In kyphotic patients with CLL, it is crucial to consider the elevated risk of infection, such as Mycobacterium avium, when undergoing ALIF surgery to minimize additional complications.
Dr. Vadim Dolgov, Washington State University, Elson S. Floyd College of Medicine, 412 E Spokane Falls Blvd Spokane, Washington, United States. E-mail: vadim.dolgov@wsu.edu
Introduction: Kyphosis is characterized by excessive forward curvature of the spine often causing back pain and stiffness, and occasionally, neurological deficit. Surgical management of kyphosis can entail an anterior lumbar interbody fusion (ALIF) in addition to a posterior spinal fusion with or without a laminectomy. Chronic lymphocytic leukemia (CLL) is a slow-growing cancer that affects the bone marrow. If ALIF is considered as a treatment option for kyphosis in a patient with CLL, attention needs to be taken to minimize complications.
Case Report: A 70-year-old male with a history of kyphosis and CLL presented with refractory lower back pain attributed to his kyphosis. The patient required multiple procedures to correct his kyphosis including an ALIF between L3 and S1. During the ALIF, significant scar tissue and phlegmon were noted at the surgical site, and disc cultures revealed Mycobacterium avium. The accumulation of phlegmon and scar tissue required significant manipulation of the vessels to perform the procedure. Before closure of the anterior incision, the patient presented with absent pulses of the left leg. A thrombosis in the left iliac artery was noted and treated with stent placement during the surgery.
Discussion: CLL leads to an immune compromised state which may lead to undiagnosed infections, specifically M. avium in our patient. Imaging showed the infection likely played a role in the disc degeneration of the lumbar spine, exacerbating the formation of the phlegmon and scar tissue. This required extensive manipulation of the vessels that resulted in the formation of thrombosis of the left iliac artery.
Conclusion: Care must be taken during ALIF procedures on patients with CLL during manipulation of the vessels. If kyphosis is rapidly worsening in a patient with CLL, infection of the vertebra should be ruled out.
Keywords: Lumbar spondylosis, anterior lumbar interbody fusion, chronic lymphocytic leukemia, kyphosis, chronic lymphocytic leukemia, Mycobacterium avium, anterior lumbar interbody fusion.
Kyphosis is characterized by excessive forward curvature of the spine often causing back pain, usually associated with stiffness [1]. Surgical management can include anterior lumbar interbody fusion (ALIF), lateral lumbar interbody fusion, Smith–Petersen osteotomies, Ponte osteotomies, 3 column osteotomies, and other maneuvers to restore lordosis [2]. An ALIF is an approach to spinal fusion in which the orthopedic surgeon accesses the ant vertebra from the anterior of the patient’s body. This is normally performed through a lower left abdominal incision to not cause damage to thinner blood vessels, such as the inferior vena cava, during obtaining surgery site access [3]. A direct benefit of performing surgery anteriorly is the ability to insert a larger cage in between the vertebra for greater support and distance between vertebra for the treatment of kyphosis. During the procedure, bone graft is obtained from the pelvis for the purpose of disc fusion [4]. Chronic lymphocytic leukemia (CLL) is a slow-growing cancer that affects the blood and bone marrow. It is characterized by the overproduction and accumulation of mature, but abnormal, white blood cells (WBCs) called lymphoblasts in the blood, bone marrow, and lymphatic tissue [5]. Symptoms may include fatigue, weight loss, and swollen lymph nodes [6]. CLL is usually a slow-growing cancer with a good prognosis [7]. Treatment of CLL places a patient in an immunosuppressed state. The presence of CLL in this patient presented unique challenges pertaining to the management of a spine infection in combination with kyphosis, chronic back pain, and multilevel spondylosis with varying levels of central canal and intraforaminal stenosis with radiculopathy and central stenosis syndrome. The purpose of this presentation is to present a patient with lumbar spondylosis, lumbar kyphosis, radiculopathy, severe central canal syndrome, and inability to walk in the setting of CLL and what was ultimately identified as Mycobacterium avium in the disc space of L4-5.
The patient was informed that the data concerning their case would be submitted for publication and gave permission for its use.
A 70-year-old male patient with a history of COPD, 40 pack/year smoking history, and CLL presented to clinic for evaluation of severe refractory lower back pain that radiated into his right lower extremity. He had a history of working as a heavy laborer. Nine months before the evaluation, the patient sustained a ground level fall resulting in a lower back injury. He developed persistent lower back pain, radiating into his lower extremities with neurogenic claudication. He underwent two epidural steroid injections and multiple sessions of physical therapy with only temporary relief of his symptoms. The patient complained of decreased sensation associated with the legs distal to the calves, particularly at the lateral aspect on the dorsal aspect of the feet. Physical examination showed tenderness of the lower lumbar paraspinous musculature and the midline. There was limited range of motion of the lumbar spine, the patient visibly had some kyphosis associated with the spine. There was 4/5 strength in the right knee extension and left knee extension. The ankle dorsiflexion strength was 4/5 bilaterally. There was 4/5 dorsiflexion strength in the extensor hallucis longus bilaterally. L5 Motor Strength on the Right: ankle dorsiflexion tibialis anterior 4/5. There was decreased sensation in the bilateral L4 and L5 distribution in the legs. The patient’s gait was impeded to the extent that he was dependent upon a walker only for short distances. By the time he presented for the definitive posterior surgery, he was dependent on a wheelchair to transport. Laboratories were consistent with CLL showing an elevated WBCs (14.6 K/µL), decreased neutrophils percentage (38.8%), increased lymphocyte percentage (56.2%), increased lymphocyte count (8.22K/µL), and decreased prothrombin time (10.4 s).
