reduce pain and to allow the ability to continue weight-bearing with less fear of suffering a pathologic fracture [1, 2]. Prophylactic fixation is essential as metastatic bone disease predisposes patients to fractures. In addition, oncologic treatments such as certain types of chemotherapy are known to contribute to bone loss [3]. After the spine, the pelvis is the most common bone for metastases to travel to [4]. This demonstrates a clear need for effective interventions for prophylactic fixation in the pelvis. Because of the morbidity of operating on the pelvis, the less invasive a means of prophylactic stabilization, the more desirable the intervention [5]. Presently, there are percutaneous interventions that attempt to achieve this, such as cementoplasty, ablation, percutaneous screw fixation, and the Illuminoss system [6]. In addition, patients may receive plate or screw fixation to stabilize the bone that is implicated by these lesions. However, the natural curvature of the bony pelvis can make plate or screw fixation a challenge, leading to longer surgeries (such as the cup-cage reconstruction of the acetabulum) that may lead to greater blood loss and longer stays in the hospital [7]. The minimally invasive percutaneous interventions such as cementoplasty and ablation are quicker procedures that can be an effective form of palliation [8]. However, cementoplasty does not lead to as rigid of fixation as screws or plates do nor does it replace diseased bone in the way that an open acetabular reconstruction can. Ideally, there would be an intervention that provides rigid fixation with shorter operating times to decrease post-operative morbidity. The CurvaFix intramedullary implant was designed for the purpose of fixation after pelvic trauma but it can be readily adapted to prophylactic fixation of oncologic lesions. There is a single case report detailing its oncologic use in an upper sacral fragility fracture in a patient with metastatic pancreatic cancer. The CurvaFix system itself is an interlocking segment, similar to a flexible reamer, that contains a series of cables that rigidly lock the cables into place once the device attains the desired shape and location. The following case report illustrates an example of the CurvaFix nail used for intramedullary fixation of a pathologic fracture in the pubis and anterior column of the pelvis for metastatic disease in conjunction with an ipsilateral total hip arthroplasty for osteoarthritis. To our knowledge, this is the first case of its kind reported in the literature.
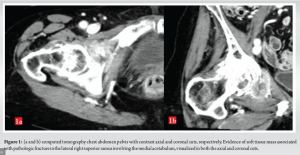
A 77-year-old female presented to the orthopedic oncology clinic with right hip pain. She had a history of stage IIIC1 mixed serous, endometrioid, and endometrial adenocarcinoma and recurrent breast cancer with known bone metastases. She had previously finished a course of chemotherapy for endometrial cancer and received a lumpectomy and radiation for breast cancer. When she presented, she was on zoledronic acid for bone metastases. She followed up with gynecologic oncology for this but was referred to orthopedic oncology because of worsening hip pain that started after a fall. She received imaging that demonstrated a pathologic fracture in the right inferior pubic ramus at the site of a known lytic lesion, in addition to severe osteoarthritis. She received an intra-articular steroid injection as her pain on the exam was thought to be contributed by her osteoarthritis. However, she received no relief. She presented to the clinic ambulating with the aid of a cane. We referred her to interventional radiology to have a cryoablation performed which was successful. However, a few months later, she represented with significant pain in the right hip, as well as progressive weight loss and fatigue. Computed tomography chest, abdomen, and pelvis at that time revealed a new lesion in the lateral superior ramus involving the medial acetabulum (Fig. 1). The patient had been scheduled for a total hip arthroplasty already at an outside hospital. However, because this new lesion involved the acetabulum, she returned for consideration of concurrent total hip arthroplasty and fixation of the pathologic fracture. The patient was in favor of this approach and agreed to the surgical plan.
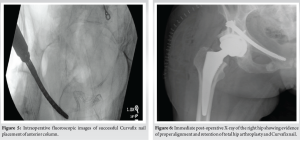
We used a Kocher-Langenbeck posterior approach to the hip/acetabulum. Exposure was taken more proximally by elevating the gluteus minimus off the posterior column of the acetabulum. The start point for the Curvafix nail was found directly posteriorly and superiorly from the acetabulum. We used the three primary fluoroscopic views (AP of the pelvis, obturator inlet, and outlet views) to place a guidewire along with the opening reamer at the start point for an antegrade anterior column screw (Fig. 2). The guidewire was placed down along the anterior column across the tumor site along the superior pubic ramus and pubic root (Fig. 3). 
The desired screw length was measured to be 110 mm. A reamer was placed across the guidewire and reamed. A 7.5 mm × 110 mm Curvafix screw was then placed in standard fashion and deployed, thus locking the cables into place (Fig. 4 and 5).
We then turned our attention to the total hip arthroplasty. After the acetabulum was reamed to the floor of the fovea, the floor fovea showed 1 mm of metal at the base from the Curvafix screw behind the acetabulum wall, and roughly 1/8 of the cup surface showed tumor that was embedded. We removed the tumor with a rongeur and sent it for pathology. We then reamed in line with the normal acetabular version. There was minimal exposure of the nail, so we opted for press fit over cement (Fig. 6). She was made partial weight-bearing to 50% for the first two and a half weeks when she was progressed to weight-bearing as tolerated. Otherwise, she was kept on hip precautions until 6 weeks post-operative. She had resolution of her pre-operative pain by two and a half weeks post-operative, at which time she progressed to weight-bearing as tolerated. At her 6-week post-op visit, she remained pain-free in the hip, and radiographs of the hip showed no evidence of hardware complication. She most recently followed up at 5 months post-operative in which repeat X-ray of the hip showed intact implants without evidence of loosening or failure (Fig. 7).
