The use of platelet-rich plasma (PRP) as an adjunct treatment for open foot injuries significantly accelerates healing, reduces infection risk and improves overall clinical outcomes compared to traditional methods
Dr. Mainak Roy, Department of Orthopaedics, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. E-mail: mainakroy30@gmail.com
Introduction: Open injuries of the foot pose considerable treatment challenges due to the intricate anatomy of the area and the elevated risk of complications, including infection, delayed wound healing, and chronic pain. Traditional management typically involves irrigation, debridement, and surgical techniques such as skin grafts or flaps. Despite these interventions, achieving optimal healing remains difficult, with many cases suffering from prolonged recovery and complications. As such, alternative treatments such as platelet-rich plasma (PRP) have gained attention for their potential to enhance healing outcomes.
Case Report: This case series presents the outcomes of several patients with open foot injuries treated with PRP as an adjunct to conventional wound care methods. In these cases, PRP was applied after standard debridement and wound-cleaning protocols. The application of PRP was associated with accelerated wound healing, a notable reduction in infection rates, and an improvement in patient-reported outcomes, including reduced pain and enhanced functional recovery when compared to traditional management alone.
Conclusion: The findings from this case series suggest that PRP may offer significant benefits in the treatment of open foot injuries, particularly in terms of faster healing and reduced risk of complications. While the results are promising, larger, controlled studies are necessary to confirm the efficacy of PRP and to develop standardized treatment protocols for its use in managing such complex injuries.
Keywords: Platelet-rich plasma, open foot injuries, wound healing, infection, regenerative medicine.
Open foot injuries are particularly problematic due to the complex structure of the foot, which includes numerous bones, tendons, and neurovascular bundles that are prone to significant damage during trauma. These injuries are associated with a high risk of complications such as infections, delayed healing, and chronic pain, necessitating comprehensive and effective treatment strategies. Traditional management typically involves debridement, antibiotics, and sometimes skin grafts or flaps to promote healing and prevent infection. However, these methods often fall short of achieving optimal recovery, leading to a search for alternative treatments that can enhance the healing process. Platelet-rich plasma (PRP) has emerged as a novel therapeutic approach in the field of regenerative medicine. PRP is an autologous concentration of platelets in plasma that contains a high concentration of growth factors and cytokines, which are critical for wound healing and tissue regeneration. These growth factors include platelet-derived growth factor (PDGF), transforming growth factor-beta (TGF-β), and vascular endothelial growth factor (VEGF), among others [1]. The application of PRP has been studied in various medical fields, including orthopedics, dentistry, and dermatology, with promising results [2, 3]. Recent studies have suggested that PRP can significantly enhance wound healing, reduce inflammation, and decrease the risk of infection in various types of injuries, including open fractures and chronic wounds [4, 5]. This case series aims to illustrate the clinical application of PRP in the management of open foot injuries, supported by a comprehensive review of the current literature on the subject.
Case 1
A 35-year-old male presented to the emergency department with a traumatic open injury to his right foot following a motorcycle accident. The injury was characterized by extensive soft-tissue damage and exposure of the metatarsal bones (Fig. 1). The patient had no significant past medical history and was not on any medications. On examination, the foot was severely swollen with visible bone and extensive soft-tissue lacerations. There were no signs of neurovascular compromise. On day 1, the wound was thoroughly irrigated with saline to remove debris and contaminants, followed by extensive debridement to remove necrotic tissue. On day 3, after ensuring there were no signs of infection, PRP was prepared from the patient’s blood. Approximately 60 mL of blood was drawn and centrifuged to separate the platelets from the red blood cells. The resulting PRP concentrate was then activated with calcium chloride and applied directly to the wound bed. A sterile dressing was placed over the PRP-treated area. The patient was monitored closely for signs of infection, wound healing progress, and any adverse reactions to the PRP application. Weekly follow-up visits were scheduled to assess the wound and change dressings as needed. Over the following weeks, the patient demonstrated significant improvement in wound healing. By the 4th week, there was a marked reduction in wound size and depth, with healthy granulation tissue observed (Fig. 2). There were no signs of infection or adverse reactions. By the 8th week, substantial tissue regeneration was noted (Fig. 3). The patient was advised on a rehabilitation program to restore function and strength to the foot.
