A high index of suspicion of tuberculosis is imperative in endemic countries, especially in healthcare workers, irrespective of the immunity, vaccination status, and radiographic appearance. Early diagnosis and timely treatment give excellent functional outcomes.
Dr. Siddharth Gunay, Department of Orthopaedics, R.N. Cooper Hospital, Mumbai, Maharashtra, India. E-mail: siddharthgunay@gmail.com
Introduction: India accounts for more than 25% of the global cases of tuberculosis (TB). Skeletal TB accounts for approximately 15% of extra-pulmonary TB cases and up to 5% of all TB cases. Spine is the most common site for osteoarticular TB accounting for half of the total osteoarticular TB cases. TB osteomyelitis of flat bones such as the scapula is uncommon. The risk of TB among healthcare workers is significantly higher as compared to the general population. This is of particular concern, especially in endemic countries.
Case Report: A 26-year-old doctor presented with a 1-month history of dull-aching right shoulder pain without constitutional symptoms. The patient had tenderness over coracoid process on deep palpation with no other positive findings. Plain radiographs were unremarkable but magnetic resonance imaging revealed osteomyelitic changes in the coracoid process which was confirmed as TB on histopathology. The patient had excellent outcome after 18 months of anti-tuberculous therapy.
Conclusion: A high index of suspicion of TB is imperative in endemic countries, especially in healthcare workers, irrespective of the immunity, vaccination status, and radiographic appearance. Early diagnosis and timely treatment give excellent functional outcomes.
Keywords: Coracoid, tuberculosis, osteomyelitic, anti-tuberculous therapy, endemic.
India accounts for more than 25% of the global cases of tuberculosis (TB) [1]. Skeletal TB accounts for approximately 15% of extra-pulmonary TB cases and up to 5% of all TB cases [2]. Spine is the most common site for osteoarticular TB accounting for half of the total osteoarticular TB cases [2]. TB osteomyelitis of flat bones such as the scapula is uncommon. The risk of TB among healthcare workers is significantly higher as compared to the general population [3]. This is of particular concern, especially in endemic countries. Here, we present a case of isolated TB of the coracoid process in a 26-year-old male doctor who was successfully treated with anti-tuberculous therapy (ATT) and at 18 months’ follow-up had excellent functional outcomes. The patient was informed that the data concerning the case would be submitted for publication and he provided consent for the same.
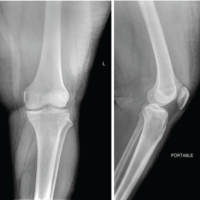
A 26-year-old male doctor presented with dull aching right shoulder pain for 1 month. He gave no history of trauma, fever, weight loss, or loss of appetite. Pain used to get aggravated on strenuous activities and relieved on rest. He consulted elsewhere where physical examination was unremarkable and the cause of pain was attributed to long working hours. He was given oral etoricoxib 90 mg twice a day for 2 weeks and started on physiotherapy. Physiotherapy was given in the form of strengthening exercises and interferential therapy which failed to alleviate his symptoms. The patient presented to us 1 month after physiotherapy was commenced. On examination, there was no obvious deformity or skin changes. Superficial palpation elicited no tenderness or local rise of temperature. However, the patient had mild tenderness on deep palpation over the coracoid process. He had no palpable lymphadenopathy. He had full range of movements which were painless. Measurements taken over the arm and forearm revealed no muscle wasting and neurovascular examination was insignificant. His American Shoulder and Elbow Surgeons (ASES) score was 75. Blood investigations revealed a hemoglobin of 15 g/dL and total leukocyte count of 7700/mm3. Differential leukocyte count was 65% neutrophils, 22% lymphocytes, 11% monocytes, 2% eosinophils, and 0 basophils. Erythrocyte sedimentation rate (ESR) was 12 mm/h (normal 0–15 mm/h) and C-reactive protein was 3.5 mg/dL (normal 0–5 mg/dL). Plain radiographs of the shoulder in anteroposterior and axillary views (Fig. 1) were unremarkable. We advised a magnetic resonance imaging (MRI) of the shoulder considering that the patient had a non-resolving pain for 2 months. MRI (Fig. 2) revealed signal changes in the coracoid process and adjoining soft tissue with features consistent with osteomyelitis. Mediastinal lymph nodes were found to be involved. High-resolution computed tomography of the chest was done which showed sub-centimeter-sized pre-tracheal, para-tracheal, hilar, pre-carinal, and bilateral axillary lymph nodes. Ultrasound-guided biopsy of the lesion was performed which was reported as epitheloid granuloma with central caseation necrosis. GeneXpert found the lesion sensitive to rifampicin.
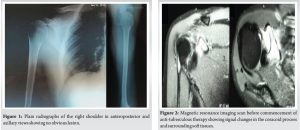
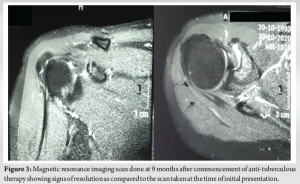
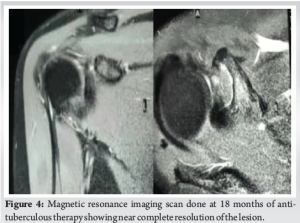
The patient was asked regarding his immunization status and contact history of TB. He was immunized till date as per the national immunization program and had no previous contact with a diagnosed TB patient. The patient was given ATT for 18 months. Initial phase included rifampicin, isoniazid, ethambutol, and pyrazinamide for 2 months and continuation phase included rifampicin and isoniazid for 16 months. This treatment was given after consulting the infectious disease specialist team. MRI was done at 9 (Fig. 3) and 18 months’ (Fig. 4) follow-up after commencement of ATT and at the 18th month, MRI showed near complete resolution of the lesion with altered marrow signals in the coracoid greatly reduced compared to the first scan. His ASES score at the final follow-up was 95/100.
