Recognition and management of spontaneous iliacus muscle hematomas as a rare cause of femoral neuropathy. It highlights the importance of early diagnosis and appropriate management to prevent long-term complications, especially in cases without apparent trauma or anticoagulation therapy. The case study emphasizes the need for thorough clinical assessment and imaging studies, as well as the potential for conservative treatment to yield successful recovery.
Dr. Rui Sousa, Viseu Dão-Lafões Local Health Unit – Av. Rei Dom Duarte, 3504-509 Viseu. E-mail: ruivmsousa@gmail.com
Introduction: Femoral neuropathy is a rare condition typically resulting from compression of the femoral nerve. While it is commonly associated with anticoagulated patients due to psoas hematomas, spontaneous iliacus muscle hematomas without any evident trauma or coagulation disorders are exceedingly uncommon. This case report details the occurrence and management of a spontaneous iliacus muscle hematoma in an adolescent patient. Such cases have been scarcely reported, making this documentation critical for enhancing clinical understanding and management strategies.
Case Report: A 16-year-old male of Caucasian ethnicity, with no significant medical history, presented with thigh muscle atrophy, decreased strength in the left lower limb, and progressive loss of weight-bearing capacity over a month. The patient reported no history of trauma. Clinical examination revealed hypoesthesia in the femoral nerve territory and significantly reduced quadriceps muscle strength. Imaging studies, including magnetic resonance imaging, identified a fusiform mass deep to the left iliac muscle, consistent with an encapsulated hematoma. The patient was treated conservatively with rest and analgesics, followed by physical rehabilitation. Follow-up assessments showed progressive improvement in muscle trophism and weight-bearing capacity, with complete recovery of femoral nerve conduction at 1 year.
Conclusion: This case underscores the importance of considering spontaneous iliacus muscle hematomas in the differential diagnosis of femoral neuropathy, even in the absence of trauma or anticoagulation therapy. The report highlights the necessity for thorough clinical evaluation and imaging to ensure accurate diagnosis. It adds valuable information to the orthopedic literature, particularly in managing rare presentations of femoral neuropathy, emphasizing the need for vigilance in monitoring and follow-up to prevent long-term complications. By detailing this unusual presentation, the report aims to enhance the understanding and treatment strategies for similar cases.
Keywords: Femoral neuropathy, Iliac hematoma, conservative management, adolescent
Femoral neuropathy is an uncommon condition, typically resulting from a compressive etiology. The femoral nerve can be compromised in the retroperitoneal space, particularly at the level of the psoas-iliac groove. Psoas hematoma is a compressive etiology most frequently described in anticoagulated patients and occurring in about 7% of them [1]. However, this type of pathology has occasionally been described in patients not harboring primary or secondary coagulation disorders [2]. There is often a delay in the diagnosis as it presents subtly and non-specifically, generally with hip or groin pain, hip flexion contracture, and femoral nerve paresthesias [3]. We present a case of an adolescent patient with a spontaneous iliacus muscle hematoma, with no history of trauma or other apparent cause.
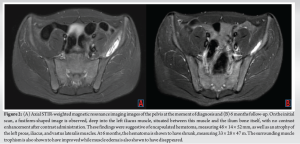
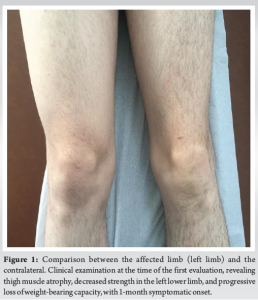
A 16-year-old Caucasian male with no significant medical history presented with a 1-month history of thigh muscle atrophy, decreased strength in the left lower limb, and progressive loss of weight-bearing capacity (Fig. 1). There was no history of trauma. Clinically, he exhibited hypoesthesia in the femoral nerve innervation territory and a 2/5 quadriceps muscle strength. Radiographs revealed diffuse osteopenia of the femur and tibia. Electromyography (EMG) revealed femoral nerve disfunction with a severe decrease in the femoral nerve conduction. Magnetic resonance imaging (MRI) showed a fusiform mass located deep in the left iliac muscle, measuring 48 × 14 × 52 mm, with no contrast enhancement after contrast administration, consistent with an encapsulated hematoma. In addition, atrophy of the thigh musculature, as well as the psoas and iliac muscles, was observed (Fig. 2a). The patient was managed conservatively with rest, and analgesics were referred to a physical and motor rehabilitation clinic. At the 2-month follow-up, he presented with progressive recovery of muscle trophism and weight-bearing capacity, with significant clinical improvement at 6-month follow-ups. A follow-up MRI showed a reduction in the size of the hematoma (Fig. 2b). At 1 year follow-up, EMG indicated a complete recovery of femoral nerve conduction.
