This article is intended to provide a step-by-step guide for others to fuse the sacroiliac joint with the iFuse-TORQ implant under Stealth navigation.
Dr. Jia Bao Lin, Department of Orthopedic Surgery, OhioHealth Doctors Hospital, OH, USA. E-mail: johnlin1122@gmail.com
Introduction: Dysfunction of the sacroiliac (SI) joint exists in nearly one-third of patients with lower back pain. There are nuances in diagnosing SI joint dysfunction with a combination of physical exam maneuvers and intra-articular injections. The management of patients with SI joint pain can include posterior pelvic fixation, which traditionally has been described using fluoroscopy to obtain safe placement of implants.
Case Report: In this technique guide, we would like to introduce a novel technique of using Stealth navigation to facilitate SI fusion with the iFuse-TORQ implant.
Conclusion: SI dysfunction is a common cause of low back pain that can be difficult to diagnose and treat. In this technique guide, we describe the successful treatment of SI pathology using the Stealth Navigation with the iFuse-TORQ implant.
Keywords: Sacroiliac joint, iliosacral screw, o-arm, stealth navigation, fusion, arthrodesis, sacroiliac joint.
Sacroiliac (SI) joint dysfunction is a well-known pain generator, and it is important to correctly differentiate from existing lumbar pathology; it has been noted that 15–30% of lower back pain is originating from the SI joints [1-3] There is no single physical exam maneuver or imaging that is diagnostic of SI joint dysfunction, which makes it difficult to diagnose, however, intra-articular SI joint injections can serve as a reliable diagnostic method [1]. When correctly diagnosed, patients who fail conservative measures are able to find relief with various options of SI joint fixation, and 33 different devices have been utilized for this procedure [4]. Minimally invasive SI joint fusion has been shown to improve pain, physical function, and quality of life when compared to conservative management [5]. This novel technique of fusing the SI joint with the iFuse-TORQ implant (SI-BONE, Inc., Santa Clara, CA) with Stealth navigation (Medtronic, Minneapolis, MN) has not yet been described in the literature, although navigation is an emerging standard for posterior pelvic fixation [6].
Patients are positioned supine on a radiolucent table with a presacral bump to enable proper trajectory without hitting the table while allowing for bilateral iliosacral screws placement as needed. The legs are allowed to externally rotate and standard preparation and draping technique is applied. Proximally, the iliac crests should be exposed, and the lateral aspects of the patient should be draped as low as possible near the gluteal folds. Draping is then completed at the level of the pubic symphysis. For the Stealth navigation system, a small incision is made through the skin, overlying the palpable ilium, just one finger breadth proximal to the anterior superior iliac spine (Fig. 1a). The registration post is manually impacted into the ilium without predrilling, being mindful to mimic the trajectory of the iliac wing to keep the post within the inner and outer tables (Fig. 1b).The array is then attached and rotated to the appropriate number so that the sensors are viewable at all times by the Stealth unit (Fig. 1c).
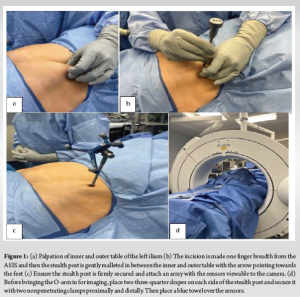
Next, the field is covered with two three-quarter sheets and clipped together around the array with a towel over the top of the array as the O-arm machine was brought in to maintain a sterile field (Fig. 1d). Initial radiographs are taken by the O-arm machine to ensure that the area of interest was centered on the screen, in this case, the posterior ring and sacrum. Once confirmed to be in the appropriate position, the towel is removed from the array for visualization, and an O-arm spin is performed on the low radiation setting. Preoperatively, the anticipated iliosacral screw trajectories are templated and measured, and this is again confirmed with the Stealth system. The navigated aiming gun is cannulated and allows real-time visualization of the guide wire for safety in placement (Fig. 2a, b, c). Initially, the navigated gun is used to find the rough starting point against the skin to allow appropriate incision placement (Fig. 2d). Next, the navigated gun is taken all the way down to the bone and an appropriate initial trajectory for our first right iliosacral screw is found and confirmed on Stealth navigation.
