Identification and treatment of mycobacterium avium complex musculoskeletal infection in a patient with no previous trauma or immunocompromised state.
Dr. Eric Taris, Department of Orthopedic Surgery, East Tennessee State University, James H Quillen College of Medicine, Johnson City, Tennessee, USA. E-mail: Tarises@midlandu.edu
Introduction: Mycobacterium avium complex (MAC) musculoskeletal (MSK) involvement is a rare clinical presentation of the upper extremity. When MSK involvement does occur, hand and wrist involvement are the most often reported due to the rich synovial fluid environment in these regions. This report describes an unusual case of tenosynovitis of the hand, in which a patient presented with a prolonged course of wrist pain due to MAC.
Case Report: An 87-year-old Caucasian, right-handed female presented with a 2-year history of right wrist pain and swelling. There had been no previous trauma or immunocompromised state. The patient was hospitalized for severe pneumonia 2 years ago, with wrist pain developing in the months after discharge. The treatment course included radical synovectomy and subsequent triple antibiotic therapy upon confirmation of MAC rice bodies. Due to advanced age and worsening dementia, the patient did not follow-up until 2 years post-operatively. Upon return at 2 years postoperatively, the patient had concerns of recurrent tenosynovitis. Treatment was declined by the family at this time and the patient did not return again until 5 years postoperatively with continued worsening tenosynovitis. Repeat synovectomy was suggested; however, additional treatment was held by the family due to the patient’s cognitive decline.
Conclusion: The aim of this report is to describe an atypical presentation of MAC-induced tenosynovitis. Patients diagnosed with a MAC infection should be treated promptly and informed of the possibility of recurrence. The goal of this report is to encourage practitioners to keep MAC infection on their list of differentials when evaluating abnormal wrist swelling.
Keywords: Mycobacterium avium Complex, granulomatous tenosynovitis, volar wrist.
Mycobacterium avium complex (MAC) musculoskeletal (MSK) involvement is a rare clinical presentation of the upper extremity. When MSK involvement does occur, hand and wrist involvement are the most often reported [1]. The rich synovial fluid environment in these regions creates a medium for the mycobacteria [2, 3]. The extensor and flexor tendon sheaths have an inner visceral layer and an outer parietal layer. Normally, these layers abut one another, but this potential space is rich with synovial fluid, proving to be an ideal environment for infections such as MAC. Tenosynovitis due to bacterial infection may develop through one of three mechanisms: (1) trauma with direct inoculation, (2) contiguous spread from adjacent infected tissues, and (3) hematogenous spread [4, 5, 6]. Of the reported MSK mycobacterial infections, the vast majority attribute it as a result of direct contact or trauma [7]. Diagnosis of a MAC infection is accomplished through a thorough history and physical exam, radiographs, Computed tomography/Magnetic resonance imaging (MRI) scan, and laboratory testing. The necessary laboratory tests include acid-fast bacillus staining and cultures in a Lowenstein-Jensen medium. Mycobacterial cultures are notoriously burdensome because MAC grows very slowly, taking 4–6 weeks for proper inoculation and growth. Diagnosis of suspected soft tissue infection secondary to MAC requires biopsy and positive culture. First line initial treatment of MAC infections is a three-drug regimen consisting of a macrolide, rifampin, and ethambutol. This treatment regimen should be prescribed for 1 year [3, 8, 9]. When MAC presents as an MSK infection, performing a tenosynovectomy/synovectomy will not realistically remove all infected tissue. However, it does decrease the diseased tissue load and provide improved pharmacologic therapy to the remaining infected tissue, allowing a better chance of resolution. Here, we discuss the initial presentation, treatment course, and outcome of an 87-year-old woman with MAC tenosynovitis of the right volar wrist.
