To propose a better recommendation for treatment of distal femoral fracture .
Dr. Ayush Prakash, Department of Orthopaedics, GSVM Medical College, Kanpur, Uttar Pradesh, India. E-mail: ayushprakashemail@gmail.com
Introduction: Treatment of supracondylar and intercondylar fractures of the distal femur has historically been difficult. These fractures are often unstable and comminuted and tend to occur in the elderly or in patients with multiple injuries.
Objective: The purpose of the study is to assess the functional and radiological outcome of locking plate fixation in AO type 33C distal femur fractures.
Materials and Methods: A total of 49 patients with distal femoral fractures were operated by open reduction with internal fixation with a distal femur-locking compression plate (LCP) through the standard swashbuckler approach. The functional and radiological outcomes were assessed using the Neers scoring system.
Results: Out of 49 patients, Muller type C2 was the most common fracture with 36 out of 49 (73.5%). Union was found in 47 patients with two patients presenting with non-union. The average union time of the fracture was 12–20 weeks with the mean time of union being 16.2 weeks. All patients were successfully given a walking aid in the 20th week. The average knee score was 79.71 using the Neers scoring system.
Conclusion: Fractures of the distal femur are more common in high-velocity injuries and occur in middle-aged males and old age women. Most fractures were comminuted. LCP appears to be technically an ideal implant for comminuted distal femoral fractures with proper physiotherapy producing excellent results. Knee stiffness was the most common complication.
Keywords: Distal femur fracture, distal femur locking compression plate, intercondylar femur fracture.
Distal femoral fracture is one of the most common lower limb injuries and it accounts for <1% of all fractures. Historically, supracondylar and intercondylar fractures of the distal femur have been known to impose challenges to the orthopedic surgeons. These fractures are often unstable and comminuted. They make up 7% of all femur bones. Thirty-one percentages of femoral fractures involve the distal portion. The highest rates are in women over 75 and boys and men ages 15 to 24. Most fractures are the result of high trauma and cause extensive tissue and joint damage and metaphyseal comminution. The incidence of malunion, non-union, and infection is high in many studies. Past joint arthroplasty might complicate treatment in older patients [1]. As the AO group improved its internal fixation devices, treatment recommendations began to change. The overall result of intra-articular fractures is less than ideal, and the effects of operative and non-operative treatments are similar. As these fractures can be better understood using new tests such as computed tomography scans/magnetic resonance imaging, surgery has become the first option in treating these fractures. The current generation of distal femoral locking compression plates (LCPs) is pre-shaped to the average anatomy and creates a fixed-angle construct. The pullout ability of locking screws is higher than traditional screws, making them particularly suitable for osteoporotic bones. These are designed to be used in a minimally invasive fashion to protect local biology and prevent fracture healing and infection. Early mobilization of the knee is important in obtaining a good result [1,2]. The purpose of this study was to assess the functional and radiological outcome of locking plate fixation in AO type 33C distal femur fractures. We wanted to assess the outcome in terms of union, wound healing, and range of motion.
It is a prospective study in which a total of 49 patients with distal femoral fractures reporting to Orthopedics OPD/Emergency, GSVM Medical College, and associated LLR Hospital and treated by LCP fixation were chosen and sampling based on the inclusion and exclusion criteria were included in the study. Patients of the age group 18–70 years with AO type 33C distal femur fractures who were willing for follow-up and fit for surgery were included in the study. Adequate hemodynamic stabilization of the patient and a detailed examination of the various injuries were done on admission.
A radiological assessment with anteroposterior and lateral X-rays was done. The fracture was classified using the AO/OTA or Muller classification [3]. The patients were operated using the standard Swashbuckler approach [3,4]. Proper post-operative rehabilitation played a major role in the recovery of the range of movement and improved the power of the quadriceps and the functions of the joint. Rehabilitation was customized according to the patient and the fracture type. Patients were followed up at 1st, 2nd, 4th, 6th month, and 1-year intervals. The results were clinic radiologically assessed with anteroposterior and lateral radiographs at each follow-up. The fracture was said to be radiologically united if the callus was seen in at least three cortices in anteroposterior and lateral views. The functional outcomes were analyzed using the Neers knee scoring system.