The femoral nerve originates from the posterior branches of the ventral rami of the L2–L4 spinal roots. It travels through the psoas major muscle, moves between the groove formed by the psoas and iliacus muscles, and exits the pelvis below the inguinal ligament, positioned near the femoral artery and vein. This nerve supplies the iliacus, sartorius, and quadriceps muscles (including the rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis). In addition, its terminal cutaneous branches provide sensation to the anterior thigh (through the anterior femoral cutaneous nerve) and the medial distal leg (through the saphenous nerve) [2]. Expansive lesions in the psoas or iliacus muscles can lead to femoral neuropathy by either direct compression or local nerve ischemia and may result in iliacus compartment syndrome [4]. The most common lesion in the iliacus muscle is a hematoma, which is a major complication associated with anticoagulant therapy or hemophilia [5]. However, other muscle mass lesions such as abscesses, tumors (including neurofibromas), and lymphadenopathies can also cause femoral compressive neuropathy [6]. In addition, the femoral nerve can be damaged during surgical procedures involving the abdomen, pelvis, or hip [7], as well as during pregnancy [8]. Femoral neuropathy resulting from iliacus or psoas hematomas, although rare, presents significant clinical challenges and underscores the importance of prompt diagnosis and appropriate management to prevent long-term deficits [2]. Hematomas in this region present insidiously and are not heralded by an obvious lesion or ecchymosis [9]. Diagnosis is frequently delayed due to its subtle and non-specific presentation, typically manifesting as hip flexion contracture, hip or groin pain, and femoral nerve paresthesias [3]. Subperiosteal hematoma (SPH) of the iliac bone is another extremely rare occurrence usually seen in adolescents after trauma [10-14]. The underlying pathophysiology of a subperiosteal iliac hematoma is believed to be secondary to traction on the loosely attached periosteum, elevated secondary to blunt trauma, often from a fall onto the buttocks. This injury is seen primarily in athletic adolescents without any history of bleeding disorder or blood thinning medications, most likely because of their strong pelvic musculature pulling on the relatively weak Sharpey’s fibers of the periosteum in the setting of high-impact activities. SPH can also lead to femoral nerve palsy due to the mass effect on the femoral nerve as it drapes over the iliacus muscle and passes into the femoral canal [10]. Some cases of post-traumatic SPH, especially after sports trauma, have also been described [10, 15]. In these cases, the presence of an expanding hematoma, transcatheter arterial embolization of the affected vessels, or surgical evacuation of the hematoma may be required to treat the hematoma itself or femoral neuropathy [11, 12, 14]. Although rare in children and young adults, intra-tumoral hemorrhage should be considered in patients presenting with spontaneous hematomas. The most common underlying diagnosis is malignant fibrous histiocytoma, with cases reported in the iliopsoas muscle [16, 17]. Patients with spontaneous hematomas that do not resolve as expected should be viewed with particular suspicion. It is advisable to monitor such patients to ensure complete resolution and confirm the absence of an underlying tumor [18]. Due to the rarity of this condition, identifying the exact etiology in this case is inherently challenging. While it is plausible that a minor, unrecognized trauma may have been a contributing factor, other possibilities such as subclinical or undetected physiological conditions cannot be ruled out. The lack of any clear pre-disposing factors highlights the diagnostic complexity associated with spontaneous iliacus muscle hematomas, emphasizing