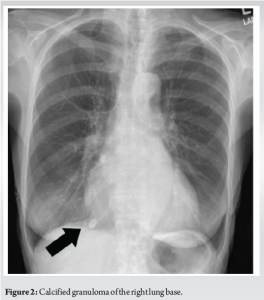
An 87-year-old right-hand-dominant Caucasian female presented to the Orthopedic Hand Clinic with a 2-year history of right wrist pain and swelling, denying any previous traumas or injuries to her wrist. Two years ago, the patient was hospitalized for a severe case of pneumonia. In the following months, the patient noticed right wrist discomfort which she described as throbbing with occasional sharp pains. Bracing, NSAIDs, and tramadol provided by her primary physician failed to resolve her symptoms. Radiographs and MRIs were obtained before she presented to the clinic. Radiographs revealed chondrocalcinosis of the wrist and first CMC joint osteoarthritis. The MRI showed extensor and flexor tenosynovitis with rice bodies and cystic changes (Fig. 1). The patient also had previous chest X-rays which revealed a calcified granuloma of the right lung base (Fig. 2). Her past medical history and review of symptoms were noncontributory, and she was not immunocompromised.

A physical exam of the right hand revealed non-tender, boggy swelling of the volar wrist measuring 8 cm × 5 cm just proximal to the wrist crease. The dorsal wrist swelling measured 4 cm × 2 cm and was localized over the 5th and 6th extensor compartments.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were elevated at 51 and 16.8, respectively. The patient’s laboratory work including complete blood count (CBC), complete metabolic panel, creatine phosphokinase, uric acid, and basic rheumatoid panel were negative.
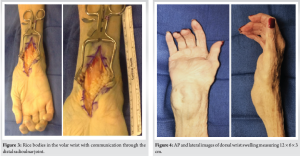
The patient was scheduled for radical synovectomy of both the dorsal and volar wrists. At the time of surgery, the patient’s differential was chondrocalcinosis versus an atypical bacterial infection. Surgery was planned on an outpatient basis. During surgery, rice bodies were found at the volar and dorsal wrist with communication of the rice bodies through the distal radioulnar joint (Fig. 3). There was thickening of the volar flexor forearm compartments in the wrist and palm. The median nerve was intact but flattened and hypervascular. Dorsally, there was thickening of the extensor carpi ulnaris tendon sheath. Approximately 10–15 mL of rice bodies were excised. Synovectomy was performed of all thickened synovium, which was ensured by meticulous inspection and removal of all visible synovial tissue throughout the joint using direct visualization. The right carpal tunnel was released. Specimens were sent for fungus cultures, acid-fast bacilli stains, anaerobic/aerobic cultures, and Lowenstein-Jensen medium cultures were sent for processing.
Initial laboratory results for fungus cultures, acid-fast bacilli stain, and anaerobic and aerobic cultures were negative. Lowenstein-Jensen medium cultures came back positive 4 weeks later for Mycobacterium avium intracellular complex. The infectious disease team started the patient on Ethambutol 400 mg, Rifabutin 150 mg, and Clarithromycin 500 mg for 1 year. The patient was seen back in the clinic roughly 2 years after surgery with concerns of recurrent tenosynovitis. The patient had a painless, boggy swelling that measured 6 cm × 5 cm × 3 cm. Repeat synovectomy was discussed, however the patient had progressive dementia and poor health. Due to the patient’s low demand on her hands, it was decided to treat the patient conservatively. Roughly 5 years after surgery, the patient was seen in the clinic again. The area of swelling was found to be 12 cm × 6 cm × 3 cm (Fig. 4). An MRI was obtained and showed a large collection of synovial fluid at the wrist (Fig. 1). At this time the patient had worsening dementia and poor health conditions unrelated to her MAC hand infection. The decision was made by the family to continue conservative management. This marked the past visit with the patient.