In our study, 49 patients with intercondylar femur fracture were operated on with open reduction with internal fixation (ORIF) with distal femur-locking compression. Patients were followed up at 1st, 2nd, 4th, 6th month, and 1-year intervals.
Demography
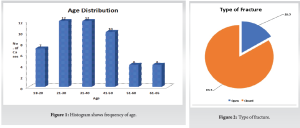
In our study, the majority of injured patients were male (81.6%) who showed that men participated in outdoor activities and the highest number of patients was in the 21–40 age group (49%).
Tables 1 and 2, Fig. 1

Type of fracture
Most of the fractures in this study group were of closed type (83.7%).
Table 3, Fig. 2
AO type of fracture
Table 4
Majority of the fractures belonged to AO type C2 accounting for 73.5% whereas only 2% in our study group belonged to type C3 .
Mean range of motion during follow-up period
Table 6 Mean range of motion during the follow-up period.
The mean range of motion was 97.95° at the end of 1 year with the maximum gain in knee flexion of 130° and the minimum was 20°.
The average knee score was 79.71 using the Neers scoring system.
Union was found in 47 patients with two patients presenting with non-union. Among the 47 patients, seven patients presented with malunion. Two patients who presented with non-union required reoperation. The average union time of the fracture was 12–20 weeks with the mean time of union being 16.2 weeks. All patients were successfully given a walking aid by the 20th week.
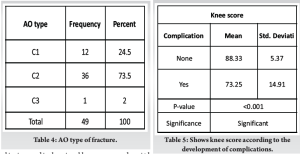
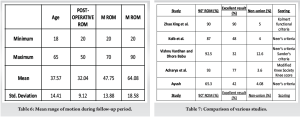
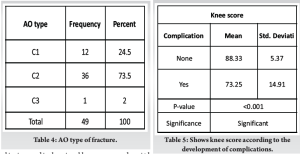
Table 5 – shows knee score according to development of complications.
Twenty-eight out of 49 patients developed complications (57.14%). Eleven developed knee stiffness, three developed surgical site infections, and three developed both. Limb length discrepancy was found in two patients, varus angulation and malunion were found in seven patients, and non-union was found in two patients. Reoperation is required in two cases due to non-union. The knee score value was not significant with respect to age, sex, mode of injury, type of fracture, associated injury, and AO type. Of the 36 C2 strains, 15 had excellent results, 13 had good results, six had fair results, and two had poor results. Only one patient with type C3 was included and the results were negative.
Management of distal femoral fractures has been a matter of discussion over the decade. There has been a change in philosophy in the surgical treatment of intercondylar fractures of the distal femur. Treatment of choice earlier was close management of these fractures, due to the non-availability of appropriate implants and lack of proper techniques.
