CT-based true external rotation (TER) evaluation in robotic total knee arthroplasty (TKA) provides considerable benefits, including improved implant placement precision. This method effectively aligns the femoral component with the individual anatomy, lowering the possibility of malrotation-related difficulties such as midflexion gap instability and patellar tracking abnormalities, resulting in better patient results and satisfaction.
Dr. Sawankumar Pawar, Department of Orthopedics, Fortis Hiranandani Hospitals, Vashi, Navi Mumbai, Maharashtra, India. E-mail: drsawanortho@gmail.com
Introduction: Midflexion gap (MFG) malalignment remains a challenge in total knee arthroplasty (TKA), often attributed to inaccurate femoral component positioning. Precise determination of true external rotation (TER) is crucial for optimal implant orientation and MFG reduction. This study aimed to evaluate the utility of computed tomography (CT)-based TER measurement in robotic knee replacements.
Materials and Methods: A retrospective analysis was conducted on data from 300 patients who underwent robotic TKA using a system that incorporates CT-derived bone models. TER was measured preoperatively on CT scans.
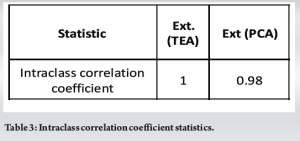
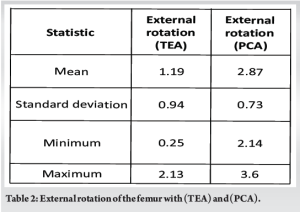
Results: The mean posterior condylar angle (PCA) (n = 300) between the transepicondylar axis (TEA) and the posterior condylar axis was 2.87 ± 0.73° (95% confidence interval [CI]) with a range of 2.14–3.6°. The external rotation between the anatomical and surgical TEA is 1.19 ± 0.94° (95% CI) with a range of 0.25–2.13°. Intraclass correlation coefficient for the angle is 1 (TEA) and 0.98 (PCA). This highlights potential discrepancies between traditional radiographic measurements and actual TER. Femoral component positioning aligned closer to the CT-based TER compared to standard methods. In addition, a significant reduction in MFG was observed in knees with TER-guided implant placement.
Conclusion: CT-based TER measurement provides a more accurate assessment of femoral rotation compared to conventional radiographs. This improved precision translates into optimal implant positioning and significantly reduces MFG malalignment in robotic knee replacements. Our findings suggest that incorporating CT-based TER into the workflow can enhance the accuracy and outcomes of robotic TKA.
Keywords: Computed tomography-based true external rotation, posterior condylar angle, posterior condylar axis, transepicondylar axis, total knee arthroplasty.
Knee osteoarthritis (OA) is a frequent condition causing significant morbidity in the aged population. Total knee arthroplasty (TKA) is a surgical procedure that has received widespread validation for its ability to restore a remarkable degree of function to the knee while also reducing knee OA discomfort. Around 20% of patients are still not satisfied with their TKA outcomes [1]. It is well known that a long-lasting implant and a good and effective outcome from TKA depend on the reliability of the rotational alignment and the technique used when placing the femoral component [2]. The stability and symmetry of the prosthetic joint’s flexion gap are determined by the femoral component’s adequate rotation throughout its range of flexion. Increased internal rotation of the femoral component is associated with patellar maltracking, which can cause patellar instability, conversely, excessive external rotation of the femoral component causes flexion instability, discomfort in the anterior knee, high revision rates, faster deterioration of the polyethylene insert, and impingement in posterior stabilized cam-post designs [3, 4]. This additionally plays an important in establishing native knee kinematics by enabling the knee to rotate in full range of motion while maintaining correct stability. Historically, as a substitute for the gap balancing approach, the posterior condylar angle (PCA) and the surgical transepicondylar axis (TEA) were used to ensure femoral component rotational alignment during measured resection procedures [5]. However, the reproducibility and accuracy of intraoperative TEA identification have been called into question in the literature, with conflicting reports. When a posterior condylar line rotates 3–4° internally with regard to its TEA, it indicates good condylar anatomy [6]. However, many studies have found variances in the connection of the PCA to the TEA, which might result in component malrotation in “25.5–72%” of patients [7, 8]. Over the past decade, many devices designed to aid in TKA, such as robots and dynamic tensioners, have entered the market. It is anticipated because their precision will reduce the incidence of malrotation in the femoral component, hence improving TKA results. Precise determination of true external rotation (TER) is crucial for optimal implant orientation and midflexion gap (MFG) malalignment reduction. This study aimed to assess the precision of native femoral TER in robotic knee replacements utilizing pre-operative computer tomography, employing either a TEA or PCA reference technique.
