A comprehensive clinical assessment can help effectively plan surgery for patients with this rare condition by predicting anesthesia challenges. Total hip replacement can lead to a successful outcome in patients with ochronotic arthropathy. The use of capsulotomy can be considered for these patients. In addition, spinopelvic parameters must be taken into consideration in cases of fused spine to prevent impingement or dislocation.
Dr. Ankit Kumar Garg, Department of Orthopaedics, All India Institute of Medical Sciences, Raipur, Chattisgarh, India. E-mail: ankitkrgarg7@gmail.com
Introduction: Alkaptonuria is a rare genetic disorder characterized by the absence of the enzyme homogentisate 1,2 dioxygenase, which leads to the accumulation of homogentisic acid in connective tissues and blood, resulting in Ochronosis and osteoarthropathy.
Case Report: We present a case report of a 56-year-old male with ochronotic arthropathy and quadriceps tendon rupture who underwent a total hip replacement. The patient exhibited right hip pain, difficulty walking, and restricted movement at the hip and spine. Radiographic and magnetic resonance imaging findings confirmed significant arthritic changes in the right hip joint and a mid-substance tear in the quadriceps tendon. Intraoperatively, dark pigmentation was observed in the affected tissues, consistent with the diagnosis of Ochronosis. The literature review indicates that joint replacement surgery is the treatment of choice for ochronotic arthropathy, with patients experiencing good functional recovery. The prosthesis’s long-term survival rate is comparable to primary arthroplasty, and the optimal surgical approach regarding capsule preservation remains a topic of debate.
Conclusion: Joint replacement is a feasible treatment option for patients with ochronotic arthropathy. Understanding the spine-pelvic relations and other potential complications can help surgeons plan for better recovery and functional outcomes.
Keywords: Ochronotic arthropathy, alkaptonuria, total hip replacement.
Alkaptonuria is a rare genetic disorder with autosomal recessive inheritance which is caused by the absence of the enzyme homogentisate 1,2 dioxygenase, which is responsible for the breakdown of homogentisic acid, an intermediate in the tyrosine degradation pathway [1]. Homogentisate 1,2 dioxygenase is produced in the liver hepatocytes and kidney cells. The absence of this enzyme leads to the accumulation of homogentisic acid within the cells and blood, which then gets excreted through urine. However, due to significant accumulation and relatively lesser excretion, the homogentisic acid accumulates in connective tissues (such as menisci, tendons, intervertebral discs, articular surfaces, sclera, and pinnae), leading to dark pigmentation, and a condition known as Ochronosis [1]. Homogentisic aciduria, Ochronosis and osteoarthropathy characterize the disorder. It presents with multisystemic involvement, with the spine, hips, and knees commonly affected in the musculoskeletal system. The patient’s urine changes color on exposure to air or reducing agents [2]. The diagnosis is often suspected intraoperatively due to the characteristic black pigmentation of tissues and confirmed with a histological diagnosis. We present an interesting case report of a patient with ochronotic arthropathy and quadriceps tendon rupture.
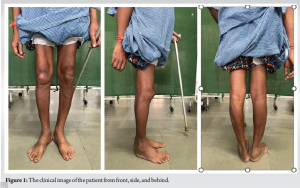
A 56-year-old male patient came in with a chief complaint of right hip pain for the past year and difficulty walking for the last 6 months. The pain worsened with movement and improved with rest. The patient had no other significant medical history. An antalgic gait with a Trendelenburg component was observed during the clinical examination. Gross wasting of the right gluteal and thigh region was noted, along with an extension lag over the right knee and a palpable defect over the quadriceps tendon area (Fig. 1). Movement at the hip and spine was restricted. No pigmentation or discoloration was found on the body, and the patient did not report any blackening of urine. Routine blood tests, including the rheumatological profile, came back within normal limits.
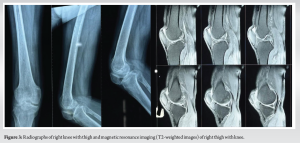
The radiography results revealed significant arthritic changes in the right hip joint, with reduced joint space and deformation of the femoral head, indicating osteonecrosis (Fig. 2). The lateral radiograph of the knee showed patella baja (Fig. 3), and the lumbar spine exhibited a calcified disk with reduced intervertebral space (Fig. 2). An magnetic resonance imaging of the right knee confirmed a mid-substance tear in the quadriceps tendon (Fig. 3).