Surgical stabilization at an early stage can facilitate care of the soft tissue, it permits early mobility and reduces the complexity of nursing care. Open reduction and internal fixation have been the treatment of choice. A variety of implants used were angled blade plates, dynamic condylar screws (DCS), condylar buttress plates and interlocking nails, and LCP. A certain amount of good bone stock is required to fix angle devices such as condylar blade plate along with DCS to insert the lag screw and its entry makes a significant amount of bone loss from the lag screw entry site which itself compromises already fractured condyles; hence, it limits their use in some fracture type of intra-articular fracture. This was solved by condylar buttress plates for comminuted fractures. However, with standard buttress plating, these fractures often fall into varus deformity. The failure rate was high especially in osteoporotic bone. In 1973, Connoly advocated closed reduction and cast brace ambulation while in 1974, Schatzker[5] reported superior results using operative methods. Also in 1967, Neer[6,7] classified supracondylar/ intercondylar fractures, used straight plate and screws and considered conservative treatment was superior to internal fixation. Zehntner mk et al(1992) [8] evaluated 59 supracondylar & intercondylar fractures in 57 patients after a mean follow up of 5 years and 7 months after internal fixation using AO/ASIF technique. Axial alignment was compared with that of the uninjured side. Differences were within 5 degrees for more than 75% cases. Alignment differences were more frequent in complicated and intercondylar fractures. Simonian et.al (1998) [9] described push screw and double plating for fixation of distal femoral fractures as these fractures have a unique problem of loss of fixation of distal fragment. Loss of distal fixation leads to toggling distal screws which can lead to varus angulation and fracture fixation failure. Less Invasive Stabilisation system has been developed to provide multiple fixed angle distal locked screws and can be best thought as a submuscular internal fixation[9]. Biomechanical studies revealed that gross loosening of the standard condylar buttress plate and DCS occurred due to the toggle at the screw-plate interface, which leads to early implant loosening resulting in breakage of the implant and varus/valgus collapse of the distal fragment. To address these issues, a first-generation locking condylar plate was designed. Screw-plate toggle and motion at the bone-screw interface are minimized by a locking plate and provide more rigid fixation. Rigid fixation is felt to be one key to the successful treatment of these fractures. The conventional plates are associated with their own demerits such as screw pullout, implant failure, and unstable fixation needing post-operative immobilization. Delayed post-operative mobilization results in stiffness of the knee which is an indicator of poor outcome. The invention of a locking condylar buttress plate made fixation in osteoporotic and comminuted fractures easier. Hence, now with the evolution of locking compression plating for distal femoral fractures, especially for the comminuted intra-articular fractures, many of the older demerits could be addressed which includes the increased stability due to locking compression plating principle, multiple screw options in the distal fragment providing option for fixing the multiple fragments restoring the anatomical congruity and providing stable fixation of the distal fragment with the proximal fragment with resulting increased stability allowing for early mobilization. Current fracture patterns that we encounter are complex comminuted types due to the prevalence of high-speed vehicles mainly due to the high two-wheeler population in countries such as India. Improved health-care results in a longer life span and subsequently presents us with more osteoporotic fractures which were previously treated using conservative methods. The LCP is a single-beam construct where the strength of its fixation is equal to the sum of all screw-bone interfaces rather than a single screw’s axial stiffness and pullout resistance in unlocked plates. Its unique biomechanical function is based on splinting rather than compression resulting in flexible stabilization, avoidance of stress shielding, and induction of callus formation. It can also be used as biological fixation without disturbing the fracture site. Another fixation method is a less invasive stabilization system. The main difference between the distal femur-LCP and the LISS is that the LISS utilizes an outer jig device for shaft holes, functioning essentially as a locking guide jig, which is attached to the distal part of the plate and guides the placement of the proximal locking screws. The shaft holes on the distal femur-LCP are oval allowing for the options of a compression screw or a locking screw. This leads to a more precise placement of the plate, as it is able to be compressed more closely to the bone. Although distal femur-LCP is designed to fit the anatomy of the distal femur, we were worried about the fit in our local Asian population where shorter and smaller femurs are the norm. Comparable studies utilizing the distal femur-LCP demonstrate only short-term results. Although the follow-up period of our series was short, studies have shown that early function is comparable to final long-term outcome. The outcome seems to correlate with fracture severity, anatomic reduction, bone quality, length of time elapsed from injury to surgery, concomitant injuries, the exact positioning and fixation of the implant, and lastly the rehabilitation protocol and patient education and awareness. Furthermore, the initial severe concomitant cartilage damage may predispose to early osteoarthritis, although there is no evidence of that yet. In our study, 80% were male and 20% were female which is