the need for further investigation and reporting of similar cases to better understand their underlying mechanisms. There is no consensus or guidelines regarding the best optimal treatment for spontaneous hematoma. Non-operative treatment has been described to be recommended for patients on anticoagulation therapy or those with bleeding disorders as well as patients with mild-to-moderate femoral nerve palsy associated to small hematoma. Surgical decompression of the hematoma or trans-catheter arterial embolization is generally advised for cases of severe hemorrhage, iliacus hematoma resulting from trauma, or complete palsy of the nerve [5, 19-22]. Although it has been previously stated that operative decompression is indicated in cases of large iliacus hematomas, parameters defining hematoma size have not been reported. Surgical exploration and hematoma evacuation carry a risk of immediate neurovascular injury, potentially leading to further bleeding, while the major surgery required to expose these deep structures also has a significant impact on rehabilitation [22]. Decompression should be considered in the presence of progressing signs and symptoms. If non-operative management is chosen, serial neurological examinations and hematological parameters reflecting ongoing blood loss must remain stable [9]. Non-operative treatment was elected in our case as the patient the hematoma appeared to be encapsulated, and thus, hardly amendable for percutaneous drainage due to its viscosity. The fact that no contrast enhancement after contrast administration was observed further contributed to our belief that there was no ongoing bleeding. The patient present at the 2-month follow-up with progressive recovery of muscle trophism and weight-bearing capacity, showing a good response to the conservative treatment. There was a significant reduction in the size of the hematoma at 6 months with complete resolution of the femoral nerve paralysis at 1 year, although variable lengths of recovery have been reported in the literature.
Femoral neuropathy due to spontaneous pelvic hematoma, though rare, poses significant diagnostic and therapeutic challenges. This condition often presents subtly and non-specifically, leading to delays in diagnosis. Typical manifestations include hip or groin pain, hip flexion contracture, and femoral nerve paresthesias. The case presented highlights an adolescent patient with a spontaneous iliacus muscle hematoma without a history of trauma or other apparent causes, managed successfully with conservative treatment. Key considerations for managing such cases include a thorough clinical assessment, imaging studies to confirm the diagnosis, and careful monitoring. Regular follow-up is crucial to ensure the resolution of the hematoma and recovery of nerve function. Early diagnosis and appropriate management are essential to prevent long-term complications and to ensure optimal patient outcomes.
This case report of femoral neuropathy secondary to a spontaneous iliacus muscle hematoma underscores the necessity for heightened clinical awareness and prompt diagnosis in patients presenting with non-specific symptoms such as thigh muscle atrophy and decreased limb strength, especially in the absence of trauma or anticoagulation therapy. The successful conservative management and full recovery observed in this adolescent patient illustrate the potential for non-surgical intervention in similar cases. This report contributes valuable insights into the rare presentation of spontaneous hematomas, emphasizing their consideration in differential diagnoses and highlighting the importance of thorough clinical and imaging assessments. The findings are pertinent for orthopedic and broader medical communities, offering guidance for managing atypical presentations of femoral neuropathy and enhancing overall patient care strategies.