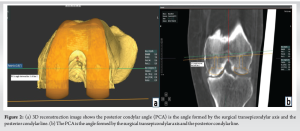
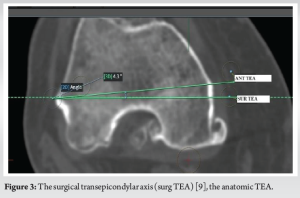
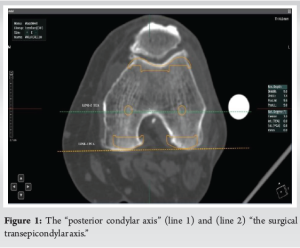
A retrospective analysis was conducted on data from 300 who underwent robotic TKA using a system that incorporates computed tomography (CT)-derived bone models. TEA and PCA were measured preoperatively on CT . Each patient underwent pre-operative CT scans of the ankle, knee, and hip and was instructed to stretch the knee joints as far as feasible. Jplanner software (Java, San Diego, CA) was used to segment all of the scans. A three-dimensional (3D) replica of the patient’s degenerative knee joint was generated by segmenting the femur and tibia bones. The study included patients who required a total knee replacement due to OA in their knees. The study excluded patients with trochlear dysplasia, arthritis with inflammation, and post-traumatic or septic arthritis. To best identify the median sulcus, two lines of reference were drawn across the axial portion of the femur’s distal end, where the femoral epicondyles intersect. The “posterior condylar axis” (line 1) is formed by the posterior areas of both the lateral and medial condyles, whereas (line 2) “the surgical transepicondylar axis” connects the most prominent region of the “lateral epicondyle” to the “medial epicondyle’s median sulcus” (Fig. 1). “The PCA is the angle formed by the surgical TEA and the posterior condylar line” (Fig. 2a and b, Fig. 3) depicts “the surgical TEA (surg TEA) [9], the anatomic TEA (anat TEA) [10], and the angle between them.”
Two observers (arthroplasty fellows with at least 2 years of work experience in orthopedics after receiving their postgraduate degree in orthopedics) independently evaluated the parameters, and the mean of their observations was determined to reduce “inter- and intra-observer variability.”
Statistics
The data were constructed and gathered using Microsoft Excel. The analysis was performed using “Epi info (Version 7.2; CDC, Atlanta).” Standard quantitative data were expressed using the mean and standard deviation. Descriptive statistics were used to assess the demographics and features of the groups. Standard deviations were included in the mean reports for rotational values. This two-tailed analysis had a significance threshold of 0.001. “Intra- and inter-observer variability were measured using an intra-class correlation.”
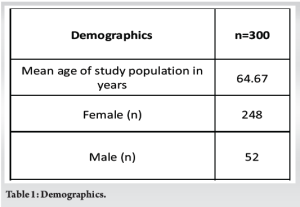
A total of 300 knees were assessed with stage 4 osteoarthritis with right to left side ratio 178:122 The female-to-male ratio for the study was 248:52. The study population had a mean age of 65.19 ± 7.57 years (Table 1). The mean PCA (n = 300) in between “the TEA and the posterior condylar axis” was 2.87 ± 0.73° (95% CI) with a range of 2.14–3.6°. The external rotation between anatomical and surgical TEA is 1.19 ± 0.94° (95% CI) with a range of 0.25–2.13° (Table 2). The intra-class correlation coefficient for the angle indicates a very high level of correlation between the two angles (Table 3).
