• The distal tibia, being subcutaneous, is very prone to wound complications after surgical exposure. • The distal tibia and fibula fractures can also be accessed using a single incision for plate fixation. • The single-incision approach is a reliable alternative to the dual-incision method.
Dr. SK Rai, Department of Orthopaedics, Military Hospital, Ambala, Haryana, India. E-mail: skrai47@yahoo.com
Introduction: Comminuted fractures of the distal end of the tibia and fibula usually occur due to high-velocity trauma, and the tibia, being subcutaneous in this area, is prone to wound healing risks and complications. Fixation typically involves two separate incisions, medial and lateral, which pose risks of wound healing complications and devascularization of the distal tibia. This study aims to present a novel single anterolateral incision approach for the internal fixation of distal tibia and fibula fractures to minimize soft-tissue complications.
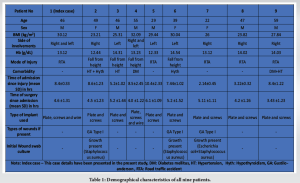
Case Report: Nine patients were treated with internal plate fixation for their comminuted fractures of the distal end of the tibia and fibula using a single-incision technique. The cohort included six male and three female patients, with a mean age of 31.8 years (range 17–59).
Conclusion: We present nine cases of comminuted fractures of the distal end of the tibia and fibula treated with a single-incision technique for internal plate fixation, resulting in satisfactory outcomes without any wound healing complications.
Keywords: Fracture, distal tibia, distal fibula, anatomy, incision.
Distal tibia fractures are invariably caused by high-energy impact, and it is associated with fibular fractures. Motor vehicle accidents, falls from heights, or twisting injuries typically generate the high-energy axial compressive force, direct bending, or low-energy rotational forces responsible for such fractures. Due to their nature, causes, limited soft-tissue coverage, and blood supply, these fractures frequently lead to non-union and soft-tissue complications. Rubio-Yanchuck et al [1]. The primary aim of treating tibial fractures is to enhance fracture stability without exacerbating soft-tissue problems through surgical intervention, which presents a significant challenge for distal tibial fractures. Surgical recommendations typically include open reduction and internal fixation (ORIF), external fixation, and intramedullary nailing, Kwan et al [2] . However, when rigid fibular fixation is necessary, the traditional approach involves two separate incisions: One lateral incision for the fibula and another anterolateral incision for the tibia. Unfortunately, these combined incisions often result in extensive soft-tissue dissection and periosteal injury, elevating the risk of deep infection and skin necrosis, particularly when the initial injury involves extensive soft-tissue damage and when the two incisions are not adequately spaced apart, Lee at el [3,4] Song et al. suggested minimally invasive plate osteosynthesis (MIPO) as an alternative technique to preserve soft-tissue integrity at the fracture site. [5] Consequently, various alternate methods have been suggested for the conservation of soft tissue at the location of the fracture. Recently, there has been a proposal to use a single-incision method for treating fractures in the distal tibia and fibula. [6-8] Multiple studies have assessed the practicality of this method and its implementation in clinical settings.[9-14] In the present study, we present nine cases of comminuted fractures of the distal end of the tibia and fibula using the single-incision technique and their outcomes.
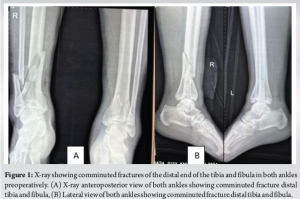
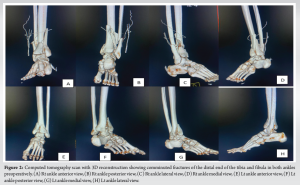
Our illustrated case involves a 46-year-old male patient without any medical comorbidities who was involved in a roadside accident and brought to our emergency department. There was no history of transient loss of consciousness after the accident. He presented with pain and swelling in both the leg and ankle regions without any wound, Physical evaluation revealed full consciousness and alertness, with stable vitals and no neurological deficits. Clinically, the abdomen and chest were normal. There was swelling around both ankles. Distal arterial pulsation was present, and no neurological deficit was detected clinically. A posterior slab was applied. (Fig 1 and 2). Radiologic studies were performed, revealing comminuted fractures of the distal end of the tibia and fibula in both ankles (Fig. 1, 2, Table 1).
