This case outlines the complications that are at risk during a hip fusion takedown to total hip arthroplasty and highlights important considerations to incorporate in a revision plan if complications arise
Dr. Samuel G Eaddy, Mercy Health St. Vincent Medical Center, Department of Orthopedics and Sports Medicine, 2409 Cherry Street, Suite #10, Toledo - 43608, Ohio, United States. E-mail: eaddy.sam@gmail.com
Introduction: Spontaneous hip fusion is a multifactorial condition that can cause drastic functional limitations. Total hip arthroplasty (THA) can provide symptomatic improvement but leads to high rates of instability, dislocation, and revision.
Case Report: A 66-year-old woman with a long-standing history of dysplastic and spontaneously fused left hip received a fusion takedown to primary THA. She subsequently dislocated with catastrophic acetabular cup failure necessitating revision THA. She reports no pain or dislocations at 12 months post-revision.
Conclusion: Deciding to perform THA for spontaneous hip fusion should consider clinical benefit alongside increased risks of dislocation and revision. Patients with acetabular dysplasia and longer durations of fusion are at an increased risk, due to skewed anatomic landmarks, weak abductors, and altered spinopelvic parameters. However, in the case of primary THA failure, revision surgery can provide satisfactory benefits.
Keywords: Hip fusion, hip arthrodesis, hip fusion takedown, total hip arthroplasty, hip dislocation.
Spontaneous fusion of the hip is a multifactorial process of joint ossification that often results in a stable, painless hip. Regardless of the cause, a fused hip can lead to multiple debilitating complications, including degenerative changes in adjacent joints, gait disturbances, instability, and leg-length discrepancy [1,2]. Primary total hip arthroplasty (THA) can provide functional improvement, patient satisfaction, and relief of ipsilateral knee and back pain caused by altered gait mechanics [3,4]. Complications and revisions are not uncommon, especially as these patients often have chronic illnesses associated with the fused hip. In this study, we report the case of a woman with a long-standing auto fusion of her left hip, managed initially with THA, who subsequently suffered dislocation with catastrophic acetabular cup dislodgement upon a closed reduction attempt in the emergency room. She received revision THA with satisfactory results. The patient provided written informed consent before writing this manuscript.
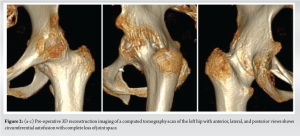
A 66-year-old female presented to our clinic with painless, limited range of motion (ROM) in her left hip, and pain in her left knee that had begun to affect her daily activities. She first noticed limitations in ROM in her early 30s and she reported that by age 40, her ROM was essentially zero. Past medical history also included bilateral knee arthritis and daily tobacco use. She reported having her hip examined as a child but did not recall receiving a formal diagnosis. Physical examination revealed increased lumbar lordosis during ambulation with compensatory hip hiking, left leg shortening with a hip internal rotation, and flexion contracture with no active and passive hip ROM. A pelvic radiograph revealed left hip fusion, severe dysplasia, and complete obliteration of the joint space (Fig. 1). Review of prior radiographs revealed arthritic changes in her left knee as well. Computed tomography (CT) reconstruction was performed to evaluate the patient’s acetabular bone stock and native femoral version, demonstrating a thinned native posterior wall and increased femoral anteversion compared to the contralateral hip (Fig. 2). The patient consented to undergo hip fusion takedown to primary THA to regain hip ROM.

A direct anterior approach (DAA) utilizing an anterior minimally invasive surgery table (Medacta, Castel San Pietro, Switzerland) was performed for the index procedure. Intraoperatively, her abductors appeared intact but moderately atrophic. An in situ femoral neck napkin ring cut was made 1.5 cm proximal to the lesser trochanter. Reaming the acetabulum required advancing through the fused femoral head under live fluoroscopy with the addition of palpation and visual inspection of the acetabular walls. Final implants included a 62 mm multi-hole acetabular shell secured with five screws, a neutral lip liner, and a cementless size 4 femoral stem with a 40 mm standard head (Fig. 3). Intraoperative fluoroscopy showed restoration of leg length and offset, and the hip was stable throughout the arc of ROM. There were no intraoperative or perioperative complications, and she was discharged home weight-bearing as tolerated with anterior hip precautions on post-operative day 2.