Metastatic lesions of the pelvis causing pathologic fractures are significant sources of pain for patients. When compounded on a known history of osteoarthritis in the joint adjacent to the lesion or due to the presence of metastatic bone disease in the proximal femur, the pain and gait dysfunction are even worse. To our knowledge, there is no case reported in the literature of a Curvafix nail used in the pubic rami for oncologic fixation of a pathologic fracture. In addition, we are also not aware of any case that demonstrates ipsilateral total hip arthroplasty performed concurrently in the same surgery with the fixation. Although this implant was placed through an extended posterior approach to the hip and acetabulum, the Curvafix implant can be placed in a minimally invasive fashion. Because patients with metastatic bone disease seek quality-of-life improvements with minimal hospital time, this offers an advantage over more invasive procedures such as plate and screw fixation of the pelvis or cup-cage reconstruction. It is not the only minimally invasive option. Percutaneous cementoplasty, either with or without screw augmentation, has become a relatively common procedure. However, the curved anatomy of the pelvis is not amenable to the placement of straight screws. In addition, the IluminOss fixation system is a relatively new device that utilizes an insertable balloon catheter that expands and contains a light curable polymer that induces intramedullary fixation. There are studies demonstrating its efficacy for fixation in bones with a natural curve, such as the pubis [9]. There is also a report in the literature of a pubic rami fracture fixation by use of interlocking intramedullary nail in 2018 by Ivanov et al. [10]. The Curvafix implant offers the ability for minimally invasive placement, flexibility to adapt to the contours of the region of the pelvis being spanned, and the ability to lock the implant rigidly once the desired location and contour are achieved. As with other minimally invasive methods, this can reduce morbidity in terms of blood loss, increased operative times, and longer length of stay in the hospital [5]. As demonstrated here, placement of the Curvafix implant across the anterior column does not preclude placement of a total hip arthroplasty. Pre-operatively, on January 23, 2024, the patient had the following range of motion values for her right hip. Flexion: 80°; Extension: 10°; Abduction: 20°; Adduction: 10°; External rotation: 20°; and Internal rotation: 20°. At her 5-month post-operative visit, the patient had the following range of motion values: Flexion: 100°; Extension: 20°; Abduction: 35°; Adduction: 15°; External rotation: 35°; and Internal rotation: 25° (Fig. 8). She did have pain with range of motion at this time given further spread of her metastatic disease in the hip and torso.
This case demonstrates the ulterior utility of the Curvafix nail for prophylactic fixation of oncologic lesions in the acetabulum. We also demonstrated that it is possible to perform this fixation concurrently with an ipsilateral total hip arthroplasty. These surgeries led to complete palliation of the patient’s pre-operative pain and the ability to bear weight freely. The Curvafix nail should be considered when performing prophylactic fixation in a bone with a natural curve such as the pubis. This method of intramedullary fixation can be performed in conjunction with an open procedure or can be performed percutaneously, offering advantages over open interventions.
This is an important case report for the literature because this is a unique example of treating two separate, painful pathologies that may present in conjunction in elderly patients-osteoarthritis and a pathologic fracture-in one single surgery. It also displayed a unique application of the Curvafix nail that has not been reported in the literature.
References
- 1.Piccioli A, Rossi B, Scaramuzzo L, Spinelli MS, Yang Z, Maccauro G. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury 2014;45:412-7. [Google Scholar]
- 2.Park JW, Kim YI, Kang HG, Kim JH, Kim HS. Joint-preserving palliative surgery using self-locking screws of intramedullary nail and percutaneous cementoplasty for proximal humeral metastasis in the advanced cancer patients. World J Surg Oncol 2018;16:93. [Google Scholar]
- 3.Guise TA. Bone loss and fracture risk associated with cancer therapy. Oncologist 2006;11:1121-31. [Google Scholar]
- 4.Prabowo Y, Asril E, Wikanjaya R. Functional outcome of operative treatment for pelvic metastatic bone disease from primary thyroid cancer: A case series. Int J Surg Case Rep 2020;66:288-97. [Google Scholar]
- 5.Mostafa AM, Kyriacou H, Chimutengwende-Gordon M, Khan WS. An overview of the key principles and guidelines in the management of pelvic fractures. J Perioper Pract 2021;31:341-8. [Google Scholar]
- 6.Lea WB, Neilson JC, King DM, Tutton SM. Minimally invasive stabilization using screws and cement for pelvic metastases: Technical considerations for the pelvic “Screw and Glue” technique. Semin Intervent Radiol 2019;36:229-40. [Google Scholar]
- 7.Rommens PM, Hofmann A, Kraemer S, Kisilak M, Boudissa M, Wagner D. Operative treatment of fragility fractures of the pelvis: A critical analysis of 140 patients. Eur J Trauma Emerg Surg 2022;48:2881-96. [Google Scholar]
- 8.Pusceddu C, De Francesco D, Ballicu N, Santucci D, Marsico S, Venturini M, et al. Safety and feasibility of steerable radiofrequency ablation in combination with cementoplasty for the treatment of large extraspinal bone metastases. Curr Oncol 2022;29:5891-900. [Google Scholar]
- 9.Oikonomidis S, Alabsi A, Ashqar G, Graf M, Sobottke R. Intramedullary stabilization of pubic ramus fractures in elderly patients with a photodynamic bone stabilization system (IlluminOss). Geriatr Orthop Surg Rehabil 2019;10:2151459318824904.1-7. [Google Scholar]
- 10.Ivanov PA, Zadneprovsky NN, Nevedrov AV, Kalensky VO. Pubic rami fractures fixation by interlocking intramedually nail: First clinical experience. Traumatol Orthop Russia 2018;24:111-20. [Google Scholar]