comparable to that of Chauhan et al. [10], Vishnu Vardhan and Dhorababu et al. (2021) [11], Borthakur et al. [12], Rauf et al. [13], and Konuganti et al. [14], which is quite a change from earlier studies such as Schuetz et al. [15], Syed et al. [16], Fankhauser et al. [17], and Wong et al. [18], all of which had a female preponderance and the age was also higher suggesting that most of them were in the elderly female mainly due to osteoporosis and weakened bones. The mean age in our study was 37.57 years (range 18–65 years), and the mean age in the study conducted by Kapil Mani et al. [19] was 40.75 years. The mode of injury was road traffic injury in 90% of cases, thereby signaling a shift from domestic fall in the elderly to high-energy trauma, that is, road traffic accident in mainly younger age group. We found a right-sided preponderance in our study with 86% right-sided, 12% left-sided, and 2% bilateral involvement. The average range of flexion achieved was 97.95° which is lower than other studies such as 115° in Vallier et al. [20], 117° in Kayali et al. [21], and 113° in Fankhauser et al.. This is mainly due to the inclusion of intra-articular fractures in our study. Our study had 32 patients out of 49 patients who achieved more than 90° of flexion, which constituted about 65.30% of patients. In the study conducted by Kolb et al. (2008) ,42 patients out of 50 patients achieved more than 90° (87%) [22]. This difference was mainly due to the inclusion of only intercondylar distal femur fractures in our study where gaining functional range of motion was a challenge even after good fixation. Our study had 21 patients with excellent results (42%), 18 patients had satisfactory results (36%), 7 patients had unsatisfactory results (14%), and 4 had poor results (8%). Anuj Agarwal et al. (2017) had taken all intercondylar fractures such as our study and they had 7 patients with excellent results among 12 patients (54%), 3 had good results (25%), and 2 had fair results (16%)[23]. Kolb et al. (2008) showed 15 patients with excellent results (48%), 10 patients with good results (32%), and 6 patients with fair results (20%). All these studies showed comparable results with good and excellent scores in almost 75% of cases, no matter whatever scoring system was used. In our study, two had non-union among 49 patients (4%) whereas Sahoo and Chand [24] showed three non-union among 34 patients (9%) suggesting that distal femur LCP is an excellent method of internal fixation. Borthakur et al. showed no cases of non-union. Ricci et al. (2014) showed that 64 patients among 335 patients had non-union and required reoperation (19%)[25]. Acharya et al. (2017) showed a 7% non-union rate[26]. Hoffman et al. (2013) showed 20 patients with non-union among 111 fractures (18%) [27]. Heather et al. (2006) showed six cases out of 46 patients who had non-union (13%)[28]. Our study had 8 open cases (16%) and 41 closed cases (84%) whereas Hoffman et al. (2013) showed 40% open cases and 60% closed cases. The rate of infection in our study was 14%. The intra-articular fractures with higher grade and more comminution , had poor result in terms of healing and range of motion. In our study, knee score was statistically not significant in terms of age, sex, mode of injury, open or closed fracture, any associated injury, or grade of fracture. However, the knee score was significantly reduced if there was a post-operative complication such as a surgical site infection. Knee stiffness was the most common complication postoperatively. In 1951, Delmore, West, and Schriber suggested fibrosis or arthrofibrosis after trauma as the prime cause of knee stiffness. In our study, we concluded that distal femoral LCP is the best method of fixation for distal femoral fractures which are supported by studies such as Yeap et al. (2007) [29] and Kolb et al. (2008). In our study, we observed that most of the patients were villagers with low education level. Facilities such as physiotherapy and rehabilitation centers were also lacking in their localities. Due to all these reasons, gaining post-operative functional range of motion was a difficult task to achieve. In our study, we observed that post-operative physiotherapy is one of the crucial steps of management protocol and only attaining a stable fixation and adequate reduction is not the answer for an excellent outcome. Educating the patient regarding the importance of regular physiotherapy was a tough job. It was seen that patients with good fixation but improper physiotherapy gave bad results in terms of functional outcome. On the contrary, patients with average reduction and fixation but regular exercises gave better results in terms of functional range of motion. High-speed vehicular accidents are responsible for distal femur fractures commonly observed in the young and middle-aged. Fractures of the distal femur in the elderly osteoporotic population especially women are attributed to low-energy mechanisms such as fall at home. Distal femoral fractures are often multifragmentary and/or intra-articular and are subjected to muscular forces that render non-operative treatment a poor option. These factors also place high demands on any surgical implant used to fix these fractures and may lead to failure. Pain, decreased range of motion, and compromised function of the knee joint are a common problem arising out of articular incongruity and improper fixation of articular fragments in such fractures. The preferred treatment for distal femur fractures is still distal femur locking plate. This study has several limitations. First, is the short follow-up period and lack of a control group. Therefore, a hospital-based case–control study to compare the clinical outcome between our techniques and the standard method with long-term follow-up is required in the future. Table 7 shows comparison of results of similar studies with the present study. Case 1-5.