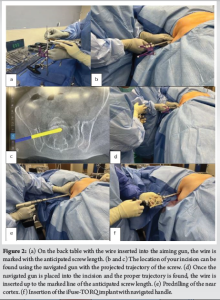
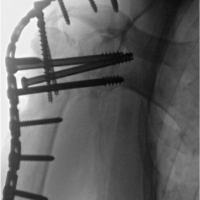
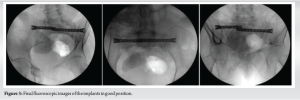
Once the appropriate trajectory is confirmed, the drill tip wire is passed through the guide/gun and advanced to the marked depth as templated preoperatively and confirmed intraoperatively. The aiming gun is then removed and the near cortex will require pre-drilling before moving to the contralateral side (Fig. 2e). The steps can then be repeated for additional screws on the ipsilateral or contralateral side.To ensure safety in placement of the wires, a second spin is performed in an identical fashion to the first spin. The images are then confirmed for safe wire placement and also to determine if anticipated screw lengths were appropriate.At this time, the screws can be placed without navigation, or a calibrated sensor can be utilized to follow the screw depth insertion in real-time (Fig. 2f). For final evaluation, wires are removed, and c-arm fluoroscopy is brought in for final assessment. Multiple radiographs are obtained (inlet, outlet, anteroposterior, and tangential views of the posterolateral ilium) to ensure that all screws are flush on bone and safe from the neural foramen (Fig. 3).
At this point, arrays on the ilium are removed and wounds are irrigated; layered closure is then performed, and small island dressings are utilized. Patients can be made weight-bearing as tolerated and discharged on the same day.
The presence of lower back pain can be a debilitating condition, affecting a patient’s ability to perform activities of daily living. This disease burden affects people worldwide at an annual prevalence of 15–45% [7]. It is imperative to differentiate the pain generators of the lower back as SI joint pain can have very similar presentations to lower lumbar and hip pathology. This would help mitigate unnecessary surgical intervention as some failed lower back pain surgery came from erroneous diagnoses, i.e., asymptomatic magnetic resonance imaging findings [8,9]. In the past, SI joint dysfunction was not widely recognized as a harbinger of lower back pain, but with increasing recognition over the last decade and the advent of minimally invasive procedures for SI joint fusion, it has shown to be an effective solution to this problem [10]. The prevalence of lower back pain that is originating from the SI joints is approximately 15–30% [1-3]. Once conservative management has been exhausted, SI joint fusion has been shown to be a reliable option to improve pain, function, and quality of life [5]. Since the introduction of the triangular titanium implants from SI-BONE for SI joint fusion in 2009, there has been ongoing innovation to create additional implants to include the iFuse-TORQ implant that is used in this step-by-step guide. Similar to the triangular titanium implant, it is porous coated to facilitate osseointegration. The helical flutes and fenestrations allow it to self-harvest bone, along with its self-drilling and self-tapping features to minimize surgical steps. Another distinguishing feature of this implant is the hooked profile of the threads to mitigate toggle and compared to the traditional screw its torque pull-out strength is 23 times greater. With its unique design, the iFuse-TORQ implant is much more robust when it comes to posterior pelvic fixation and SI joint fusion (SI Bone:https://si-bone.com/) [11]. Using traditional fluoroscopy guidance for the placement of SI screws or implants has been widely adopted in current practice for posterior pelvic instrumentation. However, another safe and effective way is with technological advancements like the O-arm, which can provide 3D intraoperative computed tomography scans and Stealth navigation to use this data and navigate screws. This enabling technology has been shown to significantly reduce radiation doses to the patient and medical staff, as well as time for SI joint fixation [6]. There have also been cadaveric studies that demonstrated greater precision and accuracy with screw placements when using 3D navigation [12,13]. Accuracy is crucial when implants are placed in the pelvis due to significant morbidity if these proximate structures, L5/S1 nerve roots, super gluteal and internal iliac arteries are compromised [6]. SI joint fusion can be obtained using a wide variety of implants and it can be safely performed with traditional fluoroscopy or navigated with the O-arm and Stealth technology. Our method of using Stealth navigation with the iFuse-TORQ implant has been successfully completed in two patients who found relief and left on the same day of surgery. We hope this guide will enable others to safely navigate the pelvis for SI joint fusion in patients with SI joint dysfunction.