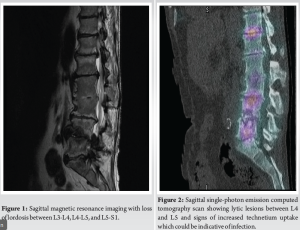
Radiographs identify that there was diminished disc base throughout the lumbar spine with loss of lordosis (Figs. 1 and 2). There was a previous synostosis associated with L2-3. There was no abscess formation.
Plan
We proposed that the patient have at least some restoration of lordosis in preparation for a very definitive posterior procedure in which we anticipated that the patient would require facetectomies and a posterior spinal fusion to adequately decompress the nerve roots laterally at the neuroforamina while also decompressing the central canal. To achieve these objectives in a spine that had this much kyphosis, it was felt that an ALIF would allow better restoration of the lordosis while also maximally allowing an optimal fusion [8]. Hence, it was proposed that the patient have an ALIF of L3-S1 followed by a second stage posterior spinal fusion of the same with assertive facetectomies and laminectomies for maximal decompression under the circumstances in which the patient was losing function of the L4 and L5 radicular distribution and the motor and sensory fibers.
Procedure and complications
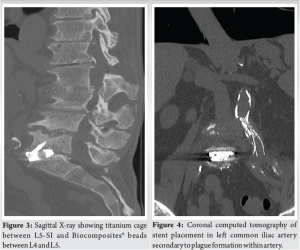
The surgeons embarked upon an intended L3-S1 ALIF. However, substantial scar tissue was identified at L3-4 and L4-5. The limited exposure of L4-5 identified that there was not only scar tissue, but phlegmon. The tissue was sent off for pathological analysis with culture and sensitivities. During this dissection, the limited access to L4-5 called for placement of antibiotic beads for the suspected infection. Hence, antibiotic beads from Biocomposites® Stimulan laden with vancomycin were placed into the disc base of L4-5. There was no such phlegmon associated with L3-L4, but there certainly was scar tissue at L3-4, and that prohibited the surgeons from adequate access to the disc space. Therefore, a fusion procedure was not performed anteriorly for L3-4. With the interest of restoring lordosis to the spine, an ALIF was performed at L5-S1 utilizing the Globus Titanium Hedron case packed with 10 cc of Solum IV which was mixed with bone marrow aspiration from the left anterior iliac crest processed by Celling biosciences. The locking wedges of this plate were utilized for maximal stability. Before closure, a drop off of the pulses in the left leg were observed and the patient’s left leg had become cold. A thrombosis had formed in the left iliac artery during the operative intervention. This was attended to by a vascular surgeon with a left common iliac angioplasty balloon (10 mm × 4 cm) and stenting (10 mm × 6 cm) with uncovered stent through a left inguinal approach. There was restoration of pulses, and the need for fasciotomies in the leg did not arise.
The radiographic results of the procedure are noted in Figs. 3 and 4, including the stent placement on the left iliac vessels and the ALIF of L5-S1 with antibiotic bead placement into the disc space of L4-5 (Fig. 3 and 4).
Follow-up examination identified that the patient had M. avium growing from the L4-5 disc space. Infectious disease was consulted. The patient’s antibiotic regimen consisted of oral rifampin 300 mg capsule q Daily oral ethambutol 400 mg tablet q Daily and oral azithromycin 500 MG tablet q Daily.
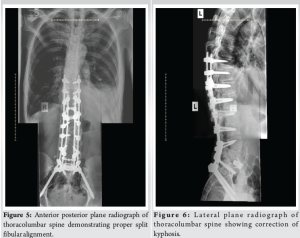
The patient was placed on a 3-month regimen of Plavix as an antiplatelet agent. With the clearances from vascular surgery, the patient underwent a lateral lumbar interbody fusion of L1-2 on account of the lack of restoration of lordosis at L4-5 and L3-4. In addition, the patient had kyphosis associated with L2-3 where there was a synostosis already.