Our research shows that the native femoral axis is externally rotated by 2.87° concerning PCA and 1.19° concerning TEA, with a difference between PCA and TEA of approximately 1.68°. Therefore, CT-based robotic TKA aids in pre-operative planning by assisting in the determination of implant sizes as well as implant rotation, taking into account the native anatomy of patients. This fact prevents outliers, unlike conventional TKA, which has a fixed 3° external rotation regardless of the patient’s rotational anatomy. Improper alignment constitutes one of the majority of prevalent challenges that result in revisions in knee arthroplasty surgery [11, 12]. While minor alignment erroneous may be tolerable [13, 14], true outliers within the alignment might cause issues and failures. Surgeons may now use real-time ligament stress data and 3D simulations to make precise adjustments during knee arthroplasty owing to the integration of robotic surgery and navigation. We call this functional alignment. Studies have shown that robotic-assisted TKA technology effectively restores the joint line and balances the gap while preserving almost normal knee joint motion. Ensuring accurate rotational alignment with the femoral component is essential for achieving favorable and promising outcomes from TKA [15, 16]. Excessive external rotation can lead to flexion and midflexion instability, stiffness, and post-operative pain, particularly pain in the anterior region of the knee. Conversely, excessive internal rotation can produce patellar maltracking and instability [3, 4]. In severe knee valgus deformity, the measured resection approach may be inaccurate when relying solely on one landmark or the axis to guide component rotation of the femur during TKA. In addition, malrotation may arise due to hypoplasia of the lateral femoral condyle [17, 18]. Determining a TEA may be difficult because it can be hard to pin down the most prominent point of the medial epicondyle’s sulcus [19]. Epicondylar axes are classified into two types: A surgical axis, which runs from the center of the medial epicondyle sulcus to the lateral epicondyle, and a clinical axis, which runs through the prominent portions of the medial and lateral epicondyles [20, 21]. Although the surgical axis proves more challenging to establish clinically, Kinzel et al. [22], and Berger et al. [23] believed it is of greater reliability. The anterior part of either the medial or lateral condyles of the femur may erode, making it challenging to define the Whiteside’s line in distorted knees [24, 25]. Therefore, it is crucial to consider all pertinent axes in TKA when calculating the femoral component rotational alignment. Based on research conducted in the West, a PCA is estimated to be approximately 3° [21, 23, 26]. The anteroposterior femur cut is positioned with 3° external rotations concerning the posterior condylar axis using a majority of customized jigs used in measured resections. Our research indicates that the PCA across the Indian knees is approximately 2.27 ± 0.73°. This implies that the femoral component malrotation in Indian knees may arise from the utilization of conventional femoral jigs with 3° of built-in external rotation concerning the posterior condylar axis during TKA. Our investigation found that femoral rotation concerning TEA and PCA resulted in consistent external rotation in functional alignment. According to our research, it is more accurate to use robotic pre-operative software to identify surgical TEA than to apply a fixed 3° external rotation to PCA to accomplish the proper rotation of the femoral component during TKA. Given these data, we advise against using a set PCA to calculate the rotation of the femoral component in TKA as this could lead to a high frequency of outliers. The following are the limitations of our investigation. Our radiological investigation was CT-based. With CT images, cartilage degeneration is not seen. Only a portion of Indian patients made up the study population. The long-term functional result was not assessed. Advantages of CT-based TER evaluation in TKA CT-based TER evaluation offers several advantages over traditional radiographic methods in TKA surgery, as evidenced by several studies.
Improved accuracy
Reduced discrepancies
CT-based TER directly measures the angle between the femoral condyles and the distal femur, bypassing potential errors in anatomical landmarks used in radiographic techniques. This reduces discrepancies between pre-operative planning and actual implant placement.