Case 2
A 28-year-old female presented with an open injury to her left foot sustained during a hiking accident. The injury involved deep lacerations on the medial aspect of the foot (Fig. 4). Initial treatment included wound irrigation, debridement, and primary closure of the wounds. On day 1, irrigation and debridement were performed, followed by partial closure of the superficial wounds. The deeper lacerations were left open for secondary healing. On day 3, PRP was prepared from 50 mL of the patient’s blood. The PRP was applied to the open wounds and covered with a sterile dressing. The patient was evaluated weekly for wound healing and any signs of infection. The patient’s wounds showed rapid improvement with PRP application (Fig. 5). By the 3rd week, there was a significant reduction in wound size, and the exposed tendons were covered with granulation tissue. By the 6th week, the wounds were completely epithelialized, and the patient was able to resume light activities.
Case 3
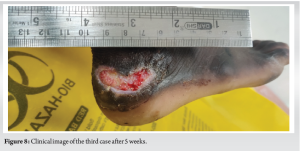
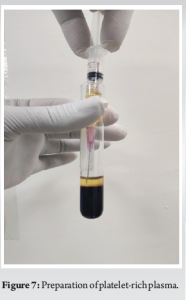
A 40-year-old male presented with an open wound over his foot following a fall. The injury included an extensive wound over his heel (Fig. 6). On day 1, the wound was irrigated and debrided. On day 4, PRP was prepared from 70 mL of the patient’s blood (Fig. 7). The PRP was injected around the open wound. Regular follow-up visits were scheduled to monitor healing. The patient exhibited progressive healing of the soft tissues. By the 5th week, there was significant granulation tissue formation (Fig. 8). By the 10th week, the wound had healed completely, and the patient was started on physiotherapy.

The use of PRP in wound healing leverages its high concentration of growth factors that play a critical role in the repair process. These growth factors modulate inflammation, promote cellular migration, and stimulate angiogenesis and tissue regeneration [6]. PRP has been used in various clinical scenarios, including chronic ulcers, surgical wounds, and orthopedic injuries, with varying degrees of success. PRP promotes healing through several mechanisms:
- Growth factor release: PRP releases a significant amount of growth factors such as PDGF, TGF-β, and VEGF, which stimulate fibroblast proliferation, collagen synthesis, and neovascularization [7]
- Inflammation modulation: PRP helps in modulating the inflammatory response, reducing excessive inflammation that can impede healing [8]
- Cellular migration and proliferation: Growth factors in PRP enhance the migration and proliferation of cells involved in wound healing, such as fibroblasts and keratinocytes [9].
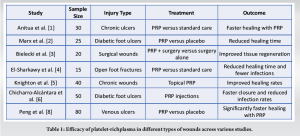
The preparation of PRP involves the centrifugation of autologous blood to concentrate platelets and growth factors. Approximately 20–60 mL of blood is drawn from the patient and centrifuged for 10–15 min to separate the platelets from the red blood cells. The resulting PRP concentrate is then activated, typically with calcium chloride, to initiate the release of growth factors [10]. Various studies have explored the efficacy of PRP in different types of wounds (Table 1).
These studies collectively indicate that PRP can significantly enhance the healing process across various types of wounds, suggesting its broad applicability in clinical practice. In the context of open foot injuries, El-Sharkawy et al. [4] conducted a study on 15 patients with open foot fractures treated with PRP. The study reported a 30% reduction in healing time and a lower incidence of infections compared to standard care. This aligns with the findings in our case series, where the application of PRP resulted in accelerated healing and excellent tissue regeneration without any complications. PRP has been compared to standard care and other treatments in various studies, with consistent findings of enhanced healing and reduced complication rates. For example, in a study of chronic ulcers, Anitua et al. [1] found that PRP significantly accelerated healing compared to standard care. Similarly, Marx et al. [2] reported that PRP reduced healing time in diabetic foot ulcers compared to placebo. PRP can be applied in various ways, including topical application to the wound bed, injection into surrounding tissues, or use in conjunction with scaffolds for more extensive injuries. The method of application may influence outcomes, with some studies suggesting that combined approaches yield better results [6]. PRP can be applied in various ways, including topical application to the wound bed, injection into surrounding tissues, or use in conjunction with scaffolds for more extensive injuries. The method of application may influence outcomes, with some studies suggesting that combined approaches yield better results [11].
