The occurrence of tray-taper breakage following primary reverse total shoulder arthroplasty is a rare but noteworthy complication. It is imperative for surgeons to remain vigilant about the possibility of encountering this uncommon issue. This case report not only illustrates infrequent complications of tray-taper breakage but also contributes to a broader understanding of the spectrum of complications associated with reverse total shoulder arthroplasty.
Dr. Chang Hee Baek, Department of Orthopaedic Surgery, Yeosu Baek Hospital, Jeollanam-do, Republic of Korea. E-mail: yeosubaek@gmail.com
Introduction: Reverse total shoulder arthroplasty (RTSA) has become a pivotal intervention for managing rotator cuff arthropathy in the elderly, showing consistent improvements in pain relief and shoulder function. However, the broad spectrum of indications for RTSA is accompanied by a notable incidence of complications, prompting continuous advancements in technology and surgical techniques.
Case Report: This case report presents an uncommon complication rarely discussed in the existing literature – humeral tray-taper breakage after RTSA. The patient, a 68-year-old with a history of rotator cuff repair surgery, underwent RTSA with concurrent subscapularis repair due to rotator cuff arthropathy. Postoperatively, the patient gradually reported weakness in internal rotation (IR), leading to a subsequent secondary pectoralis major (PM) transfer. However, following an incident where the patient experienced acute pain due to a slip, a tray-taper breakage in the implant was revealed. To address the broken implant and the weakness in IR, the patient underwent revision RTSA combined with the PM transfer. With a post-operative rehabilitation program, at 1 year and 6 months postoperatively, the patient demonstrated significant pain relief and improved functional outcomes.
Conclusion: The case report underscores the importance of recognizing and addressing rare complications associated with RTSA, providing insights into the management of humeral tray-taper breakage. Furthermore, combined PM transfer to RTSA could be a solution to weakness in IR. This case report emphasizes the need for careful consideration of potential complications and innovative solutions for optimal patient outcomes.
Level of Evidence IV: Case report.
Keywords: Reverse total shoulder arthroplasty, revision shoulder arthroplasty, complication
Reverse total shoulder arthroplasty (RTSA) has emerged as a compelling option for addressing rotator cuff arthropathy in the elderly population, demonstrating consistent improvements in both pain relief and shoulder function [1]. Over time, the accumulated clinical experience has driven technological advancements in implant design and surgical techniques. The versatility of RTSA has demonstrated promising outcomes across a spectrum of conditions, ranging from massive rotator cuff tears and fractures to arthritis, chronic dislocations, and fracture sequelae [2]. However, the extensive range of indications for RTSA is accompanied by different types of complications, including infection, periprosthetic fracture, instability, and loosening [3]. In this context, we present a unique case report focusing on an uncommon complication rarely discussed in the existing literature: Humeral tray-taper breakage after RTSA [4]. The significance of this case lies not only in its rarity but also in informing the potential complications associated with RTSA.
Case Description
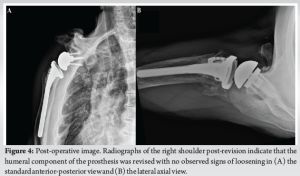
A 68-year-old patient, right-hand dominant, experienced chronic pain and weakness in the right shoulder. Before visiting our hospital, the patient underwent rotator cuff repair surgery at another hospital about a year ago. On examination, a re-tear with atrophy and severe fatty degenerations of the supraspinatus and infraspinatus was identified, leading to RTSA concomitant with subscapularis repair. Postoperatively, the patient initially expressed satisfaction with the clinical results. However, starting at the post-operative 2-year mark, he gradually reported a loss of internal rotational (IR) strength and range of motion. Sonography revealed a re-tear of the repaired subscapularis. Conservative treatment, including strengthening exercises, was administered for 1 year. Despite this, the patient continued to experience reduced IR strength, particularly during activities such as toileting. Functional assessments indicated unsatisfactory scores: A pain Visual Analog Scale (VAS) of 5, a Constant score of 38/100, and an American Shoulder and Elbow Surgeons (ASES) score of 41/100. IR to back reached buttock level and strength measured was 15.4N. Radiographic evaluation showed no signs of implant loosening. (Fig. 1) After discussing with the patient, a secondary pectoralis major (PM) transfer was scheduled, but a few days before the operation, the patient was injured from a slip down in his right shoulder, with a tray-taper breakage seen on radiography and computed tomography scans (Fig. 2a and b). Consequently, a revision RTSA was recommended for the broken implant, combined with the PM transfer to address IR weakness.