Single-incision technique
Following the administration of spinal anesthesia, the patient was positioned supine. A cushion was placed under the hip on the same side as the operation to prevent outward rotation of the leg. The affected limb was inflated with a tourniquet and properly positioned. The tourniquet was applied for a maximum of 90 min and deflated before final closure.
A longitudinal anterolateral incision was made through the skin and subcutaneous tissues along the projection line of the extensor digitorum longus muscle, between the tibia and fibula, focusing on the fracture line in the distal leg. The incision extended just above the ankle joint, with potential proximal extension as needed for internal fixation placement. Initially, lateral retraction of the peroneus longus and brevis muscles exposed the fibular fracture. Depending on the fracture line location, treatment involved either a one-third tubular plate or a distal fibular anatomical locking plate (India-made plate). Careful exposure and relocation of the superficial peroneal nerve and extensor digitorum longus were performed together. Reduction was meticulously managed to achieve the desired tibial length. Subsequently, the tibialis anterior, extensor hallucis longus, and extensor digitorum longus muscles were collectively displaced laterally at the fracture’s upper portion. The tibialis anterior and deep peroneal nerves were repositioned centrally to expose the distal tibia, as depicted in Fig. 3.
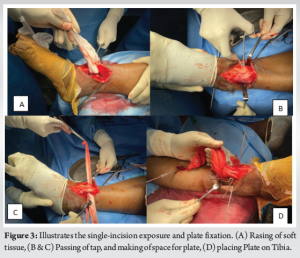
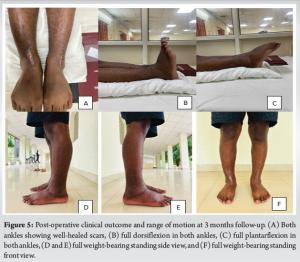
Once the fractured tibia was successfully aligned, a specialized anterolateral L-anatomical locking plate was used to stabilize the lateral side of the tibia (Fig. 4. Intravenous antibiotics were administered for 48 h post-surgery. Physiotherapy followed, and patients were discharged 2 weeks after suture removal. Demographic characteristics of all nine patients are detailed in Table 1. The final outcome has been shown in Fig. 5

The comminuted fracture distal tibial is invariably associated with soft-tissue complications, which can contribute to wound dehiscence, infection, and delayed union/non-union of fractures, representing a significant problem in the surgical treatment of fractures of the distal third of the tibia and fibula Höiness P et al [15]. The most effective treatment for distal tibial fractures is currently a subject of debate, Vallier HA [16] and Mair O, et al [17]. Recent studies have compared different methods for treating distal tibial fractures [18,19]. The three primary treatment modalities are ORIF, MIPO, and intramedullary nail (IMN) treatments. Several studies have shown that using IMNs reduces the risk of wound complications and leads to superior functional improvement of the ankle compared to ORIF and MIPO [19,20]. Hu et al. suggested that ORIF appears to offer more benefits in achieving anatomical alignment and reducing knee discomfort [19]. The study examined the possibility of using the MIPO method or IMN for some cases. Ma et al. [20] recorded that anterolateral plating through a single incision in ORIF offers the benefits of achieving anatomical alignment and fixation. Similarly, Femino and Vaseenon [21] suggested various benefits of the single-incision approach, such as direct exposure of the fracture site, preservation of the angiosomes of the skin in the front part of the ankle area, and maintaining the entire layer of soft-tissue covering the lower part of the tibia. This single incision enables the internal fixation to be fully covered when the wound is closed. Using this single incision, the tibial lateral column and syndesmosis can be directly observed and realigned, and the superficial peroneal nerve can be dissected and protected. The dual-incision method is commonly employed because it provides a clear view and allows for direct handling. Nevertheless, the single-incision technique can also be used for fractures occurring in the lower third of the tibia and fibula, particularly in cases classified as A1, A2, B1, and C1 distal tibial fractures, as well as Type C1 fibular fractures, according to the AO classification system, Shantharam et al. [8] Our study found that a single-incision method can be used to treat all sorts of distal tibial and fibular fractures in the AO classification. Furthermore, numerous studies have assessed the practicality of implementing this method in a clinical setting [8,12]. Shantharam et al. [6] initially suggested the possibility of using a single-incision method to treat fractures, whereas Yu et al. [8] examined the anatomical foundation of an anterolateral approach for the distal tibia and fibula. Their measurements revealed a clear separation between muscles and nerves in the front and side of the lower leg, and using a single incision might prevent damage to the main blood vessels and nerves. Our technique found that the single-incision method provided sufficient visibility for subsequent surgeries. In addition, the superficial/deep peroneal nerve and anterior tibial arteries were clearly delineated that reduces the chance of injury.
