Simultaneous knee replacement should be considered in patients with severe pre-operative bilateral knee deformities, including arthrodesis to optimize post-operative recovery.
Ms. Morgan K Villa, Virginia Commonwealth University School of Medicine, Richmond, VA, USA. E-mail: villamk@vcu.edu
Introduction: Juvenile idiopathic arthritis (JIA) poses lifelong challenges due to chronic inflammation that can lead to permanent deformities like autofusion, severely affecting quality of life.
Case Report: In this case, a 31-year-old female with a 21-year history of bilateral knee pain secondary to JIA faced a unique challenge: bilateral knee autofusion. Radiographs revealed severe bilateral contractures, erosive changes, and autofusion, prompting the decision for simultaneous total knee arthroplasties (TKAs). Evaluation at 1-year postoperatively showed significant improvements in function, pain, and activities of daily living.
Conclusion: This case provides insight into outcomes of simultaneous TKAs in the context of autofusion, highlighting the procedure’s viability in resolving debilitating knee conditions, even in the presence of complex factors such as JIA.
Keywords: Simultaneous total knee arthroplasties, autofusion, juvenile idiopathic arthritis.
Juvenile idiopathic arthritis (JIA) is a complex autoimmune disease that leads to joint destruction and can cause permanent deformity in children. JIA is often a disabling condition that has long-term effects on patient quality of life. In cases of JIA where the disease progresses despite conservative management, surgical intervention may become necessary. Joint replacement surgery, including total knee arthroplasty (TKA), can alleviate pain and restore mobility in patients with severe arthropathy. Conversion of prior knee arthrodesis to total knee comes with distinct technical challenges often requiring use of tissue expanders due to difficult exposure and insufficient closure, patellar and tibiofemoral osteotomies, and significant soft tissue release to improve angular and flexion deformities. In addition to these risks, converted knees traditionally have higher rates of post-operative skin necrosis, arthrofibrosis, infection, and extensor insufficiency [1]. Here, we present a patient with spontaneous bilateral arthrodesis as a consequence of JIA who subsequently underwent simultaneous bilateral TKA at our institution.
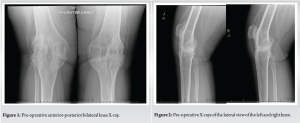
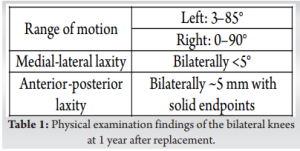
A 31-year-old female presented for evaluation of chronic bilateral knee pain secondary to polyarticular JIA diagnosed in childhood. She reported a 21-year history of knee pain and stiffness that severely impaired her ability to perform activities of daily life. Her symptoms persisted despite several years of medical management including methotrexate, hydroxychloroquine, tofacitinib, and adalimumab. At the age of 21, she underwent right total hip arthroplasty due to the progression of symptoms despite conservative treatment. On examination, she walked with an antalgic, stiff-legged gait. Range of motion was extremely limited, as both knees had fixed flexion contractures of 25° beyond with no further flexion (Table 1). She had bilateral swelling and crepitation with movement. Bilateral knee radiographs demonstrated bilateral erosive changes consistent with Kellgren-Lawrence stage four changes and severe contractures. Lateral views demonstrated fixed flexion with continuous trabeculae spanning the tibiofemoral joint, consistent with bilateral autofusion. The patient was counseled to consider conservative treatments including weight management, physical therapy, pain management through over-the-counter medications, and evaluation by her rheumatologist before pursuing surgical management. She returned after an unsuccessful trial of these modalities, including a 60-pound weight loss and medical therapy with apremilast. At this visit, staged versus simultaneous bilateral TKA was discussed, including a potentially increased complication risk with bilateral simultaneous TKA, weighed against a single rehabilitation with both knees replaced, given the fixed flexion contracture of her knees. The patient elected for simultaneous bilateral TKA. Long leg views were obtained in addition to AP and lateral views for pre-operative planning and implant sizing (Fig. 1-3).