Surgical method and post-operative rehabilitation
Under general anesthesia, the patient was placed in the beach chair position. Utilizing the previous incision line, a standard deltopectoral approach was employed, extended inferiorly to expose the insertion of the PM tendon in the humerus. Surrounding tissue around the PM was released, and the PM tendon was detached from the insertion site. After preparing the PM tendon (Fig. 3a), the broken tray-taper part of the RTSA was removed, and the humeral component was extracted using a flexible osteotome. (Fig. 2c) The glenoid component showed stable fixation and was left untouched. Afterward, six holes were created in the greater tuberosity of the humerus to pass the free sutures. These sutures formed loops, and the fracture-cemented humeral stem (Equinoxe; Exactech, Inc, Gainesville, Florida, USA) was passed through the pre-placed loop suture and impacted into the humerus. (Fig. 3b) Each end of the sutures was passed through the lateral edge of the harvested PM tendon, and the other ends were passed through the teres minor tendon. (Fig. 3c) Finally, these sutures were tied together, ensuring a firm attachment of the PM tendon to the humerus. (Fig. 3d) The patient was immobilized for the first 4 weeks and gradually progressed to an active-assisted range of motion exercises, followed by strengthening exercises at 3 months postoperatively.
Post-operative outcome
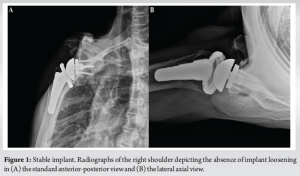
At 1 year and 6 months postoperatively, the patient experienced significant relief from pain, achieving a pain VAS of 1. Functional outcomes were satisfactory, with a Constant score of 75/100 and an ASES score of 77/100. IR increased from the level of the buttock to the L3 level, accompanied by improved strength measuring 29.1N. Radiographic images showed a securely fixed implant without any signs of loosening (Fig. 4).
The utilization of RTSA in the treatment of rotator cuff arthropathy has yielded promising clinical outcomes. However, like any surgical procedure involving prosthesis implantation, it introduces a spectrum of potential complications [1, 3, 5]. Noteworthy complications associated with RTSA include infection, instability, implant loosening, prosthetic fracture, and others, contributing to an overall reported complication rate of highest up to 25% in primary RTSA [6-8] Tray-taper problems, although rarely reported, have been documented in case studies. For instance, et al. [9] reported a case of spontaneous dissociation of a conventional Morse taper in a modular third-generation shoulder hemiarthroplasty. Another study by Kaymakoglu et al. [10] highlighted a case of humeral stem tray failure in RTSA, and McDonald et al. [11] presented a case series depicting humeral tray-taper junction failure. These complications may manifest following strenuous activities such as weight lifting, golfing, or mechanical falls [11]. In addition, they may be associated with the use of different component materials, as suggested by Lewicki et al. [12], who reported a 10-fold lifetime increase in Cobalt chrome component devices compared to Titanium devices based on finite element and fatigue analyses in the tray-taper part of the implant. Despite the diversity in causative factors, patients often present with non-specific symptoms, such as pain and mechanical clicking, emphasizing the need for a comprehensive evaluation of component attachment. In this current case report, we detailed an unusual occurrence of taper-tray breakage in RTSA, resulting from a mechanical fall. Patients experienced abrupt pain, and radiographic evaluation revealed dissociation of the taper-tray component. This case highlights the importance of recognizing and addressing such a problem, even though they may be infrequently reported. Furthermore, it is imperative to acknowledge the functional limitations of RTSA, particularly in terms of IR, which is a crucial aspect affecting patients’ daily activities, such as toileting [13]. In our case, when faced with IR dysfunction and the failure of conservative treatment, we planned a secondary PM transfer before deciding on the revision of RTSA. PM transfer, known for its use in irreparable subscapularis to enhance IR [14], has been acknowledged for its effectiveness in addressing IR dysfunction in both clinical and biomechanical studies [15-17]. The revision procedure involved concomitant PM transfer, resulting in improved post-operative IR strength and range of motion. This underscores the significance of considering alternative interventions to address functional IR deficits associated with RTSA. The choice of implant type in RTSA also warrants discussion. In our case, we opted for a lateralized RTSA implant. While existing studies suggest that lateralized implants may lead to increased IR, [18, 19] the clinical outcomes remain variable and unpredictable [20-23] Kim et al. [24] demonstrated that implant type and lateralization were not independent factors influencing IR. Similarly, Gibian et al. [25] identified higher pre-operative IR and 1-year post-operative forward elevation as independent predictors of sufficient post-operative IR after RTSA. Despite potential advantages, the observed increase in IR strength and range of motion cannot be conclusively attributed solely to the lateralized implant in our case.