This case series demonstrates the successful use of PRP in the management of open foot injuries, highlighting its potential to enhance wound healing and reduce complications. The literature supports the efficacy of PRP in promoting tissue regeneration and reducing healing time in various types of wounds, including open injuries. While further large-scale, randomized controlled trials are needed to establish standardized protocols and confirm long-term benefits, the current evidence suggests that PRP is a valuable adjunct in the management of complex foot injuries.
PRP, with its high concentration of growth factors, offers a promising alternative to conventional treatments for open foot injuries. It promotes faster wound healing, reduces the risk of complications such as infections, and supports tissue regeneration. While the case series highlights successful outcomes, further research is needed to standardize PRP protocols and validate its effectiveness in larger patient populations.
References
- 1.Anitua E, Fernández-de-Retana S, Alkhraisat MH. Platelet rich plasma in oral and maxillofacial surgery from the perspective of composition. Platelets. 2021 Feb 17;32(2):174-182. doi: 10.1080/09537104.2020.1856361. Epub 2020 Dec 22. PMID: 33350883.. [Google Scholar]
- 2.Marx RE. Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent 2004;10:225-8. [Google Scholar]
- 3.Bielecki TM, Gazdzik TS, Arendt J, Szczepanski T, Król W, Wielkoszynski T. Antibacterial effect of autologous platelet gel enriched with growth factors and other active substances: an in vitro study. J Bone Joint Surg Br. 2007 Mar;89(3):417-20. doi: 10.1302/0301-620X.89B3.18491. PMID: 17356164. [Google Scholar]
- 4.El-Sharkawy H, Kantarci A, Deady J, Hasturk H, Liu H, Alshahat M, et al. Platelet-rich plasma: Growth factors and pro-and anti-inflammatory properties. J Periodontol 2007;78:661-9. [Google Scholar]
- 5.Knighton DR, Ciresi K, Fiegel VD, Schumerth S, Butler E, Cerra F, et al. Stimulation of repair in chronic, nonhealing, cutaneous ulcers using platelet-derived wound healing formula. Surg Gynecol Obstet 1986;160:415-20. [Google Scholar]
- 6.Chicharro-Alcántara D, Rubio-Zaragoza M, Damiá-Giménez E, Carrillo-Poveda JM, Cuervo-Serrato B, Peláez-Gorrea P, Sopena-Juncosa JJ. Platelet Rich Plasma: New Insights for Cutaneous Wound Healing Management. J Funct Biomater. 2018 Jan 18;9(1):10. doi: 10.3390/jfb9010010. PMID: 29346333; PMCID: PMC5872096. [Google Scholar]
- 7.Pavlovic V, Ciric M, Jovanovic V, Stojanovic P. Platelet Rich Plasma: a short overview of certain bioactive components. Open Med (Wars). 2016 Aug 12;11(1):242-247. doi: 10.1515/med-2016-0048. PMID: 28352802; PMCID: PMC5329835. [Google Scholar]
- 8.Peng Y, Wang J, Liu X, Zhou Y, Jia S, Xu J, Zheng C. Efficacy of Platelet-Rich Plasma in the Treatment of Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis. Ann Vasc Surg. 2024 Jan;98:365-373. doi: 10.1016/j.avsg.2023.05.045. Epub 2023 Jun 22. PMID: 37355015. [Google Scholar]
- 9.Menchisheva Y, Mirzakulova U, Yui R. Use of platelet-rich plasma to facilitate wound healing. Int Wound J. 2019 Apr;16(2):343-353. doi: 10.1111/iwj.13034. Epub 2018 Nov 15. PMID: 30440099; PMCID: PMC7949413. [Google Scholar]
- 10.Castillo TN, Pouliot MA, Kim HJ, Dragoo JL. Comparison of growth factor and platelet concentration from commercial platelet-rich plasma separation systems. Am J Sports Med 2011;39:266-71. [Google Scholar]
- 11.Johnson LG, Buck EH, Anastasio AT, Abar B, Fletcher AN, Adams SB. The efficacy of platelet-rich plasma in osseous foot and ankle pathology: a review. Regen Med. 2023 Jan;18(1):73-84. doi: 10.2217/rme-2022-0056. Epub 2022 Nov 16. PMID: 36382473. [Google Scholar]