- Fractures of the distal femur are more common in high-velocity injuries and occur in middle-aged males and old age women. Most fractures were comminuted. LCP appears to be technically an ideal implant for comminuted distal femoral fractures with proper physiotherapy producing excellent results
- Knee stiffness was the most common complication that we encountered in our series. Surgical site infection was also a common problem affecting the final functional outcome.
LCP appears to be more efficient for the treatment of distal femoral fractures both functionally and radiologically.
References
- 1.CoryA. Collinge and Donald A. Wiss; Title: Rockwood And Green's Fractures In Adults,7th Edition.2015 [Google Scholar | PubMed]
- 2.Robert H. Miller III • Frederick M. Azar; Campbell's Operative Orthopaedics 12th edition Volume 3. 2017. [Google Scholar | PubMed]
- 3.Surgical treatment of displaced, comminuted fractures of the distal end of the femur. RDMize, RW Bucholz and DP Grogan, Journal of bone and joint surgery Am .1982;64;871-879. [Google Scholar | PubMed]
- 4.Mize RD, Bucholz RW, Grogan DP. Surgical treatment of displaced, comminuted fractures of the distal end of the femur. J Bone Joint Surg Am 1982;64:871-9. [Google Scholar | PubMed]
- 5.Schatzker J, Home G, Waddell J. The Toronto experience with the supracondylar fracture of the femur, 1966-72. Injury 1974;6:113-28. [Google Scholar | PubMed]
- 6.Neer CS 2nd, Grantham SA, Shelton ML. Supracondylar fracture of the adult femur. A study of one hundred and ten cases. J Bone Joint Surg Am 1967;49:591-613. [Google Scholar | PubMed]
- 7.Kanakeshwar RB, Arun KC, Dheenadayalan J. Classification of distal femur fractures and their clinical relevance. Trauma Int 2016;2:3-6. [Google Scholar | PubMed]
- 8.Martin K. Zehntner, Dante G. Marchesi, Hansbeat Burch and Reinhold Ganz, "Allignment of Supracondylar/Intercondylar fractures of the femur after internal fixation by AO/ASIF technique", Journal of Orthopaedic Trauma 1992, Volume 6, No.3; p 318-326. [Google Scholar | PubMed]
- 9.Simonian PT, Thompson GJ, Emley W, et al. Angulated screw placement in the lateral condylar buttress plate for supracondylar femoral fractures. Injury. 1998; 29:101-104. [Google Scholar | PubMed]
- 10.Chauhan S, Dhanger SK, Singh BP. Study of surgical management of distal femur fracture using locking compression plate. Int J Orthop Sci 2021;7:921-5. [Google Scholar | PubMed]
- 11.Vishnu Vardhan N, Dhorababu T. Evaluation of functional outcome after open reduction and internal fixation of distal femur fractures by locking compression plate. Int J Orthop Sci 2021;7:9-13. [Google Scholar | PubMed]
- 12.Borthakur B, Hanse B, Haque R, Jindal S, Talukdar M. Results of locking compression plate fixation in distal femur fractures: A prospective study. J Med Thesis 2016;4:31-6. [Google Scholar | PubMed]
- 13.Rauf A, Iqbal MZ, Bhatti Z, Shafi MT. Outcome of distal femoral locking plate in supracondylar fracture of femur Muller type-A by MIPPO technique. J Sheikh Zayed Med Coll 2017;8:1281-3. [Google Scholar | PubMed]
- 14.Konuganti SR, Jakinapally SR, Rao VP, Rapur S. Management of distal femur fractures with locking compression plate: A prospective study. Int J Res Orthop 2018;4:208-13. [Google Scholar | PubMed]
- 15.Schuetz M, Müller M, Krettek C, Höntzsch D, Regazzoni P, Ganz R, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: A prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury 2001;32:SC48-54. [Google Scholar | PubMed]