The limitation of RTSA longevity necessitates revision surgery, often prompted by various complications, including the rare occurrence of taper-tray breakage. The current case report exemplifies the importance of recognizing and addressing such mechanical complications. Notably, in our case, the revision procedure incorporated a PM transfer to treat the IR dysfunction. This emphasizes the need for vigilance in managing both uncommon mechanical complications and post-operative IR deficits that may arise following primary RTSA.
Humeral tray-taper breakage is a rare but serious complication following reverse total shoulder arthroplasty. In selected patients with residual internal rotation weakness, a combined pectoralis major transfer and revision RTSA can effectively restore functional outcomes.
References
- 1.Mayfield CK, Korber SS, Hwang NM, Bolia IK, Gamradt SC, Weber AE, et al. Volume, indications, and number of surgeons performing reverse total shoulder arthroplasty continue to expand: A nationwide cohort analysis from 2016-2020. JSES Int 2023;7:827-34. [Google Scholar]
- 2.Oh JH, Jeong HJ, Won YS. Implant selection for successful reverse total shoulder arthroplasty. Clin Shoulder Elb 2023;26:93-106. [Google Scholar]
- 3.Galvin JW, Kim R, Ment A, Durso J, Joslin PM, Lemos JL, et al. Outcomes and complications of primary reverse shoulder arthroplasty with minimum of 2 years’ follow-up: A systematic review and meta-analysis. J Shoulder Elbow Surg 2022;31:e534-44. [Google Scholar]
- 4.Liebhauser M, Hohenberger G, Lohberger B, Hauer G, Deluca A, Sadoghi P. Implant breakage after shoulder arthroplasty: A systematic review of data from worldwide arthroplasty registries and clinical trials. BMC Musculoskelet Disord 2023;24:804. [Google Scholar]
- 5.Maier SP 2nd, Prabhat AM, Collins JE, Von Keudell A, Earp B, Zhang D. Outcomes of reverse total shoulder arthroplasty for proximal humerus fracture versus rotator cuff arthropathy. J Am Acad Orthop Surg Glob Res Rev 2023;7:e23.00169. [Google Scholar]
- 6.Dragonas CG, Mamarelis G, Dott C, Waseem S, Bajracharya A, Leivadiotou D. Anatomic total shoulder arthroplasty versus reverse total shoulder arthroplasty in patients aged over 70 without a full-thickness rotator cuff tear: A systematic review and meta-analysis. J Shoulder Elb Arthroplast 2023;7:24715492231206685. [Google Scholar]
- 7.Ma GC, Bradley KE, Jansson H, Feeley BT, Zhang AL, Ma CB. Surgical complications after reverse total shoulder arthroplasty and total shoulder arthroplasty in the United States. J Am Acad Orthop Surg Glob Res Rev 2021;5:e21.00146. [Google Scholar]
- 8.Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J Shoulder Elbow Surg 2011;20:146-57. [Google Scholar]
- 9.Mencia MM, Goalan R, Skeete R. Atraumatic dissociation of a modular shoulder hemiarthroplasty: A case report and literature review. JSES Int 2020;4:400-3. [Google Scholar]
- 10.Kaymakoglu M, Aral F, Huri G. Failure of a reverse total shoulder arthroplasty with a broken humeral stem tray: A case report. J Orthop Case Rep 2023;13:111-4. [Google Scholar]
- 11.McDonald LS, Dines JS, Chin C, Warren RF, Dines DM. Humeral tray-taper failure in modular reverse total shoulder arthroplasty. HSS J 2016;12:8-12. [Google Scholar]