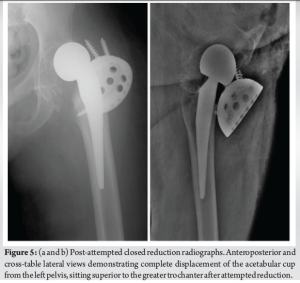
On post-operative day 7, the patient presented to the emergency department following a “stretching” pain sensation while rising from a chair. On examination, the left leg was abducted, externally rotated, and shortened approximately two inches. Her neurovascular status was normal. Radiographs revealed anterior-superior dislocation of the prosthetic femoral head (Fig. 4). Attempts at closed reduction under procedural sedation by an orthopedic surgery resident were unsuccessful. Subsequent radiographs demonstrated complete acetabular cup dislodgement superior to the greater trochanter (Fig. 4,5). No acute fractures were noted. The patient then consented to revision THA the following morning. A direct lateral approach was utilized for the revision surgery. The acetabular cup was entrapped within the intramuscular area of the abductors, causing an intrasubstance tear and partial avulsion from the greater trochanter. Acetabular and femoral components were removed without fractures, and the acetabular wall was reamed to medialize the socket and avoid further posterior-superior bone loss. A Trabecular Metal Acetabular Revision System (Zimmer-Biomet, Warsaw, IN, USA) was implanted, including a 54 mm buttress and shim augment secured with five screws, a 58 mm multihole shell secured with three posterior-superior screws, and a dual mobility cup (28 mm head and 46 mm liner). A 150 mm Arcos® Modular Femoral Revision System stem (Zimmer-Biomet) was utilized to adjust appropriate femoral anteversion. After the abductors were repaired, her hip appeared stable throughout ROM. Her immediate post-operative course was uneventful. Of note, prophylaxis for heterotopic ossification (HO) was not prescribed. She worked with physical therapy on gentle mobility exercises. She was discharged home on post-operative day 4 with anterior hip precautions and the use of an abduction pillow for 6 weeks while sleeping. She remained toe-touch weight-bearing on the left leg for 6 weeks to further protect the acetabulum revision. Formal physical therapy and full weight-bearing began at 6 weeks. The patient reported no pain and did not experience further dislocations at subsequent follow-up visits. At 12 months, her total Hip Harris Score was 75 points (out of 100). She ambulated without a Trendelenburg gait and used a cane for longer distances. Hip ROM showed 90° flexion, 29° abduction, 28° adduction, 35° external rotation, and 5° internal rotation. Radiographs showed maintained alignment of all components with no signs of loosening (Fig. 6). There was radiographic evidence of HO without pain or functional limitations. The patient was seen again at 2 years and 10 months post-operative and was doing well overall without complication. Her Hip Harris Score had improved to 84 points, and her 12-item Short Form Survey score was above average at 51 for physical health and 62 for mental health (50 being average for each). Hip ROM was 90° flexion, 35° abduction, 30° adduction, 35° external rotation, and 15° internal rotation. At this time she complained of worsening contralateral knee pain related to pre-existing arthritis. She ambulated with a cane primarily due to severe valgus deformity of the right knee; however, her left leg gait cycle was steady with improved left hip ROM compared to before her index procedure (Supplemental Video 1). Final radiographs redemonstrated a stable prosthesis without further development of HO (Fig. 7). Despite her eventful clinical course, the patient was satisfied with her decision to undergo initial THA due to the improved ROM it ultimately provided.


