Individuals who present with complaints of knee pain and restricted deep flexion mucoid degeneration of the ACL should be given careful consideration. These individuals are often in their mid-40s
Dr. Syed Kareemulla, Department of Orthopaedics Traumatology, Amulya Nursing Home, Narasaraopet, Andhra Pradesh, India. E-mail: sdkarim1926@gmail.com
Introduction: Mucoid degeneration (MD) of the anterior cruciate ligament (ACL) is a rare entity affecting the middle-aged people with equal gender predisposition. The enigmatic pathological etiology of MD of ACL has been the subject of numerous ideas, including synovial, traumatic, degenerative, ectopic, changed joint mechanics, etc. correlating magnetic resonance imaging (MRI) with clinical diagnosis helps in concluding the diagnosis. Arthroscopic debulking of the ACL helps in relieving the pain.
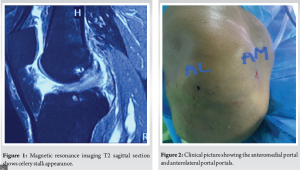
Case Report: We describe here a woman in her 40s who has been experiencing right knee pain for the past 2 years. Although there are no additional clinical symptoms visible upon examination, there is pain with deep knee flexion. MRI’s knee has been taken, and celery stalk appearance has been noticed, as described by Akin. The patient was treated with arthroscopic debulking using conventional arthroscopic portals, and the pain was relieved.
Conclusion: The diagnosis of MD is assisted by clinical examination and correlating the clinical findings with MRI, as it is typically overlooked. The pain is reduced with arthroscopic debulking.
Keywords: Mucoid degeneration anterior cruciate ligament, celery stalk appearance, arthroscopic debulking.
The first description of anterior cruciate ligament (ACL) mucinous degeneration was made in 1999 [1]. The prevalence of mucinous degeneration ranged from 0.7% to 5.3% [2]. All of them are not symptomatic. ACL degeneration is a disorder with a wide scope. Regarding the mucin-induced degeneration of the ACL, several theories have been put forth. Explained it may be due to traumatic or degenerative or synovial [3,4]. It is either their primary or secondary condition (meniscal cysts, osteoarthritis) [5-7]. Middle-aged people are typically affected. This common condition is frequently misdiagnosed. The patient should be thoroughly examined, a diagnosis made, and an intervention carried out while bearing in mind the current situation. ACL debulking is the procedure of choice. Sometimes, notchplasty is necessary in addition to careful ACL debulking.
A 40-year-old female came with a complaint of pain over the posterior aspect of her right knee for 2 years with no history of trauma. Clinical testing was performed prior to surgery with no signs of instability. Pain with deep flexion is noticed, no terminal restriction of extension and no signs of instability are present. To further evaluate, the patient was instructed for X-ray scanogram and magnetic resonance imaging (MRI) of the knee. X-ray scanogram reveals no deviation of mechanical axis, and MRI knee was taken and in MRI the classical celery stalk appearance was noticed in the t2 sagittal section of knee (Fig. 1). The clinical and radiological findings are correlated, and the patient planned arthroscopic debulking.
Surgical technique evaluation
Portals used
- Portal A- Standard arthroscopic anterolateral portal, which is 1 cm inferior and lateral to the inferior pole of the patella
- Portal B- Standard anteromedial portal which is determined using a spinal needle (Fig. 2).
Surgical technique
Under spinal anesthesia, the patient is positioned supine, and a standard arthroscopic anterolateral portal is made with 11 blades. Diagnostic arthroscopy is done, which reveals a bulky ACL impinging in the intercondylar notch (Fig. 3), with no lesions in cartilage and menisci.

With the assistance of a spinal needle, an antero medial portal is placed, and a shaver is passed. The mucinous part of the ACL is removed with the help of a meniscus punch and arthroscopic shaver. No impingement was observed in flexion and extension.
No signs of instability after debulking are noticed (Fig. 4). Wound closure and pressure bandage applied.
Post-operative rehabilitation
Weight-bearing allowed on day 1.
Ankle pumps and gluteal strengthening exercises are started.
Quadriceps strengthening is started and the patient refrained from activities that cause increased joint pressure.
Knee core strengthening exercises have been done.
The patient followed up for a year and the patient is completely free of pain and there is grade 1 laxity on examination, and the patient was okay with it as she is a housewife.
