The longitudinal management of pediatric femoral deformities requires an astute understanding of growth dynamics, pathology, and the biomechanical implications of surgical interventions. This case highlights the complexity of treating a child with a femoral neck fracture and concurrent cystic lesion, complicated by subsequent deformities such as coxa vara and bowing of the femur. The necessity for multiple, adaptive surgical interventions over the course of the child’s development underscore the importance of a personalized treatment plan that evolves with the patient’s growth
Dr. Asad Khan, Department of Orthopaedic Surgery, J. N. Medical College, Faculty of Medicine, A.M.U., Aligarh, Uttar Pradesh, India. E-mail: khanasad53@gmail.com
Introduction: Pediatric femoral deformities present unique challenges in orthopedics, requiring careful management to accommodate ongoing growth and development in young patients. This case report illustrates the longitudinal treatment of a child who experienced multiple complications following an initial femoral neck fracture in a cystic lesion, highlighting the complexity of managing such conditions over time.
Case Report: A 4-year-old child presented in 2016 with a femoral neck fracture and a cystic lesion in the proximal femur, initially managed with valgus osteotomy and dynamic compression plate fixation. Two years later, the patient exhibited a malunited fracture leading to coxa vara, which was managed by implant removal. In 2021, the child developed a bowing deformity which was corrected operatively with another osteotomy and TENS wire insertion. The most recent intervention in 2022 involved a valgus osteotomy and fixation with a dynamic hip screw to address persistent coxa vara, resulting in a successful union.
Conclusion: This case emphasizes the need for ongoing, adaptive management strategies in pediatric orthopedics, particularly for patients with complex femoral deformities. Each surgical intervention was tailored to the child’s evolving anatomical needs, with close follow-up to ensure optimal outcomes as the patient grew. The multidisciplinary approach and continuous reassessment are critical in achieving favorable long-term results in similar pediatric cases.
Keywords: Pediatric orthopedics, femoral deformities, surgical management, longitudinal case study, dynamic hip screw, valgus osteotomy, coxa vara.
Pediatric femoral deformities and pathologies, such as bone cysts and fractures, present significant challenges due to the dynamic nature of growing bones and the potential for long-term complications. The proximal femur, a common site for such conditions, is particularly susceptible to deformities, such as coxa vara and complications including avascular necrosis (AVN), largely due to its critical role in weight-bearing and mobility. Managing these conditions effectively requires an understanding of the unique biomechanics of the pediatric hip and the implications of growth on treatment outcomes. This case report details the progressive and adaptive surgical management of a child initially presenting with a femoral neck fracture and concurrent cystic lesion, complicated by subsequent deformities such as coxa vara and bowing of the femur. Through a series of carefully timed and executed interventions over a 6-year period, this report highlights the complexities of treating evolving orthopedic conditions in pediatric patients, underscoring the importance of a personalized approach that evolves with the patient’s growth.
A 4-year-old child presented 8 years ago with a femoral neck fracture and a cystic lesion in the proximal femur (Fig. 1, 2). Initial management involved a valgus osteotomy and fixation using a dynamic compression plate (Fig. 3). Despite this intervention, complications ensued over the following years, necessitating further surgical treatments.


6 years back, at the age of 6, the patient returned with a malunited femoral neck fracture resulting in a coxa vara deformity, along with the persistence of the cystic lesion. During this visit, the initial implant was removed, and a biopsy was sent from the lesion. The patient was closely monitored for progression or resolution of the condition (Fig. 4).
By the age of 9, the patient developed a bowing deformity of the femur (Fig. 5). Biopsy showed fibrous tissue with irregular, randomly oriented bony trabeculae suggestive of Fibrous dysplasia. This was addressed with an osteotomy at two points and the insertion of a titanium elastic nailing system (TENS) (Fig. 6). The intervention successfully corrected the deformity and the femur healed properly (Fig. 7).

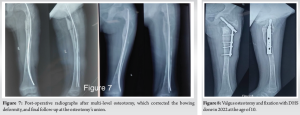
In the latest follow-up 2 years back, the child, now 10 years old, required further surgical management for ongoing coxa vara. A valgus osteotomy was again performed, this time secured with a dynamic hip screw (DHS) (Fig. 8). Subsequent follow-ups confirmed the successful union of the osteotomy site (Fig. 9).

This case illustrates the complex and dynamic nature of managing pediatric femoral deformities, especially when compounded by pathological lesions. Each surgical intervention was critically timed and executed based on the evolving needs of the growing child, demonstrating the necessity for a flexible, long-term therapeutic strategy in pediatric orthopedics.
