Irrespective of fracture level, suprapatellar nailing provides comparable outcomes in terms of healing, alignment, and extremity functional score.
Dr. Sanket Tanpure, Department of Orthopaedics, Thergaon Hospital, Thergaon, Pune, Maharashtra, India. E-mail: sankettanpure55@gmail.com
Introduction: A frequent bone fracture in falls and auto accidents is the tibial fracture. This study is prospective observational study primary aim to assess the healing duration, alignment, lower extremity functional score, and complications associated with suprapatellar (SP) tibial intramedullary nailing (IMN) for proximal, shaft, and distal tibial fractures.
Materials and Methods: Fifty-two patients (44 men and 8 women; mean age 46.9 years; range, 18–75 years) receiving semi-extended treatment using the SP method were included in the research. A solitary surgeon conducted SP IMN operations. Patients’ genders, ages, limb sides, fracture types, and classifications were noted following a minimum of a 12-month follow-up. Analysis was done on non-union, angulation, healing duration, and fracture reduction accuracy. Clinical measures were performed using the lower extremity functional score scale.
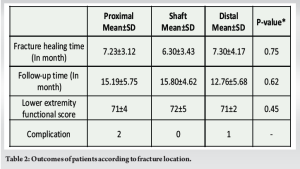
Results: In the tibia, 24 fractures occurred in the proximal third, 12 in the middle third, and 16 in the distal third. The average healing period was 7.34 months, with a range of 4–14 months. There was no statistically significant difference in healing times between the sites of the fractures (P = 0.75). There were no statistically significant variations in follow-up periods with respect to fracture locations (P = 0.62). The mean follow-up length was 15.76 months (range, 12–28 months). There was no statistically significant difference in lower extremity functional scores across the fracture site groups (P = 0.33).
Conclusion: Irrespective of fracture level, the SP IM tibia nailing has comparable functional score, a lower incidence of malalignment, shorter recovery periods, and less need for open reduction for any type of extra Articular tibia shaft fracture.
Keywords: Tibial fracture, suprapatellar nailing, lower extremity functional scoring scale.
A tibial fracture is among the most frequently occurring fractures of long bones in humans [1]. The majority of tibial fractures result from both low- and high-energy trauma. It is standard procedure to treat tibial fractures surgically with intramedullary nailing (IMN) [1,2]. One biomechanical load-sharing technology that may be advantageous is IMN, which allows for the early recovery and weight bearing [1,3]. Other significant advantages of IMN include less soft-tissue damage and maintenance of the extra-osseous blood supply [3]. Even with the minimally invasive plate osteosynthesis approach, concomitant soft-tissue problems are still inevitable, even though plate fixation can provide greater alignment control than an IMN [4]. The minimally invasive technique of IMN fixation does not impact soft-tissue injury. However, the traditional infrapatellar approach necessitates the knee to be in a flexed position throughout the nailing process, from creating the entry point to reaming and inserting the implant, making it difficult to maintain alignment and securely fix the nail in the wide canal of the distal tibial fragment [5]. Orthopedic surgeons have recently come to embrace SP IMNs more generally due to their benefits, which include easier control over fracture reduction and the ability to facilitate fluoroscopic pictures in the semi-extended position. Orthopedic trauma surgeons have recently focused on contrasting the SP and infrapatellar tibial nail insertion methods. Achieving the correct starting point and trajectory for infrapatellar nailing (IPTN) procedures necessitates hyperflexion of the knee, as explained. The pull of the extensor mechanism on the proximal segment can lead to a procurvatum deformity. Gradual flexion is required to guide a guidewire along the axis of the medullary canal and clear the patella. However, a posteriorly oriented guidewire may worsen the procurvatum deformity during nail insertion. In addition, fluoroscopic imaging is complicated by the need to significantly tilt the C-arm in line with the flexed knee. Surgeons must elevate themselves on step stools or raise their arms above their shoulders to ream in a superior to inferior direction. Given these challenges, there is a clear advantage to being able to insert tibial nails with the leg partially extended. Techniques such as Poller screws, devised by Krettek et al. [6], were developed to address these well-known issues when performing an infrapatellar nail. Even though there were methods for effectively implanting an infrapatellar tibial nail in cases of challenging proximal metaphyseal tibial fractures, novel approaches were developed to address these fracture patterns. A percutaneous lateral SP approach was carried out using a 1.5-cm transverse skin incision at the patella’s superolateral corner, as described by Morandi et al. [7]. Jakma et al. [8] used a 1–2 cm incision made exactly above the patella and in line with the tibial shaft. They employed unreamed nails, and the patellofemoral (PF) cartilage was damaged as shown by arthroscopy both before and after the nailing. In cadaveric studies, injuries to the intermeniscal ligament and medial meniscus with a SP entry have been noted [9]. Thus, to assess the effectiveness of the SP techniques in terms of radiological and functional outcomes when treating tibia fractures with IMN, we carried out this study.