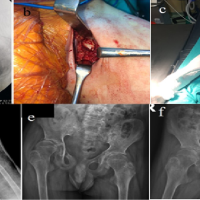
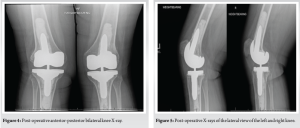
Total knee arthroplasties were performed using free-hand resection at the joint line followed by the modified utilization of standard instrumentation and fluoroscopic guidance. One of the difficulties we faced was gaining adequate exposure and alignment, given the extent of ankylosis of the bilateral patellofemoral and tibiofemoral joints, which required careful resection of both bone and soft tissue. In particular, the patella had to be carefully freed from the femur using a Cobb elevator, and a partial lateral facetectomy was performed due to the thin, friable bone that increased the risk of patellar fracture. The use of fluoroscopy in conjunction with extramedullary guides, rather than intramedullary guides, for tibial resection was advantageous in achieving precise alignment and proper implant placement in the presence of severe deformities, while also helping to reduce the risk of blood loss and transfusions [2]. Postoperatively, the patient was able to bear weight as tolerated with unlocked bilateral hinged knee braces. The epidural was removed on post-operative day 2 and the patient was transitioned to oral multimodal pain management including anti-inflammatories, opioids, and analgesics. The hospital course was complicated by persistent tachycardia and an episode of supraventricular tachycardia on post-operative day 4, which required medical management and extended her hospital stay. She was discharged to an inpatient rehabilitation facility on post-operative day 7. At 15-month follow-up evaluation and imaging, she reported improvement in her function, and ability to perform activities of daily living since the operation due to increased exercise tolerance and continued dietary modification (Figs. 4 and 5). She was walking without ambulatory aid and had returned to employment without restrictions. On examination, her range of motion had improved to 0–90° on the right, 3–85° on the left, with no lag. Medial-lateral laxity was <5° bilaterally (Table 1). Both knees had approximately 5 mm of anterior posterior laxity with solid endpoints.
JIA is a chronic autoimmune disease that affects individuals under the age of 16 and is characterized by synovial inflammation leading to joint stiffness, swelling, and persistent pain if not adequately controlled [3]. Even with early intervention, JIA can lead to permanent joint damage, limb length inequality, and disability necessitating joint replacement in adolescence or adulthood to improve pain and mobility [4-6]. The knee is the most commonly affected joint in JIA patients [7]. Patients with earlier onset of disease or longer duration of disease are at risk for more severe joint damage, increasing the likelihood of requiring joint replacement surgery [6,8]. In addition, severe disease is more likely in the polyarticular and systemic subtypes, with some studies reporting up to 50% of adolescents with these subtypes ultimately undergoing a knee replacement due to disease in adulthood [3,7]. Joint replacement in adulthood can serve as a viable option for severe arthropathy to provide pain relief and restore bony alignment. A retrospective study performed by Malviya et al. found significant improvement in pain relief and quality of life in patients with JIA who undergo TKA [5]. However, this study reported low functional outcomes and a high 20-year rate of revision at 58.2%. This can be partially attributed to pre-operative deformity as well as younger average age at replacement, leading to increased activity demand and extended component wear over time. A study performed by Ranawat et al. reported favorable outcomes in 27 out of 29 knees and significant improvement in disability ratings after TKA for JIA, highlighting the marked improvement in patient-reported and functional outcomes [9]. Further, a meta-analysis reported that patients exhibited high satisfaction postoperatively with TKA as compared to their previously fused knees [1]. Simultaneous bilateral knee replacements can be considered in otherwise healthy patients with significant bilateral deformities. These patients may experience elevated morbidity rates and encounter more challenging short-term recovery especially if they are not at optimum health. A meta-analysis performed by Liu et al. found that patients who underwent simultaneous TKA had a lower risk of deep joint infections, but an increased risk of DVT and PE compared to staged bilateral TKA [10]. These risks may be mitigated by early mobilization, prophylactic anticoagulation, and medical intervention. In a retrospective database review, simultaneous knee arthroplasties had a higher incidence of both major complications and overall complications compared to staged