We present a rare case of granulomatous tenosynovitis caused by Mycobacterium intracellulare in a patient without reported trauma or inoculation, who initially presented with a history of pneumonia. Only ~5–10% of patients that present with atypical mycobacterial infection endorse MSK involvement [10]. In addition, atypical mycobacterial pneumonia is rare in the immunocompetent [1, 11, 12]. The lack of trauma/inoculation, lack of immunocompromise, pneumonia preceding the wrist pain, and recurrence makes the case unique. The diagnosis of atypical mycobacterial tenosynovitis is often delayed. The length of time between the presence of symptoms and diagnosis averages a year or more [7]. Extensive history-taking and astute clinical awareness are vital to diagnosis. Occupational/recreational exposure is important to identifying the specific species of mycobacterium. For example, aquatic exposure has been evident in nearly all patients infected with Mycobacterium marinum, and farm exposure in patients infected with Mycolicibacter terrae [7]. Chronic hand infections are easily misdiagnosed for other conditions which are more common and have similar presentations. Examples of these similar conditions include rheumatoid arthritis, psoriatic arthritis, gout, pseudo gout, herpes zoster, de Quervain tenosynovitis, and giant cell tumor of the tendon sheath [1, 13, 14]. Some of these diagnoses may be treated with anti-inflammatories or local steroid injections. Intralesional steroid injections are contraindicated in atypical infections because of the risks of aggravating the infection. Initial laboratory workup often includes CBC, CRP, ESR, RF, and diagnostic imaging. Physical signs of infection are usually absent and blood tests are generally not helpful. Imaging plays a key role in narrowing down potential diagnoses. Both MRI and sonography can reveal the presence of rice bodies [1]. Rice bodies are small white granules resembling grains of polished rice composed of acidophilic collagenous centers encased in fibrin (Fig. 3) [13]. The presumption is that they are from microvascular infarcts of the joint synovium that then become encased in layers of fibrin afterward. Others believe they are caused by fibroblast activation leading to the formation of collagen, which later becomes encased in fibrin. Inflammatory conditions often associated with rice-body formation include rheumatoid arthritis, seronegative inflammatory arthritis, tuberculous joints, juvenile arthritides, and chronic bursitis [1, 13, 14]. With an accurate diagnosis, appropriate treatment can be obtained by patients. The effectiveness of combined surgical debridement and antimicrobial therapy in resolving atypical mycobacterial infection of the upper extremity has been studied. Results are varied given the sparse body of literature covering these infections. Current studies have shown a recurrence rate of 13–50% after tenosynovectomy and appropriate antimicrobial therapy [15,16]. Finally, a retrospective review reports two of seven patients ultimately requiring amputation due to recurrence of infection [17]. In the unfortunate circumstance of recurrence, the treatment plan could be repeated debridement and adjusted pharmacotherapy for increased duration. If infection continues to progress, decisions regarding ablative techniques or amputation should be addressed [3, 14, 18, 19].
This report presented an 87-year-old woman with MAC infection of her volar wrist. The aim of our report is to share a unique case presentation/course of recurrent atypical mycobacterial tenosynovitis and bring attention to atypical hand infections as a cause of chronic hand swelling. Patients diagnosed with a MAC infection should be informed of the possibility of recurrence. The treatment for recurrence includes conservative treatment, repeated surgeries, alterations in pharmacological treatment, and in aggressive cases, amputation. MSK infections due to MAC are exceedingly rare and difficult to treat, emphasizing the need for awareness of this pathology. Our report serves to provide an example for the presentation and treatment for MAC infections for providers to use as a framework for care in the future.
MSK infection secondary to MAC is a rare cause of granulomatous tenosynovitis in the volar wrist. This presentation is increasingly complicated by the lack of prior trauma, inoculation, or hematogenous spread in this patient. This case demonstrates the need to consider MAC as a source of infection in the differential for atypical hand infections.