The anterior single-incision approach to the distal tibia and fibula is a beneficial surgical technique involving a single incision in the skin. This approach is often utilized for promptly treating and stabilizing fractures in the distal fibula. This method acknowledges and protects the angiosomes of the skin in the front ankle area, as well as the entire soft-tissue layer over the lower part of the shin. This ensures that the internal fixation is fully covered when the incision is closed. The skin incision is conveniently distant from the hardware. The tibia’s lateral column and syndesmosis can be directly observed and realigned. The superficial peroneal nerve can be dissected with minimal invasiveness and kept within the subcutaneous layer. The incision can be expanded in both the proximal and distal directions, allowing for earlier surgical intervention in certain cases of pilon fractures. While the single-incision strategy may seem better for preserving soft tissue, it is important to carefully assess the potential danger of nerve injury, particularly during the first phase of the learning process. However, the single-incision method can be a dependable alternative for achieving improved preservation of soft tissue in fractures of the distal tibia and fibula.
The internal fixation of comminuted fractures of the distal tibia and fibula can easily be achieved using a single-incision technique. This can minimize soft-tissue damage and prevent wound-related complications in this area due to precarious blood supply and lesser soft-tissue coverage in the distal part of the tibia.
References
- 1.Rubio-Yanchuck M, Rubio-Suarez JC, Rodriguez-Merchan EC. Factors that Influence Soft-tissue Injury in Fractures of the Distal Tibia. Arch Bone Jt Surg. 2021 Mar;9(2):152-157. doi: 10.22038/abjs.2020.41667.2126. PMID: 34026931; PMCID: PMC8121041. [Google Scholar | PubMed | CrossRef]
- 2.Kwan YH, Decruz J, Premchand AX, Khan SA. Complex distal tibia fractures treated with multi-planar external fixation - a single center experience. Int J Burns Trauma 2022;12:98-105. [Google Scholar | PubMed]
- 3.Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, et al. Distal tibia fractures: Management and complications of 101 cases. Int Orthop 2010;34:583-8. [Google Scholar | PubMed]
- 4.Lee JY, Lee HJ, Yang SH, Ryu JH, Kim HT, Lee BH, Kim SH, Kim HS, Lee YK. Treatment of Soft Tissue Defects after Minimally Invasive Plate Osteosynthesis in Fractures of the Distal Tibia: Clinical Results after Reverse Sural Artery Flap. Medicina (Kaunas). 2023 Sep 30;59(10):1751. doi: 10.3390/medicina59101751. PMID: 37893469; PMCID: PMC10608781. [Google Scholar | PubMed | CrossRef]
- 5.Song X, Huang X, Yakufu M, Yan B, Feng C. Minimally invasive plate osteosynthesis or conventional intramedullary nailing for distal tibial fractures: A cohort study protocol. Medicine (Baltimore) 2020;99:e21779. [Google Scholar | PubMed]
- 6.Shantharam SS, Naeni F, Wilson EP. Single incision technique for internal fixation of distal tibia and fibula fractures. Orthopedics 2000;23:429-31. [Google Scholar | PubMed]