In the second of 3 stages of this total spine management, the patient had the lateral lumbar interbody fusion utilizing the Globus Rise-L expandable cage, packed with Globus Kinex treated with bone marrow aspiration from the left iliac crest. In the final stage of the surgery one month later, the patient had a posterior fusion performed from T10 to the pelvis with laminectomies of L1-L2, L3-L4, L4-5, and L5-S1. A Smith–Peterson osteotomy was performed at T12-L1. Neither stage II nor stage III had complications (Fig. 5). The patient has been seen 1 year follow-up, and the radiographs identify that the patient has ongoing restoration of lordosis in proper posture associated with the thoracic and lumbar spine (Fig. 6). The patient’s pain has diminished in the back to the extent that he does not really perceive pain in the back. His pain issues are related to other issues, and his energy levels are low on account of unexplained weight loss. The patient has demonstrated fusion associated with the intended levels of fusion of T10 through the pelvis. The patient has plain radiographs and computed tomography scans as noted below identifying this. The patient perceives that he has had slow but progressive improvement in his neurological status in his lower extremities. He has progressed his gait from wheelchair bound status to ambulation with a walker, including around the house. However, the patient has developed chest adenopathy and weight loss that has not been ascertained. This in the midst of oncological work-up at this time.
This case report identifies a unique circumstance of a 70-year-old man with CLL who was identified as having M. avium at L4-5 in the disc space, necessitating adaptation of the surgical plan when conducting an ALIF of L4-5 and L5-S1. In combination with a subsequent second stage lateral lumbar interbody fusion of L1-2 and a third stage posterior spinal fusion of T10 to the pelvis with assertive laminectomies and facetectomies, acceptable restoration of the patient’s lumbar lordosis and overall spinal alignment was achieved in conjunction with management of the infectious disease problem of L4-L5. Follow-up of the patient identifies improving strength and sensory function in the bilateral lower extremities in addition to reduction of back pain to the extent that the patient is walking with a walker in a stable fashion. CLL leads to an immune compromised state which may lead to undiagnosed infections, specifically M. avium in our patient [9]. Imaging showed the infection likely played a role in the disc degeneration of the lumbar spine at L4-L5. This required extensive manipulation of the vessels that resulted in the formation of thrombosis of the left iliac artery. Retrograde stent placement was used to reopen the left common iliac artery. The infection of L4-5 has been successfully treated with a combination of surgical debridement, segmental stabilization, oral rifampin, azithromycin, and ethambutol. The utilization of a titanium cage at L5-S1 was performed on account of the unique property of titanium of resisting the development of glycocalyx formation, with the intent of mitigating the risk of the development of infection at L5-S1.
Care must be taken during ALIF procedures, especially during manipulation of the vessels, while maintaining vigilance for the known risk of vascular compromise. Preoperative “clearance” was obtained for this case before the initiation of surgery from oncology. When an immunosuppressed patient has rapidly progressing kyphosis, kyphosis secondary to infection should be ruled out. Further weight should be placed on imaging over laboratory values when attempting to rule out infection in patients with CLL. If infection is discovered during surgery in a patient with CLL, multiple classes of antibiotics should be used as a first-line treatment before culture results.
In immune compromised patients, discitis must be considered in newly presenting back pain with kyphosis.
References
- 1.Yaman O, Dalbayrak S. Kyphosis and review of the literature. Turk Neurosurg 2014;24:455-65. [Google Scholar]
- 2.Pizzutillo PD. Nonsurgical treatment of kyphosis. Instr Course Lect 2004;53:485-91. [Google Scholar]
- 3.Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: A literature review. Ann Transl Med 2018;6:104. [Google Scholar]
- 4.Inamasu J, Guiot BH. Vascular injury and complication in neurosurgical spine surgery. Acta Neurochirur 2006;148:375-87. [Google Scholar]
- 5.Forconi F, Moss P. Perturbation of the normal immune system in patients with CLL. Blood 2015;126:573-81. [Google Scholar]
- 6.Diaco ND, Strohdach B, Falkowski AL, Hainc N, Brunner P, Rutishauser J, et al. Psoas abscess due to Mycobacterium avium in A patient with chronic lymphocytic leukemia-case report and review. J Clin Med 2019;8:216. [Google Scholar]
- 7.Ivanescu AM, Oprea M, Momanu R, Coles E, Colita A, Lupu AR. Prognosis factors in chronic lymphocytic leukemia. J Med Life 2012;5:48-53. [Google Scholar]
- 8.Cho WJ, Kang CN, Park YS, Kim HJ, Cho JL. Surgical correction of fixed kyphosis. Asian Spine J 2007;1:12-8. [Google Scholar]
- 9.Nosari A. Infectious complications in chronic lymphocytic leukemia. Mediterr J Hematol Infect Dis 2012;4:e2012070. [Google Scholar]
- 10.Mobbs RJ, Phan K, Daly D, Rao PJ, Lennox A. Approach-related complications of anterior lumbar interbody fusion: Results of a combined spine and vascular surgical team. Global Spine J 2016;6:147-54. [Google Scholar]