Surpasses limitations of radiographic techniques
Standard radiographic measurements, such as the TEA, can be unreliable due to anatomical variations and technical factors. CT-based TER avoids these limitations, providing a more accurate representation of true femoral rotation.
Enhanced implant positioning
Optimal component alignment
Precise TER measurement allows for precise implant positioning, leading to improved patellar tracking, ligament balance, and joint stability. This translates to better long-term functional outcomes and reduced revision rates.
Reduces MFG malalignment
MFG malalignment is a common complication in TKA, contributing to patellofemoral problems and instability. CT-based TER helps surgeons place the femoral component in a way that minimizes MFG, reducing the risk of these complications.
Additional benefits
Improved pre-operative planning
CT-based TER can be incorporated into pre-operative planning, allowing surgeons to choose the optimal implant size and orientation based on individual patient anatomy. This can streamline the surgical procedure and improve outcomes.
Potential for robotic integration
CT-based TER can be seamlessly integrated with robotic TKA systems, further enhancing accuracy and precision in implant placement. This provides surgeons with real-time feedback and guidance during the procedure.
Increased radiation exposure
Compared to standard radiographs, CT scans involve higher radiation exposure for the patient. Careful justification and optimization of CT protocols are crucial.
Additional costs
CT-based TER adds to the overall cost of the procedure, requiring access to CT scanners and specialized software for analysis.
Technical expertise needed
Interpreting CT-based TER measurements and incorporating them into surgical planning requires specific training and expertise.
Overall, the benefits of CT-based TER assessment in TKA surgery outweigh the limitations. Greater accuracy, better implant placement, and fewer complications lead to better patient outcomes and potentially lower health-care costs in the long term. As technology and knowledge in the field advance, CT-based TER is likely to become an increasingly valuable tool for surgeons performing TKA.
CT-based measurements of TER provide a more accurate assessment of femoral rotations using TEA or PCA than conventional radiographs. This improved accuracy means optimal implant placement and significantly reduces MFG errors in robotic knee replacements. Our results show that adding CT-based TER to the workflow can improve the accuracy and outcomes of robotic TKA.
In robotic TKA, using CT-based TER to align femoral components improves surgical accuracy and patient outcomes. This approach sets a new standard for long-lasting, patient-specific knee replacement outcomes by properly replicating native knee anatomy, minimizing implant malrotation, optimizing joint stability, and reducing problems such as MFG misalignment.
References
- 1.DeFrance MJ, Scuderi GR. Are 20% of patients actually dissatisfied following total knee arthroplasty? A systematic review of the literature. J Arthroplasty 2023;38:594-9. [Google Scholar]
- 2.Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019;393:655-63. [Google Scholar]
- 3.Ko DO, Lee S, Kim JH, Hwang IC, Jang SJ, Jung J. The influence of femoral internal rotation on patellar tracking in total knee arthroplasty using gap technique. Clin Orthop Surg 2021;13:352-7. [Google Scholar]
- 4.Kia M, Wright TM, Cross MB, Mayman DJ, Pearle AD, Sculco PK, et al. Femoral component external rotation affects knee biomechanics: A computational model of posterior-stabilized TKA. Clin Orthop Relat Res 2018;476:113-23. [Google Scholar]
- 5.Daines BK, Dennis DA. Gap balancing versus Measured resection technique in total knee arthroplasty. Clin Orthop Surg 2014;6:1-8. [Google Scholar]