References
- 1.Galzio R, Lucantoni D, Zenobii M, Cristuib-Grizzi L, Gadaleta A, Caffagni E. Femoral neuropathy caused by iliacus hematoma. Surg Neurol 1983;20:254-7. [Google Scholar]
- 2.Seijo-Martinez M, Castro del Rio M, Fontoira E, Fontoira M. Acute femoral neuropathy secondary to an iliacus muscle hematoma. J Neurol Sci 2003;209:119-22. [Google Scholar]
- 3.Crawford AM, Guild TT, Striano BM, Von Keudell AG. Spontaneous iliacus haematoma with femoral nerve palsy: An appeal to involve surgical teams early. BMJ Case Rep 2021;14:e239024. [Google Scholar]
- 4.Pirouzmand F, Midha R. Subacute femoral compressive neuropathy from iliacus compartment hematoma. Can J Neurol Sci 2001;28:155-8. [Google Scholar]
- 5.Goodfellow J, Fearn CB, Matthews JM. Iliacus haematoma. A common complication of haemophilia. J Bone Joint Surg Br 1967;49:748-56. [Google Scholar]
- 6.Busis NA. Femoral and obturator neuropathies. Neurol Clin 1999;17:633-53, vii. [Google Scholar]
- 7.Walsh C, Walsh A. Postoperative femoral neuropathy. Surg Gynecol Obstet 1992;174:255-63. [Google Scholar]
- 8.Kofler M, Kronenberg MF. Bilateral femoral neuropathy during pregnancy. Muscle Nerve 1998;21:1106. [Google Scholar]
- 9.Sanders SM, Schachter AK, Schweitzer M, Klein GR. Iliacus muscle rupture with associated femoral nerve palsy after abdominal extension exercises: A case report. Am J Sports Med 2006;34:837-9. [Google Scholar]
- 10.Wallace M, Kruse R, Eutsler EP, Averill LW. MRI findings of post-traumatic subperiosteal hematoma of the iliac bone with resultant femoral nerve palsy in an adolescent boy. Pediatr Radiol 2016;46:1350-3. [Google Scholar]
- 11.Guillin R, Moser T, Koob M, Khoury V, Chapuis M, Ropars M, et al. Subperiosteal hematoma of the iliac bone: Imaging features of acute and chronic stages with emphasis on pathophysiology. Skeletal Radiol 2012;41:667-75. [Google Scholar]
- 12.Choi HJ, Lee CC, Lim TH, Singer AJ. Traumatic subperiosteal pseudoaneurysm: Rare cause of subperiosteal hematoma. Am J Emerg Med 2009;27:1172.e5-7. [Google Scholar]
- 13.Weiss JM, Tolo V. Femoral nerve palsy following iliacus hematoma. Orthopedics 2008;31:178. [Google Scholar]
- 14.Poplausky MR, Durrani H, Rozenblit G, Maddineni S, Crea G, Goldberg B, et al. Traumatic subperiosteal pseudoaneurysm: A case report. J Trauma 2004;57:1115-8. [Google Scholar]
- 15.Yumoto T, Joko R, Yamakawa Y, Yamada T, Naito H, Nakao A. Subperiosteal hematoma of the iliac bone: An unusual cause of acute hip pain after a fall. Am J Case Rep 2018;19:1083-6. [Google Scholar]
- 16.Hammouche S, Mohammed I, Maheswaran T, Douds A. A rare clinical presentation of a malignant fibrous histiocytoma within the iliopsoas muscle. Ann R Coll Surg Engl 2010;92:W18-20. [Google Scholar]
- 17.Kontogeorgakos VA, Martinez S, Dodd L, Brigman BE. Extremity soft tissue sarcomas presented as hematomas. Arch Orthop Trauma Surg 2010;130:1209-14. [Google Scholar]
- 18.Murray IR, Perks FJ, Beggs I, Moran M. Femoral nerve palsy secondary to traumatic iliacus haematoma--a young athlete’s injury. BMJ Case Rep 2010;2010:bcr0520103045. [Google Scholar]
- 19.Tamai K, Kuramochi T, Sakai H, Iwami N, Saotome K. Complete paralysis of the quadriceps muscle caused by traumatic iliacus hematoma: A case report. J Orthop Sci 2002;7:713-6. [Google Scholar]
- 20.Sasson Z, Mangat I, Peckham KA. Spontaneous iliopsoas hematoma in patients with unstable coronary syndromes receiving intravenous heparin in therapeutic doses. Can J Cardiol 1996;12:490-4. [Google Scholar]
- 21.Kumar S, Anantham J, Wan Z. Posttraumatic hematoma of iliacus muscle with paralysis of the femoral nerve. J Orthop Trauma 1992;6:110-2. [Google Scholar]
- 22.Takami H, Takahashi S, Ando M. Traumatic rupture of iliacus muscle with femoral nerve paralysis. J Trauma 1983;23:253-4. [Google Scholar]