Hip fusion takedown to primary THA is an uncommon, challenging procedure that can provide functional improvement and satisfaction in patients with a spontaneously fused hip [2,3,5]. The challenge should not be underestimated, as this disease process has significantly higher risks of complications than those seen in primary THA procedures for osteoarthritis. Developmental dysplasia of the hip (DDH) is a common cause of spontaneous hip fusion, and this patient’s history and radiography suggest this to be her likely pathology. Acetabular dysplasia is an independent risk factor for malpositioning of acetabular components during primary THA, largely because it skews traditional landmarks for cup placement [6]. It is important to be cautious when reaming through a fused femoral head to avoid over-reaming eccentrically, which may lead to acetabular wall compromise. For patients with chronic hip pathology, especially DDH, pre-operative CT imaging can be helpful in evaluating bone stock and assessing whether bone grafting, augments, or further revision components should be utilized. While this patient had a thinned posterior acetabular wall on CT, it was felt that the bone stock was strong enough to support the primary implants. Long-standing hip fusion also causes biomechanical alterations that can complicate THA procedures, with abductor pathology and spinopelvic alterations being two major consequences. Longer durations of hip fusion lead to increased hip abductor atrophy due to disuse, which has been shown to cause worse outcomes following hip fusion takedown to primary THA [4]. The main mechanism for poor outcomes is due to abductor weakness resulting in a loss of essential stability that they normally provide. This is an important consideration, because abductor pathology is especially common after THA for hip fusion [2]. Methods to help mitigate instability in patients with abductor dysfunction include increasing femoral offset to tension the abductors and using a dual mobility cup or constrained liner in more severe cases. For complete loss of abductor attachment, whiteside [7] described a gluteus maximus transfer technique to reinforce the abductor complex, which can restore abductor function with high success rates. Gait adaptations and altered spinopelvic biomechanics, including increased pelvic tilt and relative lumbar lordosis, are also common time-dependent consequences of long-standing fusion [1]. These compensatory mechanisms can decrease the acetabular version and reduce the accuracy of cup placement, which further complicates the distorted anatomy in patients with pre-existing dysplasia. Pre-operative evaluation of the spinopelvic relationship with a full spinopelvic radiographic series may therefore optimize the cup version. Furthermore, Vigdorchik et al. [8] describe a simple hip-spine classification for preoperatively evaluating a spinopelvic relationship, which reduces the risk of dislocation in high-risk patients. Hip dysplasia, abductor weakness, and altered spinopelvic biomechanics all have implications for causing instability after THA. The major, feared consequence of instability is THA dislocation because it often requires revision surgery. Jauregui et al. [2] performed a systematic review of 27 studies with 1104 THA procedures for hip fusions (351 for spontaneously fused hips) and found that 1.7–4.2% of patients experienced instability, leading to a dislocation rate of up to 15.4%. They also found a weighted average 10-year revision rate of 12%, a rate that would be considered unacceptable for primary THA. Following a single THA dislocation without an identifiable cause, closed reduction may be effective. Adequate sedation is crucial; as undersedation during THA reduction is associated with worse patient outcomes, [9] and many of these cases may benefit from formal anesthesia. Recurrent dislocations are common, making revision THA an appropriate treatment option, especially if a mechanical cause of instability is identified. In cases with symptomatic cup loosening or frank dislodgement, revision of THA is necessary. The choice of the THA approach with hip fusion takedowns should depend on surgeon familiarity, but the DAA has shown excellent prosthesis positioning and faster early post-operative recovery compared to the posterolateral approach [10]. Emphasizing hip precautions may benefit these patients, even though recent trends in DAA have moved toward activity as tolerated with no immediate precautions. More recent evidence suggests that robotic-assisted THA can improve acetabular reaming and component placement in a spontaneously fused hip [11]. There is similarly no clear consensus on optimal implants, but larger head sizes are generally considered more stable. Cementless stems show excellent long-term survival rates for patients with hip fusion receiving primary or conversion THA [3]. A dual mobility construct is a reasonable choice to minimize the risk of dislocation in revision THA. For persistent instability following dual mobility THA, a revision-constrained acetabular liner may provide an improved salvage solution [5]. In cases with severe posterior/superior acetabular bone loss, buttress augments can effectively substitute the use of structural allographs and provide positive outcomes [12]. Finally, prophylaxis for HO should be considered. This patient was not prescribed HO prophylaxis and developed evidence of HO on radiographs at 1 year. Ayekoloye et al. [5] documented 39 hip fusion takedowns to THA, with 10 patients developing HO, three of whom required excision. However, all patients in this cohort received HO prophylaxis with celecoxib for 3 weeks. Further investigation into the utility of HO prophylaxis is needed to provide clearer guidelines for these procedures. Areas of future research for both primary and revision THA for patients with spontaneous hip fusion should include abductor reconstruction; acetabular reaming with respect to version and poor anatomic landmarks; approaches providing adequate exposure; navigation and robotics; and utilization of stable implants and augments when necessary. Future surgical considerations for this procedure should include an emphasis on templating, advanced imaging, implant choice, and surgical approach to provide better clinical guidelines that incorporate modern surgical advancements. The benefit of HO prophylaxis remains unclear, which warrants further research.