arthroplasties [11]. This was most distinct in patients with more significant comorbidity burden. However, a better estimate of risk could be elucidated by the study of aggregate adverse complications of two sequential unilateral knee arthroplasties performed during separate hospital admissions, as comparing bilateral and unilateral knee replacements may underestimate complications in the single-knee group [11]. The surgeon should consider both medical complications and patient-related factors in patient selection to reduce post-operative complications. Memtsoudis et al. published a committee review of expert perceptions on same-day TKA protocols [12]. Overall, the committee supported the exclusion of patients who have an American Society of Anesthesiologists Class III or greater condition, a history of ischemic cardiomyopathy, a body mass index >40, renal insufficiency, or >75 years. An ideal candidate would be young, without serious medical comorbidity, obesity, with severe arthropathy, as in the case of our patient. In addition, among patients with low comorbidity scores, the incidence of major complications was relatively low, at 2.5% in a retrospective database review performed by Warren et al. [11]. In addition, Dimitris et al. noted the major complication rate within their cohort was 3.5% and not significantly elevated compared to the unilateral group [13]. Simultaneous procedures could reduce overall hospital length of stay (LOS) in the patient with severe bilateral arthropathy [6,13,14]. Dimitris et al. found a <10% difference in average LOS when comparing bilateral simultaneous versus unilateral TKA. In addition, Yoon et al. noted a significantly longer average LOS of hospital admissions for staged bilateral TKAs when compared to simultaneous bilateral TKAs. They also noted a 5.0% major complication rate in simultaneous procedures, compared to 0.8% for staged arthroplasties. However, all patients who had a complication in the simultaneous bilateral TKA group were over the age of 70, emphasizing the importance of candidate selection in the reduction of adverse outcomes. The technical complexities and potential complications associated with the conversion of arthrodesis to TKA necessitate a thorough discussion. These conversions are complex procedures requiring detailed pre-operative planning and surgical precision, particularly given the altered anatomy and presence of scar tissue from previous operations. The conversion typically involves meticulous dissection and soft-tissue release, along with the excision of bony bridges, to re-establish joint movement. To manage the limited soft-tissue around the knee, techniques such as soft-tissue expansion may be utilized [15,16]. In addition, the type of prosthesis selected is often dictated by the integrity of the collateral ligaments, with constrained knee prostheses or hinged components favored, given the soft-tissue releases necessary for exposure [17]. Conversion from arthrodesis to TKA is associated with significant complications, with reported overall complication rates between 47% and 65% [1,18]. These complications include skin necrosis, arthrofibrosis, infection, and mechanical failures such as rupture of the extensor mechanism, leading to a notable revision rate of 25% and a failure rate of 11% within 5 years. These results emphasize the necessity for careful post-operative monitoring to manage potential challenges and ensure optimal patient outcomes [1,18]. Several studies have emphasized that successful conversion to TKA relies on proper patient selection, surgical techniques, surgeon experience, and effective complication management [1, 18-20]. Moreover, while patients may seek a significant improvement in their quality of life, they must be counseled extensively of the potential risks. Studies indicate that patients may achieve functional improvements and report high satisfaction after surgery, but the considerable risk of complications underscores the importance of thorough patient counseling and the management of expectations [1, 16-19].
In adolescence, the mainstay of treatment for JIA is preventing joint damage, pain, and maintaining functionality. As patient’s transition into adulthood and conservative treatment options fail to control disease or prevent arthropathy, joint replacement surgery can restore joint function and mitigate pain. Simultaneous knee replacement can be a successful treatment in select patients for severe bilateral joint deformity, such as those with bilateral arthrodesis, to optimize post-operative rehabilitation.
In specific cases, simultaneous knee replacement can serve as an effective remedy for severe bilateral joint deformities, particularly for individuals with bilateral arthrodesis to optimize post-operative recovery.