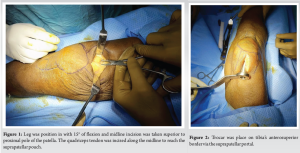
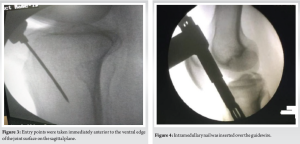
At the Tertiary Care Hospital in Bandra, Mumbai, 52 tibial shaft fractures were treated with tibial IMN between July 2019 and December 2020. The vast majority of tibial fractures were treated with a semi-extended technique, with the exception of grade IV arthrosis in the immovable PF joint (PFJ). Surgeons working alone performed all of the SP tibial IMN procedures. In this nonrandomized retrospective analysis, 52 patients (44 men and 8 women; mean age 47.2 years; range, 18–75 years) getting semi-extended care through the SP route were included in the study. For every patient, information on gender, age, limb side, and fracture classification was noted. The AO system was utilized for the classification of fractures. Written informed consent was given by each patient. Within 48 h of arriving at the emergency hospital, all fractures were treated by SP route tibial IMN. Initially, the patients received spinal anesthesia. Before the procedure, a pneumatic tourniquet was inflated. Next, the leg was prepared in a semi-extended posture with 15° of flexion. An SP midline incision was made 3 cm from the superior to proximal pole of the patella. The quadriceps tendon was incised along the midline to reach the SP pouch (Fig. 1). To preserve the PFJ, a trocar was implanted through the SP portal into the tibia’s anterosuperior border (Fig. 2). By passing a K-wire through the trocar under fluoroscopic guidance, the starting position of the nail was ascertained. In line with the McConnell et al. approach [10], the starting points were determined to be immediately anterior to the ventral edge of the joint surface on the sagittal plane (Fig. 3) and medial to lateral intercondylar tubercle in the coronal plane. A biplanar fluoroscopy system was used to verify the K-wire’s location. During the procedure, the tibial fracture was kept to a minimum and reduction maintenance was accomplished in the semi-extended position. The intramedullary canal was prepped for nail insertion by inserting the guide wire into it following proximal reaming. Next, the intramedullary canal was used to insert the nail (Fig. 4).
Distal locking and proximal locking screws were done under fluoroscopic guidance with jig (Fig. 5). Final position of implant was examined by fluoroscopic images (Fig. 6). Following surgery, patients were encouraged to gradually bear more weight. Range of motion in the knees and ankles was supported. Furthermore, physical therapy helped to progressively strengthen the quadriceps. Angulation, PF arthritis, fracture healing, and accuracy of fracture reduction were measured on X-rays. Lower extremity functional scale was used to measure functional outcome. Patients provided those measurements during the most recent follow-up check-up. Non-union, comorbidities, and fracture healing times were observed.