The case of a 4-year-old child presenting with a fractured neck of the femur and a cystic lesion in the proximal femur 8 years back, managed initially with valgus osteotomy and dynamic compression plate fixation, highlights the complexities and challenges in treating pediatric femoral neck fractures, especially when compounded by cystic lesions. The initial management approach aligns with the literature, which suggests that valgus osteotomy can effectively convert shear forces at the fracture site into compressive forces, promoting bone union and addressing coxa vara deformities [1]. However, the recurrence of issues 6 years back, with the patient presenting with a malunited neck of the femur in coxa vara and a persistent cystic lesion, necessitated implant removal and further monitoring. This recurrence underscores the difficulty in achieving long-term stability and the potential for complications such as non-union and deformity recurrence, which are well-documented in pediatric femoral neck fractures [2,3]. At the age of 9, the patient developed a bowing deformity of the femur, which was managed operatively with osteotomy and TENS wire insertion. This approach is consistent with the management of deformities in conditions, such as osteogenesis imperfecta and fibrous dysplasia, where corrective osteotomy and intramedullary nailing are employed to address bone fragility and deformities [4]. The successful correction and healing of the bowing deformity indicate the effectiveness of this surgical intervention in restoring proper alignment and function. The final surgical intervention 2 years ago, involving valgus osteotomy and fixation with a DHS for the coxa vara deformity, resulted in a successful union, as observed in the follow-up. This outcome is supported by studies that emphasize the importance of achieving anatomic reduction and stable fixation to prevent complications such as AVN and non-union [1,2]. The use of DHS in this context is particularly noteworthy, as it provides a fixed-angle construct that can help maintain the corrected alignment and support healing [5]. Throughout the patient’s treatment journey, the presence of a cystic lesion in the form of fibrous dysplasia in the proximal femur posed additional challenges. Cystic lesions, such as simple bone cysts or aneurysmal bone cysts, are known to increase fracture risk and complicate treatment due to their expansile and locally aggressive nature [5-7]. The management of these lesions often involves curettage, bone grafting, and internal fixation to achieve bony union and prevent recurrence [8-10]. The patient’s case underscores the need for a multidisciplinary approach, combining orthopedic surgical techniques with careful monitoring and follow-up to address both the fracture and the underlying cystic pathology effectively. This case illustrates the multifaceted challenges in managing pediatric femoral neck fractures with concurrent cystic lesions. The iterative surgical interventions, including valgus osteotomy, dynamic compression plate fixation, TENS wire insertion, and DHS fixation, highlight the necessity for tailored treatment strategies to address deformities, ensure bone union, and manage underlying cystic conditions. The successful outcomes achieved through these interventions underscore the importance of a comprehensive and adaptive approach in pediatric orthopedic care [1-10].
Limitation of Study
This case report, while providing valuable insights into the complex management of pediatric femoral deformities, is subject to several limitations inherent in the nature of case studies:
- Single case limitation: As the findings are based on a single patient, the generalizability of the results to the broader pediatric population with similar conditions is limited. Different patients may respond differently to similar treatments due to variations in individual anatomy, growth rates, and underlying health conditions.
- Lack of control group: The absence of a control group makes it challenging to directly attribute the success of the surgical interventions solely to the techniques used, as other confounding factors could influence outcomes.
- Subjectivity in clinical decision-making: The decision-making process in choosing specific surgical interventions and their timing might carry inherent biases based on the surgeon’s preference and experience, which might not reflect a standardized approach that could be universally applied.
- Follow-up duration: Although the follow-up period, in this case, was sufficient to observe initial healing and response to surgeries, longer-term follow-up would be necessary to fully understand the implications of these interventions on the patient’s musculoskeletal development into adolescence and adulthood.
- Detailed documentation: The case report relies on the accuracy and detail of clinical records. Any gaps or inconsistencies in documentation can lead to incomplete understanding or misinterpretation of the clinical course and outcomes.
- Variability in technique and materials: The techniques and materials used (e.g., type of osteotomy, fixation devices) are subject to variations in availability and technological advancement over time, which might influence the reproducibility of the results.
Recognizing these limitations is crucial for interpreting the findings of this case report and for designing future studies that might address these gaps, potentially through multi-case series, comparative studies, or longitudinal research involving larger patient populations.