- 16.Syed AA, Agarwal M, Giannoudis PV, Matthews SJ, Smith RM. Distal femoral fractures: Long-term outcome following stabilization with the LISS. Injury 2004;35:599-607. [Google Scholar | PubMed]
- 17.Fankhauser F, Gruber G, Schippinger G, Boldin C, Hofer HP, Grechenig W, et al. Minimal-invasive treatment of distal femoral fractures with the LISS (Less Invasive Stabilization System): A prospective study of 30 fractures with a follow up of 20 months. Acta Orthop Scand 2004;75:56-60. [Google Scholar | PubMed]
- 18.Wong MK, Leung F, Chow SP. Treatment of distal femoral fractures in the elderly using a less-invasive plating technique. Int Orthop 2005;29:117-20. [Google Scholar | PubMed]
- 19.Kapil Mani KC, Vaishya R, Dirgha Raj RC. Distal femoral fractures fixed by distal femoral locking compression plate: Functional outcomes and complications. Apollo Med 2018;15:142-6 [Google Scholar | PubMed]
- 20.Vallier HA, Hennesy TA, Sontich JK, Patterson BM. Failure of LCP condylar plate fixation in the distal part of the femur. A report of six cases. J Bone Joint Surg Am 2006;88:846-53. [Google Scholar | PubMed]
- 21.Kayali C, Agus H, Turgut A. LISS: Successful results of minimally invasive surgery for comminuted supracondylar femoral fractures with LISS: Comparative study of multiply injured and isolated femoral fractures. J Orthop Sci 2007;12:458-65. [Google Scholar | PubMed]
- 22.Kolb W, Guhlmann H et al. Fixation of Distal Femoral Fractures With the Less Invasive Stabilization System: A Minimally Invasive Treatment With Locked Fixed-Angle Screws. The Journal of Trauma, Injury, Infection, and Critical Care; Volume 65, Number 6: 1425-1434. [Google Scholar | PubMed]
- 23.Anuj agarwal, Vivek kiyawat et.al(2017) described complex AO type C3 fracture of distal femur managed by lateral locking plate by modified swashbuckler approach in 12 patients. The clinical outcome at 1 year was determined using the Knee Society Score (KSS). [Google Scholar | PubMed]
- 24.Sahoo BS, Chand DK. Distal femur fracture fixation by LCP-2 year experience. Int J Orthop Sci 2017;3:814-8. [Google Scholar | PubMed]
- 25.William M. Ricci, Philipp N. Streubel, Saam Morshed, Cory A. Collinge, Sean E. Nork and Michael J. Gardner. Risk Factors for Failure of Locked Plate Fixation of Distal Femur Fractures: An Analysis of 335 Cases. J Orthop Trauma 2014;28:83-89. [Google Scholar | PubMed]
- 26.Acharya KN, Rao MR. Retrograde nailing for distal third femoral shaft fractures: a prospective study. J Orthop Surg (Hong Kong) 2006;14:253-8. [Google Scholar | PubMed]
- 27.Martin F Hoffmann, Clifford B Jones, Debra L Sietsema, Paul Tornetta III and Scott J Koenig. Clinical outcomes of locked plating of distal femoral fractures in a retrospective cohort. Journal of Orthopaedic Surgery and Research; 2013, 8:43. [Google Scholar | PubMed]
- 28.Heather A. Vanier, Theresa A. Hennesy, John K Sontich and Brendan M Patterson. Failure of LCP condylar plate fixation in the Distal Part of Femur- a Report of six cases." The Journal of Bone and Joint Surgery,2006. 88:846¬853. [Google Scholar | PubMed]
- 29.EJ Yeap, AS Deepak. Distal Femoral Locking Compression Plate Fixation in Distal Femoral Fractures: Early Results. Malayasian Orthopedic Journal 2007; Volume I: p12-17. [Google Scholar | PubMed]