The mucoid degeneration (MD) of ACL is a rare entity affecting the middle-aged people with equal gender predisposition, according to the literature. It is frequently missed in the diagnosis. Various theories are proposed in respect to the etiology of MD of ACL, traumatic, degenerative, synovial, ectopic, and altered biomechanics. Repetitive microtrauma theory was also suggested by lancaster. The clinical presentation of MD is variable with posterior knee pain, pain in deep flexion, terminal extension is restricted, clicks, and audible snaps. MRI is the imaging modality of choice for the diagnosis of MD of ACL, displaying a moderate T1-weighted signal intensity and a high T2-weighted signal intensity. MRI features suggestive of MD of ACL is celery stalk appearance according to akin. MRI helps in differentiating mucoid cyst from MD [8]. The gold standard for diagnosing MD is the histology of the specimen. The arthroscopic findings of MD are the absence of mucous ligamentosum and the absence of synovial lining with impinging in the intercondylar notch with bulky hypertrophied ACL with yellowish mucinous material interposed in between; Whereas the normal ACL is smooth, shiny with a synovial covering over it. To manage the MD, several treatment modalities are proposed. Nonsteroidal Anti-Inflammatory Drugs are given initially for pain management. Certain individuals even recommend injecting hyaluronic acid with 40 mg of triamcinolone followed by physiotherapy, provided that the clinical complaints in these young patients correlate with MRI and rule out other pathologies. However, there is a dearth of published evidence regarding this management. However, in adult patients with MD who also have malalignment and adjacent pathologies such as medial compartment varus and root tears, these conditions should be treated with high tibial osteotomy and root repair in addition to debulking [9,10]. The patient should be preoperatively counseled regarding the need for ACL reconstruction if needed. Precarious debulking of the ACL is crucial after accurately diagnosing the mucinous degeneration of the ACL [11]. After debulking, the impingement should be examined using range of motion, and if any instability exists, an ACL reconstruction plan should be created. Additional notchplasty is required, especially in older age groups and people with a stenotic notch [12]. The debulking should be perfectly done such that there is no impingement between ACL and posterior cruciate ligament, and it should be cleared from the notch completely, and Howells triangle should be created. A satisfactory clinical outcome and an early return to sports with little risk of instability are achieved with the prudent debridement of the mucoid ACL and the mucinous debris preservation of the intact ACL fibers to restore the normal morphology [13]. Certain individuals undergoing intended partial ACL decompression in several published treatments need ACL reconstruction because of instability [14].
Patients in their middle years who visit the OPD complaining of pain over the back of the knee with pain during deep flexion should be evaluated for mucinous degeneration because it is frequently overlooked. Utilizing the gold standard of MRI to correlate clinical results. Pain relief with arthroscopic debulking is beneficial.
Mucoid ACL has few clinical signs, making diagnosis extremely challenging. The clinical manifestations include reduced deep flexion and joint line discomfort. MRI aids in maintaining diagnosis. The gold standard is a biopsy.
References
- 1.Kumar A, Bickerstaff DR, Grimwood JS, Suvarna SK. Mucoid cystic degeneration of the cruciate ligament. J Bone Joint Surg Br 1999;81:304-5. [Google Scholar | PubMed]
- 2.Makino A, PascualGarrido C, Rolón A, Isola M, Muscolo DL. Mucoid degeneration of the anterior cruciate ligament: MRI, clinical, intraoperative, and histological findings. Knee Surg Sports Traumatol Arthrosc 2011;19:408-11. [Google Scholar | PubMed]
- 3.Narvekar A, Gajjar S. Mucoid degeneration of the anterior cruciate ligament. Arthroscopy 2004;20:141-6. [Google Scholar | PubMed]
- 4.Salvati F, Rossi F, Limbucci N, Pistoia ML, Barile A, Masciocchi C. Mucoid metaplastic-degeneration of anterior cruciate ligament. J Sports Med Phys Fitness 2008;48:483-7. [Google Scholar | PubMed]
- 5.Bergin D, Morrison WB, Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: Coexistence and clinical correlation. AJR Am J Roentgenol 2004;182:1283-7. [Google Scholar | PubMed]
- 6.Pandey V, Suman C, Sharma S, Rao SP, Kiran Acharya K, Sambaji C. Mucoid degeneration of the anterior cruciate ligament: Management and outcome. Indian J Orthop 2014;48:197-202. [Google Scholar | PubMed]
- 7.Lancaster TF, Kirby AB, Beall DP, Wolff JD, Wu DH. Mucoid degeneration of the anterior cruciate ligament: A case report. J Okla State Med Assoc 2004;97:326-8. [Google Scholar | PubMed]
- 8.McIntyre J, Moelleken S, Tirman P. Mucoid degeneration of the anterior cruciate ligament mistaken for ligamentous tears. Skeletal Radiol 2001;30:312-5. [Google Scholar | PubMed]
- 9.Lintz F, Pujol N, Boisrenoult P, Bargoin K, Beaufils P, Dejour D. Anterior cruciate ligament mucoid degeneration: A review of the literature and management guidelines. Knee Surg Sports Traumatol Arthrosc 2011;19:1326-33. [Google Scholar | PubMed]
- 10.Dallo I, Chahla J, Mitchell JJ, Pascual-Garrido C, Feagin JA, LaPrade RF. Biologic approaches for the treatment of partial tears of the anterior cruciate ligament: A current concepts review. Orthop J Sports Med 2017;5:2325967116681724. [Google Scholar | PubMed]
- 11.Sweed T, Mussa M, El-Bakoury A, Geutjens G, Metcalfe A. Management of mucoid degeneration of the anterior cruciate ligament: A systematic review. Knee Surg Relat Res 2021;33:26. [Google Scholar | PubMed]
- 12.Lintz F, Pujol N, Dejour D, Boisrenoult P, Beaufils P. Anterior cruciate ligament mucoid degeneration: Selecting the best treatment option. Orthop Traumatol Surg Res 2010;96:400-6. [Google Scholar | PubMed]
- 13.Ventura D, Nuñez JH, Joshi-Jubert N, Castellet E, Minguell J. Outcome of arthroscopic treatment of mucoid degeneration of the anterior cruciate ligament. Clin Orthop Surg 2018;10:307-14. [Google Scholar | PubMed]
- 14.Hotchen AJ, Demetriou C, Edwards D, Melton JT. Mucoid degeneration of the anterior cruciate ligament: Characterization of natural history, femoral notch width index, and patient reported outcome measures. J Knee Surg 2019;32:577-83. [Google Scholar | PubMed]