- 12.Lewicki KA, Martin AJ, Bell JE, Van Citters DW. Fatigue failure of reverse shoulder humeral tray components of a single design. J Shoulder Elbow Surg 2016;25:1288-96. [Google Scholar]
- 13.Kim MS, Jeong HY, Kim JD, Ro KH, Rhee SM, Rhee YG. Difficulty in performing activities of daily living associated with internal rotation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2020;29:86-94. [Google Scholar]
- 14.Ernstbrunner L, Wieser K, Catanzaro S, Agten CA, Fornaciari P, Bauer DE, et al. Long-term outcomes of pectoralis major transfer for the treatment of irreparable subscapularis tears: Results after a mean follow-up of 20 years. J Bone Joint Surg Am 2019;101:2091-100. [Google Scholar]
- 15.Updegrove G, Kohler J, Ponnuru P, Armstrong AD. Pectoralis major tendon transfer for management of subscapularis failure after anatomic total shoulder arthroplasty: Technique and results. JSES Rev Rep Tech 2022;2:451-7. [Google Scholar]
- 16.Burkhard MD, Grubhofer F, Wieser K, Elhassan BT. Pedicled pectoralis major transfer for irreparable dehiscence of the deltoid in reverse total shoulder arthroplasty: Surgical technique and case report. JSES Rev Rep Tech 2021;1:218-23. [Google Scholar]
- 17.Werthel JD, Schoch BS, Hooke A, Sperling JW, An KN, Valenti P, et al. Biomechanical effectiveness of tendon transfers to restore active internal rotation in shoulder with deficient subscapularis with and without reverse shoulder arthroplasty. J Shoulder Elbow Surg 2021;30:1196-206. [Google Scholar]
- 18.Hao KA, Cueto RJ, Gharby C, Freeman D, King JJ, Wright TW, et al. Influence of lateralized versus medialized reverse shoulder arthroplasty design on external and internal rotation: A systematic review and meta-analysis. Clin Shoulder Elb 2023;27:59-71. [Google Scholar]
- 19.Longo UG, Franceschetti E, Carnevale A, Schena E, Cozza G, Perricone G, et al. Influence of lateralization and distalization on joint function after primary reverse total shoulder arthroplasty. Bioengineering (Basel) 2023;10:1409. [Google Scholar]
- 20.Lauria M, Hastings M, DiPaola MJ, Duquin TR, Ablove RH. Factors affecting internal rotation following total shoulder arthroplasty. JSES Rev Rep Tech 2022;2:431-6. [Google Scholar]
- 21.Gruber MD, Kirloskar KM, Werner BC, Lädermann A, Denard PJ. Factors associated with internal rotation after reverse shoulder arthroplasty: A narrative review. JSES Rev Rep Tech 2022;2:117-24. [Google Scholar]
- 22.Nunes B, Linhares D, Costa F, Neves N, Claro R, Silva MR. Lateralized versus nonlateralized glenospheres in reverse shoulder arthroplasty: A systematic review with meta-analysis. J Shoulder Elbow Surg 2021;30:1700-13. [Google Scholar]
- 23.Luster TG, Dean RS, Trasolini NA, Eichinger JK, Parada SA, Ralston RK, et al. Predictive factors influencing internal rotation following reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2023;33:1200-8. [Google Scholar]
- 24.Kim SC, Lee JE, Lee SM, Yoo JC. Factors affecting internal rotation after reverse shoulder arthroplasty. J Orthop Sci 2022;27:131-8. [Google Scholar]
- 25.Gibian JT, Sokrab R, Hill JR, Keener JD, Zmistowski BM. Predictors of internal rotation after reverse shoulder arthroplasty. Arch Bone Jt Surg 2023;11:696-703. [Google Scholar]