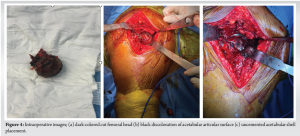
Under spinal anesthesia, the patient underwent surgery for a total hip replacement on the right side using a modified Hardinge approach. During the procedure, we observed dark pigmentation in the hip capsule, synovium, femur head, and acetabulum articular surface (Fig. 4). Samples were taken for histopathological examination, and we proceeded with total hip replacement involving anterior capsulotomy.
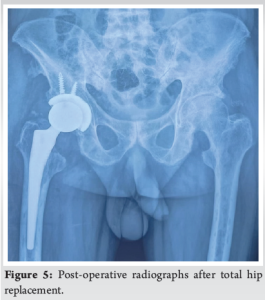
The patient recovered well with no complications. The patient was followed up at 6 weeks, 3 months, 6 months, 1 year, and 3 years. At the final follow-up, the implants are in good position (Fig. 5), and Harri’s hip score improved to 88 from 37 preoperatively. The patient can extend the knee with an extensor lag of 15° and, hence, is not willing to perform quadriceps reconstruction.
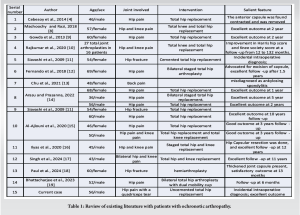
Alkaptonuria is a congenital disorder of metabolism that affects the body’s connective tissue and large weight-bearing joints. It causes arthritis in the large weight-bearing joints, making movement difficult and impacting daily activities. Most patients are diagnosed incidentally with spontaneous blackish discoloration of urine, or they may develop symptoms in the 3rd–5th decade of their life. Intraoperative diagnosis becomes likely with blackish discoloration of the bursae, capsule, synovium, and cartilage. The disease process significantly affects joints, and due to delayed presentation, joint replacement surgery becomes the treatment of choice [3]. Table (Table 1) provides a brief literature review comparing previous case reports and their key findings. The literature suggests that patients experience good functional recovery after joint replacement surgery.
The 12-year survival rate of the prosthesis is similar to that of primary arthroplasty, as reported by Spencer et al. [3]. There is no scientific evidence reported in the literature on the use of cemented versus uncemented implants in the case of ochronotic arthropathy. In their study, Cebesory et al. [4] and Fernando et al. recommended the removal of the anterior capsule due to marked thickening. Our study also found anterior capsular hypertrophy, which we subsequently removed. However, Pachore et al., in their study of 12 patients with a follow-up of 3–24 years, found good results with the preservation of the capsule during surgery [5]. A few studies have anticipated difficulty in spinal anesthesia due to changes in the spine and have preferred general anesthesia as the safer option [6,7]. In our case, no such difficulty was observed, probably due to the preservation of the space. In addition, spinopelvic parameters must be considered in the fused spine to prevent impingement or dislocation. In our case, an incidental diagnosis of alkaptonuria was made intraoperatively with exposure. Following this, an uncemented total hip arthroplasty was performed. Incidental sporadic cases of alkaptonuria are found among the Indian population. Proper pre-operative assessment with appropriate surgical steps done by a competent surgeon can be sufficient for adequate management and excellent outcomes.
The case emphasizes the effects of alkaptonuria and ochronotic arthropathy on the musculoskeletal system, especially on the hip joint. The patient’s successful recovery after total hip replacement highlights the significance of joint replacement surgery as a feasible treatment for this condition. Further research may be warranted to explore the long-term outcomes and potential differences in using cemented versus uncemented implants in cases of ochronotic arthropathy.
As a rare condition, a comprehensive clinical assessment can assist in effectively planning surgery for these patients by predicting anesthesia challenges, identifying any concurrent spine issues, and improving postoperative results. The use of capsulotomy can be considered in patients.