In conclusion, SI dysfunction is a common cause of low back pain that can be debilitating for patients. In this technique guide, we describe the successful treatment of SI pathology using the Stealth Navigation with the iFuse-TORQ implant. We hope that this technique guide will allow surgeons to safely perform SI joint fusion using this implant to successfully treat those with SI joint dysfunction.
Dysfunction of the SI joint can be debilitating for patients when performing activities of daily living. This pathology can be difficult to diagnose and treat. In this technique guide, we present a novel technique of using Stealth navigation to facilitate SI fusion with the iFuse-TORQ implant.
References
- 1.Buchanan P, Vodapally S, Lee DW, Hagedorn JM, Bovinet C, Strand N, et al. Successful diagnosis of sacroiliac joint dysfunction. J Pain Res 2021;14:3135-43. [Google Scholar | PubMed]
- 2.Polly DW Jr. The sacroiliac joint. Neurosurg Clin N Am 2017;28:301-12. [Google Scholar | PubMed]
- 3.Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac joint pain and its treatment. Clin Spine Surg 2016;29:42-8. [Google Scholar | PubMed]
- 4.Himstead AS, Brown NJ, Shahrestani S, Tran K, Davies JL, Oh M. Trends in diagnosis and treatment of sacroiliac joint pathology over the past 10 years: Review of scientific evidence for new devices for sacroiliac joint fusion. Cureus 2021;13:e15415. [Google Scholar | PubMed]
- 5.Chang E, Rains C, Ali R, Wines RC, Kahwati LC. Minimally invasive sacroiliac joint fusion for chronic sacroiliac joint pain: A systematic review. Spine J 2022;22:1240-53. [Google Scholar | PubMed]
- 6.Passias BJ, Grenier G, Buchan J, Buchan DR, Scheschuk J, Taylor BC. Use of 3D navigation versus traditional fluoroscopy for posterior pelvic ring fixation. Orthopedics 2021;44:229-34. [Google Scholar | PubMed]
- 7.Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA, American Society of Interventional Pain Physicians. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician 2009;12:E35-70. [Google Scholar | PubMed]
- 8.Ackerman SJ, Polly DW Jr., Knight T, Holt T, Cummings J Jr. Nonoperative care to manage sacroiliac joint disruption and degenerative sacroiliitis: High costs and medical resource utilization in the United States Medicare population. J Neurosurg Spine 2014;20:354-63. [Google Scholar | PubMed]
- 9.Ackerman SJ, Polly DW Jr., Knight T, Schneider K, Holt T, Cummings J Jr. Comparison of the costs of nonoperative care to minimally invasive surgery for sacroiliac joint disruption and degenerative sacroiliitis in a United States commercial payer population: Potential economic implications of a new minimally invasive technology. Clinicoecon Outcomes Res 2014;6:283-96. [Google Scholar | PubMed]
- 10.Vanaclocha-Vanaclocha V, Sáiz-Sapena N, Vanaclocha L. Sacroiliac joint pain: Is the medical world aware enough of its existence? Why not considering sacroiliac joint fusion in the recalcitrant cases? J Spine Surg 2019;5:384-6. [Google Scholar | PubMed]
- 11.SI-bone; 2024. Available from: https://si-bone.com [Last accessed on 2024 May 27]. [Google Scholar | PubMed]
- 12.Takao M, Nishii T, Sakai T, Yoshikawa H, Sugano N. Iliosacral screw insertion using CT-3D-fluoroscopy matching navigation. Injury 2014;45:988-94. [Google Scholar | PubMed]
- 13.Behrendt D, Mütze M, Steinke H, Koestler M, Josten C, Böhme J. Evaluation of 2D and 3D navigation for iliosacral screw fixation. Int J Comput Assist Radiol Surg 2012;7:249-55. [Google Scholar | PubMed]