The management of pediatric femoral deformities, particularly when complicated by pathological lesions such as cysts, demands a comprehensive, adaptive approach that accommodates the ongoing growth and developmental changes of the child. This case report illustrates the complex, multi-staged surgical interventions required over a 6-year period for a child initially presenting with a femoral neck fracture and cystic lesion. The evolution from initial injury through various complications, including malunion, coxa vara, and bowing deformity, highlights the need for a proactive and responsive treatment strategy in pediatric orthopedics. The outcomes observed in this case emphasize the importance of a multidisciplinary team and a long-term commitment to follow-up, which are critical in managing such dynamic conditions effectively. Each intervention was strategically planned to address the specific deformity at an appropriate time in the child’s growth, demonstrating the necessity of individualizing treatment to the patient’s evolving needs. Ultimately, this case underscores the challenges and complexities inherent in pediatric orthopedic management but also illustrates the potential for successful outcomes through diligent, tailored interventions. It reinforces the importance of ongoing research, innovation, and collaboration in the field to continually improve the management strategies for pediatric patients with complex orthopedic conditions.
The longitudinal management of pediatric femoral deformities requires an astute understanding of growth dynamics, pathology, and the biomechanical implications of surgical interventions. This case highlights the complexity of treating a child with a femoral neck fracture and concurrent cystic lesion, complicated by subsequent deformities such as coxa vara and bowing of the femur. The necessity for multiple, adaptive surgical interventions over the course of the child’s development underscore the importance of a personalized treatment plan that evolves with the patient’s growth. Effective management demands a multidisciplinary approach involving pediatric orthopedic surgeons, radiologists, and rehabilitation specialists to ensure comprehensive care. Regular follow-ups are essential to monitor healing, assess functional outcomes, and promptly address any complications or new deformities that may arise as the child grows. This case serves as a reminder of the challenges faced in pediatric orthopedics and the critical role of tailored, proactive surgical and medical strategies in achieving favorable outcomes.
References
- 1.Sarkar A, Sahni S, Sen B. Valgus osteotomy for non-union fracture neck of femur in a child: A case report. SAS J Surg 2023;9:122-4. [Google Scholar | PubMed]
- 2.Haider S, Harris TJ, Turner AC, Podeszwa DA, Hartman CA, Morris WZ. Treatment of delbet II/III pediatric femoral neck fractures with proximal femoral locking plate versus cannulated screws. J Pediatr Orthop 2024;44:213-20. [Google Scholar | PubMed]
- 3.Ansul R, Rajendra A, Birendra B, Chand Y, Prakash G, Banskota AK, et al. Functional and radiological outcomes of surgically treated Coxa-vara in children. J Pediatr Orthop 2024;44:e680-5. [Google Scholar | PubMed]
- 4.Elbaseet HM, Ibrahim AH, Oyoun NA, Abdelzaher MA, Khaled M. Management of combined fracture neck of femur and femoral deformity in osteogenesis imperfecta patient: A case report. Strategies Trauma Limb Reconstr 2024;19:56-9. [Google Scholar | PubMed]
- 5.Sonkusale A, Gandhi P, Jadhav D, Keswani P. An uncommon case report: Pathologic fracture in a proximal femur aneurysmal bone cyst in a child. J Orthop Case Rep 2023;13:51-4. [Google Scholar | PubMed]
- 6.Van Geloven TP, Van der Heijden L, Laitinen MK, Campanacci DA, Döring K, Dammerer D. As simple as it sounds? The treatment of simple bone cysts in the proximal femur in children and adolescents: Retrospective multicenter EPOS study of 74 patients. J Child Orthop 2024;18:85-95. [Google Scholar | PubMed]
- 7.Lohiya D, Dudhekar U, Vasavada S, Bajaj S. A case report: Aneurysmal bone cyst of proximal femur with subtrochanteric femur fracture in a child. J Pharm Negat Results 2022;13:251-5. [Google Scholar | PubMed]
- 8.Adaş M, Çakar M, Demirkale İ. Long-term outcomes of decompression and grafting in acute pathological proximal femur fractures in children with unicameral bone cysts: A retrospective study utilizing a 120° Fixed-angle low-contact locking pediatric hip plate. Med Sci Monit 2023;29:e943031. [Google Scholar | PubMed]
- 9.Michalik R, Hildebrand F, Delbrück H. Stailisation of pathologic proximal femoral fracture near the growth plate with use of a blocking plate and transphyseal screws. Children (Basel) 2022;9:1932. [Google Scholar | PubMed]
- 10.Jagiasi J, Rai AK, Sharan S, Bandebuche A. Management of aneurysmal bone cyst with pathological femur fracture: A rare case report and review of literature. J Orthop Rep 2022;2:100119. [Google Scholar | PubMed]