Hip fusion takedown to THA is a technically challenging procedure that requires an understanding of patient risk factors. Attention should be given to the cause and duration of fusion, especially due to how these affect the hip stabilizers and spinopelvic relationship. Thorough patient education should convey the increased dislocation and revision rates to obtain fully informed consent. In cases of THA dislocation, revision arthroplasty principles described here can provide satisfactory long-term results.
It is essential for orthopedic surgeons to understand the increased risks of complications associated with hip fusion takedown to THA, especially in patients with long-standing fusion, acetabular dysplasia, and tenuous abductors.
References
- 1.Thambyah A, Hee HT, Das De S, Lee SM. Gait adaptations in patients with longstanding hip fusion. J Orthop Surg (Hong Kong) 2003;11:154-8. [Google Scholar | PubMed]
- 2.Jauregui JJ, Kim JK, Shield WP 3rd, Harb M, Illical EM, Adib F, et al. Hip fusion takedown to a total hip arthroplasty-is it worth it? A systematic review. Int Orthop 2017;41:1535-42. [Google Scholar | PubMed]
- 3.Celiktas M, Kose O, Turan A, Guler F, Ors C, Togrul E. Conversion of hip fusion to total hip arthroplasty: Clinical, radiological outcomes and complications in 40 hips. Arch Orthop Trauma Surg 2017;137:119-27. [Google Scholar | PubMed]
- 4.Joshi AB, Markovic L, Hardinge K, Murphy JC. Conversion of a fused hip to total hip arthroplasty. J Bone Joint Surg Am 2002;84:1335-41. [Google Scholar | PubMed]
- 5.Ayekoloye CI, Abu Qa’oud M, Radi M, Leon SA, Kuzyk P, Safir O, et al. Review of complications, functional outcome, and long-term survival following conversion of hip fusion to total hip arthroplasty. Bone Joint J 2021;103-B 7 Suppl B:129-34. [Google Scholar | PubMed]
- 6.Gromov K, Greene ME, Huddleston JI, Emerson R, Gebuhr P, Malchau H, et al. Acetabular dysplasia and surgical approaches other than direct anterior increases risk for malpositioning of the acetabular component in total hip arthroplasty. J Arthroplasty 2016;31:835-41. [Google Scholar | PubMed]
- 7.Whiteside LA. Surgical technique: Transfer of the anterior portion of the gluteus maximus muscle for abductor deficiency of the hip. Clin Orthop Relat Res 2012;470:503-10. [Google Scholar | PubMed]
- 8.Vigdorchik JM, Sharma AK, Buckland AJ, Elbuluk AM, Eftekhary N, Mayman DJ, et al. 2021 otto aufranc award: A simple hip-spine classification for total hip arthroplasty. Bone Joint J 2021;103-B 7 Supple B:17-24. [Google Scholar | PubMed]
- 9.Ryan SP, Hopkins TJ, Wellman SS, Jiranek WA, Bolognesi MP, Seyler TM. Undersedation during total hip arthroplasty reduction results in worse patient outcomes. J Arthroplasty 2019;34:3061-4. [Google Scholar | PubMed]
- 10.Dong J, Kong L, Zhang S, Shang X, Wang J, Zhang X, et al. Conversion of a fused or ankylosed hip to total hip arthroplasty: Is the direct anterior approach in the lateral decubitus position an ideal solution? Front Surg 2022;9:819530. [Google Scholar | PubMed]
- 11.Fu H, Yan CH, Cheung A, Cheung MH, Chan VW, Chan PK, et al. Robotic-Arm assistance simplifies hip arthrodesis conversion to total hip arthroplasty. Arthroplast Today 2020;6:877-87. [Google Scholar | PubMed]
- 12.Meneghini RM, Hull JR, Russo GS, Lieberman JR, Jiranek WA. Porous tantalum buttress augments for severe acetabular posterior column deficiency. Surg Technol Int 2015;27:240-4. [Google Scholar | PubMed]