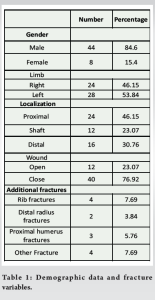
For male patients, the range of age was 18–75 years (47 years ± 7 years), and for female patients, it was 18–68 years (45 years ± 6 years). The mean age of the male and female patients was 48.6 and 45 years, respectively. Table 1 displays fractured limb side, open fracture, as well as other fractures. Fractures were categorized based on the AO system. The proximal third of the tibia had 24 fractures, the middle third had 12, and the distal third had 16. Table 1 displays fracture parameters and patient demographics. With one proximal fracture exhibiting a 4° valgus in the coronal plane, all patients achieved fracture reduction in anatomic lines. Within a range of 4–14 months, the mean fracture healing time was 7.34 months. A statistically insignificant difference (P = 0.75) was found in the fracture healing time between fracture locations. 15.76 months (range: 12–28) was the mean follow-up period. Nail dynamization was used to treat a patient who had non-union after 5 months. Implant exchange or grafting was not necessary for any of the patients. One patient experienced mild hemarthrosis, which was handled conservatively. Two individuals had superficial infections that were identified and treated with debridement and antibiotic therapy. In the knee joints, heterotrophic ossification did not take place (Tables 1 and 2).
A good results for shaft fractures have been documented with tibial IMN therapy [11,12]. While shaft fractures have shown encouraging outcomes, such as anatomic reduction, union rates, and enhanced mobility, problematic results have been described in proximal and distal tibial fractures [11,12]. Previous studies have effectively used SP approach in semi-extended position for nailing to resolve malalignment [11,12,13]. However, there are disagreements on the intensive application and SP technique for PF injury. For the great majority of patients in this study, SP tibial IMN resulted in good union rates with anatomic reduction [14]. Proximal, shaft, and distal fractures all showed comparable results in terms of fracture healing. In addition, distal fracture reduction was accomplished effectively. Similarly, favorable outcomes in distal 1/3 fractures by SP IMN were described by Avilucea et al. [5]. The semi-extended method has better alignment and a more anatomical starting point [13]. Our investigation validated the new research [15]. By positioning the patient and injured leg in a semi-extended posture, the fracture can be reduced and retained throughout the nailing process more easily. This is a key benefits. Stretching out the leg on the table also makes it easier to position the C-arm and set blocking screws, saving you from having to rearrange everything. Experience has shown that using this nailing approach decreases the incidence of compartment syndrome, since it exposes the soft tissue to significantly less intraoperative harm than conventional placement. The technique also has the benefit of requiring less assistance and having a shorter operating time. The potential of damaging the knee joint and, in the worst case scenario, infecting the joint are among the worries surrounding the usage of SP nail (SPN). Another concern is the possibility of penetration through a healthy knee joint. That being said, a large number of knee arthroscopies and retrograde femoral nailing are performed surgically these days without causing the same problems. In the first set of 25 patients by Tornetta and Collins [16], two patients had minor abrasions to their cartilage, and one had post-operative hemarthrosis. Afterward, Ryan et al. adjusted the methodology by nailing with the knee joint in 20–30 levels of flexion, playing out an average arthrotomy that main covered the upper part of the retinaculum and 1–2 cm into the quadriceps ligament, and changing the modest entry point of 3–5 cm from the center to the upper part of the patella [13]. Nowadays, a number of manufacturers have produced SPN equipment with protective sleeves to prevent intra-articular harm. Sanders et al. [12] used the SP technique to operate on 55 patients who had T2 (Stryker) and Trigen (Smith and Nephew) nails. An arthroscopy was done both before and after nailing in 13 out of 15 patients, and no alterations to the cartilage were observed. There was no relationship seen between the arthroscopic alterations, the magnetic resonance imaging (MRI) scans, and the clinical assessment 1 year following surgery. Of the 33 patients, one had grade II PF abnormalities, while the other had grade III changes. Is there any discernible anterior knee pain difference between individuals receiving IPTN and those receiving SPTN? This is another often studied subject. Research on anterior knee discomfort and kneeling pain has not yet revealed any distinctions between the two nailing methods [17]. After analyzing 12 randomized controlled trials in 2018, Chan et al. discovered that SPTN lowered sagittal alignment, visual analogue score, fluoroscopy time, and knee joint pain. In addition, they discovered improved range of mobility, Harris Hip score, Short-Form 36 Questionnaire, Lysholm knee score, and frequencies of “good” and “excellent” outcomes. The duration of hospital stay, coronal alignment, operating time, blood loss, and union time did not differ significantly across the groups [18]. Serbest et al. performed arthroscopy in their examination of 21 patients after each SPTN and found no association with anterior pain in the knee or functional limitations of the knee at a 1-year follow-up [19]. When compared to IPTN, several trials have shown improved knee pain. A brief retrospective assessment comparing 20 SPTN to 20 IPTN produced similar findings, showing lower radiation exposure, shorter operative times, better 3-month outcome scores for SPTN, and no differences in observed complications [20]. Our study shows insignificant difference in fracture healing time irrespective of fracture locations and lower extremity functional score which support recent literature. Furthermore, a significant issue with the SP technique is the possibility of PFJ chondral injury. Following SPN, the chondral surfaces have been evaluated in a variety of small investigations employing arthroscopy, MRI, and clinical evaluation [12,21]. In instances where follow-up duration and total subject count were modest, these investigations did not seem to produce any consistent results. In our study, we observed three complications as hemarthrosis and two patients with superficial infection. The main reason for the lower operation time of the SP group is the semi-extended knee position, which aids with entry recognition, fracture reduction, and fluoroscopic confirmation. The main benefit of the SP approach is that, unlike the IP strategy, which requires the affected limb to be hyperextended to at least 90°, the affixed limb can be readily retained in a semi-extended position with 20°–30° of knee flexion for the entire IMN procedure. The change in posture improves accessibility and makes it possible to obtain suitable anterior-posterior and lateral fluoroscopy images instantly. The ability to influence these aspects is crucial for the effectiveness of nail fixation, as it depends on achieving the proper entry and departure paths and the quality of fracture reduction. This is particularly true if the flexed knee position prevents access to the fluoroscopic coronal view.
According to this study, the SP method is renovative technique with greater lower extremity functional score, fewer malalignment rates, shorter surgical times, and less need for open reduction. The SP approach may be the most effective nailing method for treating tibial fractures.
SP nailing provides comparable outcomes in terms of healing, alignment, and extremity functional score irrespective of fracture level of shaft tibia. Authors recommend SP nailing approach over patellar tendon split approach irrespective of fracture level.
References
- 1.Fu B. Locked META intramedullary nailing fixation for tibial fractures via a suprapatellar approach. Indian J Orthop 2016;50:283-9. [Google Scholar | PubMed]
- 2.Zelle BA, Boni G. Safe surgical technique: Intramedullary nail fixation of tibial shaft fractures. Patient Saf Surg 2015;9:40. [Google Scholar | PubMed]