- 7.An L, Zhang J, Ma W, Zhu L, He X, Ying J, et al. Clinical comparison of single-incision and dual-incision approaches for the treatment of distal tibial and fibular fractures: A randomized controlled trial. J Orthop Surg (Hong Kong) 2020;28:2309499020930305. [Google Scholar | PubMed]
- 8.Yu B, Huang G, George JT, Li W, Pan S, Zhou H. Single-incision technique for the internal fixation of distal fractures of the tibia and fibula: A combined anatomic and clinical study. Arch Orthop Trauma Surg 2013;133:1631-7. [Google Scholar | PubMed]
- 9.Mosheiff R, Safran O, Segal D, Liebergall M. The unreamed tibial nail in the treatment of distal metaphyseal fractures. Injury 1999;30:83-90. [Google Scholar | PubMed]
- 10.Megas P, Zouboulis P, Papadopoulas AX, Karageorgos A, Lambiris E. Distal tibial fractures and non-unions treated with shortened intramedullary nail. Int Orthop. 2003;27:348-51. [Google Scholar | PubMed]
- 11.Ozsoy MH, Tuccar E, Demiryurek D, Bayramoglu A, Hayran M, Cavusoglu AT, et al. Minimally invasive plating of the distal tibia: Do we really sacrifice saphenous vein and nerve? A cadaver study. J Orthop Trauma 2009;23:132-8. [Google Scholar | PubMed]
- 12.Mirza A, Moriarty AM, Probe RA, Ellis TJ. Percutaneous plating of the distal tibia and fibula: Risk of injury to the saphenous and superficial peroneal nerves. J Orthop Trauma 2010;24:495-8. [Google Scholar | PubMed]
- 13.Pugh KJ, Wolinsky PR, McAndrew MP, Johnson KD. Tibial pilon fractures: A comparison of treatment methods. J Trauma 1999;47:937-41. [Google Scholar | PubMed]
- 14.Jain D, Selhi HS, Yamin M, Mahindra P. Soft tissue complications in distal tibial fractures managed with medial locking plates: A myth or reality? J Clin Orthop Trauma 2017;8:S90-5. [Google Scholar | PubMed]
- 15.Höiness P, Engebretsen L, Strömsöe K. The influence of perioperative soft tissue complications on the clinical outcome in surgically treated ankle fractures. Foot Ankle Int 2001;22:642-8. [Google Scholar | PubMed]
- 16.Vallier HA. Current evidence: Plate versus intramedullary nail for fixation of distal tibia fractures in 2016. J Orthop Trauma 2016;30:S2-6. [Google Scholar | PubMed]
- 17.Mair O, Pflüger P, Hoffeld K, Braun KF, Kirchhoff C, Biberthaler P, et al. Management of pilon fractures-current concepts. Front Surg 2021;8:764232. [Google Scholar | PubMed]
- 18.Lin ZQ, Zhang HZ, Luo GG, Yao JC, Xie HF, Zhang X, et al. Comparison of 3 treatment methods for distal tibial fractures: A network meta-analysis. Med Sci Monit 2019;25:7480-7. [Google Scholar | PubMed]
- 19.Hu L, Xiong Y, Mi B, Panayi AC, Zhou W, Liu Y, et al. Comparison of intramedullary nailing and plate fixation in distal tibial fractures with metaphyseal damage: A meta-analysis of randomized controlled trials. J Orthop Surg Res 2019;14:30. [Google Scholar | PubMed]
- 20.Ma H, Zhao J, Yu B, Ye B. A gross anatomic study of distal tibia and fibula for single-incision approach. J Orthop Surg Res 2014;9:28. [Google Scholar | PubMed]
- 21.Femino JE, Vaseenon T. The direct lateral approach to the distal tibia and fibula: A single incision technique for distal tibial and pilon fractures. Iowa Orthop J 2009;29:143-8. [Google Scholar | PubMed]