References
- 1.Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of Alkaptonuria. N Engl J Med 2002;347:2111-21. [Google Scholar | PubMed]
- 2.Peker E, Yonden Z, Sogut S. From darkening urine to early diagnosis of alkaptonuria. Indian J Dermatol Venereol Leprol 2008;74:700. [Google Scholar | PubMed]
- 3.Spencer J, Gibbons CL, Sharp R, Carr A, Athanasou N. Arthroplasty for ochronotic arthritis: No failure of 11 replacements in 3 patients followed 6-12 years. Acta Orthop Scand 2004;75:355-8. [Google Scholar | PubMed]
- 4.Cebesoy O, Isik M, Subasi M, Kaya A, Bilgin F, Kaya O. Total hip replacement for an ochronotic patient: A technical trick. Am J Case Rep 2014;15:27-30. [Google Scholar | PubMed]
- 5.Pachore JA, Shah VI, Upadhyay S, Shah K, Sheth A, Kshatriya A. Primary hip arthroplasty for the treatment of alkaptonuric hip arthritis: 3-to 24-year follow-ups. Arthroplasty 2019;1:8. [Google Scholar | PubMed]
- 6.Mäkelä A, Korkala O. Hip arthroplasty for alkaptonuric ochronosis. A case report. Acta Orthop Scand 1986;57:171-2. [Google Scholar | PubMed]
- 7.Pandey R, Kumar A, Garg R, Khanna P, Darlong V. Perioperative management of patient with alkaptonuria and associated multiple comorbidities. J Anaesthesiol Clin Pharmacol 2011;27:259-61. [Google Scholar | PubMed]
- 8.Mazoochy H, Razi M. Knee and Hip joint replacement surgery in a patient with ochronotic arthropathy: Surgical tips. Arch Bone Joint Surg 2018;6:577-81. [Google Scholar | PubMed]
- 9.Gowda N, Kumar MJ, Kumar AK. Black hip: A rare case treated by total hip replacement. Ann Saudi Med 2013;33:368-71. [Google Scholar | PubMed]
- 10.Rajkumar N., Soundarrajan D, Dhanasekararaja P, Rajasekaran S. Clinical and radiological outcomes of total joint arthroplasty in patients with ochronotic arthropathy. Eur J Orthop Surg Traumatol 2020;30:923-9. [Google Scholar | PubMed]
- 11.Siavashi B, Zehtab MJ, Pendar E. Ochronosis of hip joint; a case report. Cases J 2009;2:9337. [Google Scholar | PubMed]
- 12.Fernando OS, Supreeth N, David GD, Borja L, Ricardo L. An unusual case of bilateral ochronotic arthropathy of the hip successfully managed by a staged bilateral total hip replacement-an insight with a surgical note. J Orthop Case Rep 2018;8:11-4. [Google Scholar | PubMed]
- 13.Chu P, Cuellar MC, Bracken SJ, Tarrant TK. A mimic of ankylosing spondylitis, ochronosis: Case report and review of the literature. Curr Allergy Asthma Rep 2021;21:19. [Google Scholar | PubMed]
- 14.Arasu JA, Prasanna AA. Total hip arthroplasty for ochronosis: A report of three cases. J Orthop Case Rep 2022;12:23-7. [Google Scholar | PubMed]
- 15.Al-Ajlouni JM, Alisi MS, Yasin MS, Khanfar A, Hamdan M, Halaweh AA, et al. Long-term outcomes of the knee and hip arthroplasties in patients with alkaptonuria. Arthroplast Today 2020;6:689-93. [Google Scholar | PubMed]
- 16.Ilyas I, Kashif S, Algashiri MF, Rabbani SA, Aldakhil SS, Al-Mohrej OA. Long-term follow-up of bilateral hip and knee arthroplasty secondary to ochronotic arthropathy. Arthroplast Today 2020;6:214-9. [Google Scholar | PubMed]
- 17.Singh A, Thorat BS, Jaspal A. Arthroplasty in ochronotic arthropathy: 3 replacements in a single patient with a long-term follow-up of 11 Years. J Orthop Case Rep 2024;14:76-81. [Google Scholar | PubMed]
- 18.Paul AJ, John AS, Chandy VJ. Alkaptonuria with fracture neck of femur-a case report. J Orthop Case Rep 2024;14:73-7. [Google Scholar | PubMed]
- 19.Bhattacharjee S, Ahlawat A, Prasad A, Das RK. Total hip arthroplasty in ochronotic arthropathy: A case report. J Orthop Case Rep 2023;13:86-91. [Google Scholar | PubMed]