- 3.Franke J, Homeier A, Metz L, Wedel T, Alt V, Spät S, et al. Infrapatellar vs. suprapatellar approach to obtain an optimal insertion angle for intramedullary nailing of tibial fractures. Eur J Trauma Emerg Surg 2018;44:927-38. [Google Scholar | PubMed]
- 4.Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop 2008;32:697-703. [Google Scholar | PubMed]
- 5.Avilucea FR, Triantafllou K, Whiting PS, Perez EA, Mir HR. Suprapatellar intramedullary nail technique lowers rate of malalignment of distal tibia fractures. J Orthop Trauma 2016;30:557-60. [Google Scholar | PubMed]
- 6.Krettek C, Miclau T, Schandelmaier P, Stephan C, Möhlmann U, Tscherne H. The mechanical effect of blocking screws (“Poller screws”) in stabilizing tibia fractures with short proximal or distal fragments after insertion of small-diameter intramedullary nails. J Orthop Trauma 1999;13:550-3. [Google Scholar | PubMed]
- 7.Morandi M, Banka T, Gaiarsa GP, Guthrie ST, Khalil J, Hoegler J, et al. Intramedullary nailing of tibial fractures: Review of surgical techniques and description of a percutaneous lateral suprapatellar approach. Orthopedics 2010; 33:172-9. [Google Scholar | PubMed]
- 8.Jakma T, Reynders-Frederix P, Rajmohan R. Insertion of intramedullary nails from the suprapatellar pouch for proximal tibial shaft fractures. A technical note. Acta Orthop Belg 2011;77:834-7. [Google Scholar | PubMed]
- 9.Beltran MJ, Collinge CA, Patzkowski JC, Masini BD, Blease RE, Hsu JR, et al. Intra-articular risks of suprapatellar nailing. Am J Orthop 2012;12:546-50. [Google Scholar | PubMed]
- 10.McConnell T, Tornetta P 3rd, Tilzey J, Casey D. Tibial portal placement: The radiographic correlate of the anatomic safe zone. J Orthop Trauma 2001;15:207-9. [Google Scholar | PubMed]
- 11.Eastman J, Tseng S, Lo E, Li CS, Yoo B, Lee M. Retropatellar technique for intramedullary nailing of proximal tibia fractures: A cadaveric assessment. J Orthop Trauma 2010;24:672-6. [Google Scholar | PubMed]
- 12.Sanders RW, DiPasquale TG, Jordan CJ, Arrington JA, Sagi HC. Semiextended intramedullary nailing of the tibia using a suprapatellar approach: Radiographic results and clinical outcomes at a minimum of 12 months follow-up. J Orthop Trauma 2014;28:245-55. [Google Scholar | PubMed]
- 13.Ryan SP, Steen B, Tornetta P. Semi-extended nailing of metaphyseal tibia fractures: Alignment and incidence of postoperative knee pain. J Orthop Trauma 2014;28:263-9. [Google Scholar | PubMed]
- 14.Atik OŞ. Are all case reports worth publishing? Eklem Hastalik Cerrahisi 2016;27:61. [Google Scholar | PubMed]
- 15.Wang C, Chen E, Ye C, Pan Z. Suprapatellar versus infrapatellar approach for tibia intramedullary nailing: A meta-analysis. Int J Surg 2018;51:133-9. [Google Scholar | PubMed]
- 16.Tornetta P 3rd, Collins E. Semiextended position of intramedullary nailing of the proximal tibia. Clin Orthop Relat Res 1996;328:185-9. [Google Scholar | PubMed]
- 17.Isaac M, O’Toole RV, Udogwu U, Connelly D, Baker M, Lebrun CT, et al. Incidence of knee pain beyond 1 year: Suprapatellar versus infrapatellar approach for intramedullary nailing of the tibia. J Orthop Trauma 2019;33:9. [Google Scholar | PubMed]
- 18.Chen X, Xu HT, Zhang HJ, Chen J. Suprapatellar versus infrapatellar intramedullary nailing for treatment of tibial shaft fractures in adults. Medicine 2018;97:e11799. [Google Scholar | PubMed]
- 19.Serbest S, TiftiKci U, Coban M, Çirpar M, Daglar B. Knee pain and functional scores after intramedullary nailing of tibial shaft fractures using a suprapatellar approach. J Orthop Trauma 2019;33:37-41. [Google Scholar | PubMed]
- 20.Al-Azzawi M, Davenport D, Shah Z, Khakha R, Afsharpad A. Suprapatellar versus infrapatellar nailing for tibial shaft fractures: A comparison of surgical and clinical outcomes between two approaches. J Clin Orthop Trauma 2021;17:1-4. [Google Scholar | PubMed]
- 21.Chan DS, Serrano-Riera R, Griffing R, Steverson B, Infante A, Watson D, et al. Suprapatellar versus infrapatellar tibial nail insertion: A prospective randomized control pilot study. J Orthop Trauma 2016;30:130-4. [Google Scholar | PubMed]