- 6.Fitz DW, Johnson DJ, Hartwell MJ, Sullivan R, Keller TJ, Manning DW. Relationship of the posterior condylar line and the transepicondylar axis: A CT-based evaluation. J Knee Surg 2020;33:673-7. [Google Scholar]
- 7.Patel AR, Talati RK, Yaffe MA, McCoy BW, Stulberg SD. Femoral component rotation in total knee arthroplasty: An MRI-based evaluation of our options. J Arthroplasty 2014;29:1666-70. [Google Scholar]
- 8.Yau WP, Chiu KY, Tang WM. How precise is the determination of rotational alignment of the femoral prosthesis in total knee arthroplasty: An in vivo study. J Arthroplasty 2007;22:1042-8. [Google Scholar]
- 9.Asano T, Akagi M, Nakamura T. The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: In vivo analysis using a biplanar image-matching technique. J Arthroplasty 2005;20:1060-7. [Google Scholar]
- 10.Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res 1996;331:35-46. [Google Scholar]
- 11.Almaawi AM, Hutt JR, Masse V, Lavigne M, Vendittoli PA. The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthroplasty 2017;32:2133-40. [Google Scholar]
- 12.Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today--has anything changed after 10 years? J Arthroplasty 2014;29:1774-8. [Google Scholar]
- 13.Berger RA, Rubash HE. Rotational instability and malrotation after total knee arthroplasty. Orthop Clin North Am 2001;32:639-47, ix. [Google Scholar]
- 14.Hadi M, Barlow T, Ahmed I, Dunbar M, McCulloch P, Griffin D. Does malalignment affect revision rate in total knee replacements: A systematic review of the literature. Springerplus 2015;4:835. [Google Scholar]
- 15.Vaidya NV, Deshpande AN, Panjwani T, Patil R, Jaysingani T, Patil P. Robotic-assisted TKA leads to a better prosthesis alignment and a better joint line restoration as compared to conventional TKA: A prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 2022;30:621-6. [Google Scholar]
- 16.Zambianchi F, Bazzan G, Marcovigi A, Pavesi M, Illuminati A, Ensini A, et al. Joint line is restored in robotic-arm-assisted total knee arthroplasty performed with a tibia-based functional alignment. Arch Orthop Trauma Surg 2021;141:2175-84. [Google Scholar]
- 17.Alesi D, Meena A, Fratini S, Rinaldi VG, Cammisa E, Lullini G, et al. Total knee arthroplasty in valgus knee deformity: Is it still a challenge in 2021? Musculoskelet Surg 2022;106:1-8. [Google Scholar]
- 18.Mullaji AB, Sharma AK, Marawar SV, Kohli AF, Singh DP. Distal femoral rotational axes in Indian knees. J Orthop Surg (Hong Kong) 2009;17:166-9. [Google Scholar]
- 19.Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 2001;16:493-7. [Google Scholar]
- 20.Zhang G, Liu M, Fan S, Liu Z, Nie X, Qi X, et al. Comparison of the femoral condylar ellipse line and the surgical epicondylar axis: 3D measurement by MRI scans in healthy Chinese people. Orthop Surg 2023;15:1862-9. [Google Scholar]
- 21.Boisgard S, Moreau PE, Descamps S, Courtalhiac C, Silbert H, Moreel P, et al. Computed tomographic study of the posterior condylar angle in arthritic knees: Its use in the rotational positioning of the femoral implant of total knee prostheses. Surg Radiol Anat 2003;25:330-4. [Google Scholar]
- 22.Kinzel V, Ledger M, Shakespeare D. Can the epicondylar axis be defined accurately in total knee arthroplasty? Knee 2005;12:293-6. [Google Scholar]
- 23.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 1993;286:40-7. [Google Scholar]
- 24.Middleton FR, Palmer SH. How accurate is Whiteside’s line as a reference axis in total knee arthroplasty? Knee 2007;14:204-7. [Google Scholar]
- 25.Nagamine R, Miura H, Inoue Y, Urabe K, Matsuda S, Okamoto Y, et al. Reliability of the anteroposterior axis and the posterior condylar axis for determining rotational alignment of the femoral component in total knee arthroplasty. J Orthop Sci 1998;3:194-8. [Google Scholar]
- 26.Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL. Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arthroplasty 2000;15:354-9. [Google Scholar]