References
- 1.Kernkamp WA, Verra WC, Pijls BG, Schoones JW, van der Linden HM, Nelissen RG. Conversion from knee arthrodesis to arthroplasty: Systematic review. Int Orthop 2016;40:2069-74. [Google Scholar | PubMed]
- 2.Li M, Li J, Hu S, Jia B. Comparison of intramedullary versus extramedullary alignment technique in total knee arthroplasty: A PRISMA-compliant meta-analysis. Medicine (Baltimore) 2023;102:e32277. [Google Scholar | PubMed]
- 3.Pertusi RM, Rubin BR, Blackwell D. Juvenile rheumatoid arthritis. J Am Osteopath Assoc 1996;96:298-302. [Google Scholar | PubMed]
- 4.Taxter A, Donaldson BC, Rigdon J, Harry O. Association between patient-reported outcomes and treatment failure in juvenile idiopathic arthritis. ACR Open Rheumatol 2022;4:775-81. [Google Scholar | PubMed]
- 5.Malviya A, Foster HE, Avery P, Weir DJ, Deehan DJ. Long term outcome following knee replacement in patients with juvenile idiopathic arthritis. Knee 2010;17:340-4. [Google Scholar | PubMed]
- 6.Yoon HS, Han CD, Yang IH. Comparison of simultaneous bilateral and staged bilateral total knee arthroplasty in terms of perioperative complications. J Arthroplasty 2010;25:179-85. [Google Scholar | PubMed]
- 7.Rojer DE, Goodman SB. Total knee replacement in juvenile rheumatoid arthritis. Orthopedics 2005;28:39-47. [Google Scholar | PubMed]
- 8.Minden K, Niewerth M, Listing J, Biedermann T, Bollow M, Schöntube M, et al. Long-term outcome in patients with juvenile idiopathic arthritis. Arthritis Rheum 2002;46:2392-401. [Google Scholar | PubMed]
- 9.Ranawat CS, Bryan WJ, Inglis AE. Total knee arthroplasty in juvenile arthritis. Arthritis Rheum 1983;26:1140-4. [Google Scholar | PubMed]
- 10.Liu L, Liu H, Zhang H, Song J, Zhang L. Bilateral total knee arthroplasty: Simultaneous or staged? A systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e15931. [Google Scholar | PubMed]
- 11.Warren JA, Siddiqi A, Krebs VE, Molloy R, Higuera CA, Piuzzi NS. Bilateral Simultaneous total knee arthroplasty may not be safe even in the healthiest patients. J Bone Joint Surg Am 2021;103:303-11. [Google Scholar | PubMed]
- 12.Memtsoudis SG, Hargett M, Russell LA, Parvizi J, Cats-Baril WL, Stundner O, et al. Consensus statement from the consensus conference on bilateral total knee arthroplasty group. Clin Orthop Relat Res 2013;471:2649-57. [Google Scholar | PubMed]
- 13.Dimitris CN, Taylor BC, Mowbray JG, Steensen RN, Gaines ST. Perioperative morbidity and mortality of 2-team simultaneous bilateral total knee arthroplasty. Orthopedics 2011;34:841-6. [Google Scholar | PubMed]
- 14.Parvizi J, Rasouli MR. Simultaneous-bilateral TKA: Double trouble - affirms. J Bone Joint Surg Br 2012;94:90-2. [Google Scholar | PubMed]
- 15.Mahomed N, McKee N, Solomon P, Lahoda L, Gross A. Soft-tissue expansion before total knee arthroplasty in arthrodesed joints. A report of two cases. J Bone Joint Surg Br 1994;76-B:88-90. [Google Scholar | PubMed]
- 16.Cho SH, Jeong ST, Park HB, Hwang SC, Kim DH. Two-stage conversion of fused knee to total knee arthroplasty. J Arthroplasty 2008;23:476-9. [Google Scholar | PubMed]
- 17.Henkel TR, Boldt JG, Drobny TK, Munzinger UK. Total knee arthroplasty after formal knee fusion using unconstrained and semiconstrained components: A report of 7 cases. J Arthroplasty 2001;16:768-76. [Google Scholar | PubMed]
- 18.Jauregui JJ, Buitrago CA, Pushilin SA, Browning BB, Mulchandani NB, Maheshwari AV. Conversion of a surgically arthrodesed knee to a total knee arthroplasty-is it worth it? A meta-analysis. J Arthroplasty 2016;31:1736-41. [Google Scholar | PubMed]
- 19.Abdelazim H, Hashem MH. Conversion total knee arthroplasty after arthrodesis using rotatory hinge revision system. Egypt Orthop J 2019;54:154. [Google Scholar | PubMed]
- 20.Wood JH, Conway JD. Advanced concepts in knee arthrodesis. World J Orthop 2015;6:202-10. [Google Scholar | PubMed]