References
- 1.Chau CL, Griffith JF, Chan PT, Lui TH, Yu KS, Ngai WK. Rice-body formation in atypical mycobacterial tenosynovitis and bursitis: Findings on sonography and MR imaging. AJR Am J Roentgenol 2003;180:1455-9. [Google Scholar]
- 2.Falkinham JO 3rd. Epidemiology of infection by nontuberculous mycobacteria. Clin Microbiol Rev 1996;9:177-215. [Google Scholar]
- 3.Kaji Y, Nakamura O, Yamaguchi K, Nomura Y, Oka K, Yamamoto T. Combined administration of rifampicin, ethambutol, and clarithromycin for the treatment of tenosynovitis of the hand caused by Mycobacterium avium complex: Case series and literature review. Medicine (Baltimore) 2021;100:e25283. [Google Scholar]
- 4.Small LN, Ross JJ. Suppurative tenosynovitis and septic bursitis. Infect Dis Clin North Am 2005;19:991-1005, xi. [Google Scholar]
- 5.Gonzalez MH, Garst J, Nourbash P, Pulvirenti J, Hall RF Jr. Abscesses of the upper extremity from drug abuse by injection. J Hand Surg Am 1993;18:868-70. [Google Scholar]
- 6.Chin KR, Miller BS, Koris MJ. Serous flexor tenosynovitis as an associated finding in meningococcal septic polyarthritis. Am J Orthop (Belle Mead NJ) 2002;31:88-9. [Google Scholar]
- 7.Kozin SH, Bishop AT. Atypical Mycobacterium infections of the upper extremity. J Hand Surg Am 1994;19:480-7. [Google Scholar]
- 8.Daley CL, Iaccarino JM, Lange C, Cambau E, Wallace RJ Jr., Andrejak C, et al. Treatment of nontuberculous mycobacterial pulmonary disease: An official ATS/ERS/ESCMID/IDSA clinical practice guideline. Clin Infect Dis 2020;71:e1-36. [Google Scholar]
- 9.Haworth CS, Banks J, Capstick T, Fisher AJ, Gorsuch T, Laurenson IF, et al. British thoracic society guidelines for the management of non-tuberculous mycobacterial pulmonary disease (NTM-PD). Thorax 2017;72:i1-64. [Google Scholar]
- 10.Jiang L, Chiou H, Wu H, Wang H, Lai Y, Chou Y. Nontuberculous mycobacterial tenosynovitis: A case report and review of the literature. J Med Ultrasound 2015;23:199-203. [Google Scholar]
- 11.Zenone T, Boibieux A, Tigaud S, Fredenucci JF, Vincent V, Chidiac C, et al. Non-tuberculous mycobacterial tenosynovitis: A review. Scand J Infect Dis 1999;31:221-8. [Google Scholar]
- 12.Armstrong P, Wilson A, Dee P, et al. AIDS and other forms of immunocompromise. Imaging Dis Chest 2000;3:258-9. [Google Scholar]
- 13.Edison MN, Caram A, Flores M, Scherer K. Rice body formation within a peri-articular shoulder mass. Cureus 2016;8:e718. [Google Scholar]
- 14.Kwan M, Tupler R. Recurrent nontuberculous mycobacterial tenosynovitis. Ochsner J 2021;21:86-9. [Google Scholar]
- 15.Huayllani MT, Sisti A, Boczar D, Restrepo DJ, Parker AS, Sarabia-Estrada R, et al. Chronic tenosynovitis of the upper extremities caused by Mycobacterium kansasii: A clinical case and systematic review of literature. Indian J Plast Surg 2020;53:25-35. [Google Scholar]
- 16.Aubry A, Chosidow O, Caumes E, Robert J, Cambau E. Sixty-three cases of Mycobacterium marinum infection: Clinical features, treatment, and antibiotic susceptibility of causative isolates. Arch Intern Med 2002;162:1746-52. [Google Scholar]
- 17.Aryee JN, Akinleye SD, Ugwu-Oju OC, Moore CC, Freilich AM. A Series of Nontuberculous mycobacterial flexor tenosynovitis infections and cost of treatment. J Wrist Surg 2021;10:511-5. [Google Scholar]
- 18.Smidt KP, Stern PJ, Kiefhaber TR. Atypical mycobacterial infections of the upper extremity. Orthopedics 2018;41:e383-8. [Google Scholar]
- 19.Wells D, Strickland C, Schowinsky J, Lindeque B. Nontuberculous mycobacterial tenosynovitis: AIRP best cases in radiologic-pathologic correlation. Radiographics 2015;35:493-7. [Google Scholar]