India accounts for the highest number of TB cases in the world, pulmonary as well as extra-pulmonary. TB is a cause of severe morbidity and mortality and leads to a major burden on the healthcare infrastructure of the country [2]. Osteoarticular TB is especially associated with significant morbidity due to lack of timely diagnosis. This is attributed to the fact that many patients have an atypical presentation which makes suspicion of TB a dilemma [2]. It mainly occurs by hematogenous spread, with a small number of cases occurring as a result of lymphatic spread [2]. Isolated involvement of the bone in TB is uncommon as compared to concomitant pulmonary TB which is seen in one-third to half the patients [4-6]. When monoarticular, it usually affects the spine, hip, and knee with the upper extremity being fairly uncommon [5-7]. The shoulder region being affected by TB is <1% of all the cases of osteoarticular TB with scapula involvement seen in only a fraction of those cases [8]. Cases of scapular TB have been reported in the past which involve the body and angles. However, involvement of the coracoid process in TB is very rare [9,10]. The major predisposing factors for TB are malnutrition, diabetes mellitus, acquired immunodeficiency syndrome, poor sanitation, overcrowded housing conditions, repeated pregnancies, and lactation [2]. Prolonged corticosteroids and chemotherapy have also been identified as predisposing factors [11]. However, it must be noted that immunocompetent people are not immune from various forms of TB [3]. A meta-analysis published in 2017 concluded that the prevalence of latent TB infection (LTBI) in healthcare workers was 37% and the risk of LTBI in them was greater than the general population [12]. This correlates with our patient as he had no predisposing factors and plain radiographs were normal with mild symptoms suggesting a latent form of the disease due to intact immune system. The presentation of TB involving the scapular region is non-specific in the early stages with symptoms such as pain, stiffness, and decreased range of movements without constitutional symptoms [11,12]. It may be misdiagnosed as adhesive capsulitis of the shoulder further delaying the appropriate treatment [13]. At times, the affected site may be asymptomatic altogether [10]. This makes diagnosis quite difficult leading to a delay between the onset of the disease and diagnosis which may be as long as 5 months [11]. Local rise of temperature, fever, and redness of the underlying skin may be absent [2]. Due to a delay in diagnosis, many cases present with a discharging sinus and cold abscess at later stages which are an indicator of underlying bone destruction leading to a poor long-term outcome [10]. Plain radiographs and MRI aid in the diagnosis of osteoarticular TB. Radiographs are non-specific in these cases, with a wide spectrum of radiological appearance from osteolysis to ostesclerosis [15]. Cystic appearance is also noted in osteoarticular TB involving the scapula [8,16,17]. However, cystic lesions are also seen in pyogenic osteomyelitis, fungal osteomyelitis, osteosarcoma, metastasis, aneurysmal bone cysts, sarcoidosis, eosinophilic granuloma, and chordoma [18] None of these findings were seen in our patient who had a normal radiograph. MRI showed hyperintense lesion which was on the same lines as that reported by Chandane et al. [13] MRI helps to identify synovial thickening and periostitis much before it is apparent on plain radiographs and, thus, helps in increasing the suspicion of TB and an eventual early diagnosis [11]. MRI, although not diagnostic for TB, helps in assessing the osseous and soft-tissue involvement in osteoarticular TB along with underlying abscess and sinus tract formation and helps to take the most important decision between conservative and surgical treatment [2]. ESR is elevated in majority of the cases [2,8,10,15,18] and serial ESR measurement helps to assess the prognostic response to treatment. However, ESR was within normal limits in our case at the time of diagnosis and toward the end of treatment. Histopathology along with TB culture remains the gold standard methods for establishing the diagnosis of TB15] and this emphasizes the importance of correct tissue sample collection so that appropriate treatment can be started as early as possible. ATT remains the mainstay of treatment for osteoarticular TB. However, the optimal duration for the treatment of osteoarticular TB remains controversial with duration of >12 months having a relapse rate of 0.5% [19] Our patient received ATT for a duration of 18 months and he had excellent functional outcomes at the end of his treatment. This duration was in lines with the Index TB Guidelines of 2016 [20] . Osteoarticular TB is initially managed conservatively with ATT. Surgery is indicated in cases of abscess formation, neurovascular deficits, debilitating pain not responding to medications, joint deformity, and multiple drug resistance [2,19]. These factors were absent in our patient; hence, he could be managed with medications alone and we were able to achieve an excellent outcome.
This case report emphasizes the importance of a high degree of suspicion of TB in healthcare workers in endemic countries irrespective of their vaccination and current immunity status even when they present with mild symptoms and an apparently normal radiograph at uncommon sites. The key to successful outcome without long-term morbidity in these cases is timely diagnosis and early institution of ATT. We recommend similar case reports of uncommon sites with long-term follow-up periods to provide a more robust evidence.
This case highlights the need for maintaining a high index of suspicion for TB in healthcare workers from endemic regions, regardless of their vaccination history or perceived immunity, even if symptoms are mild and initial radiographs appear normal, especially in uncommon sites. Prompt diagnosis and early initiation of antitubercular therapy (ATT) are crucial to achieving positive outcomes and preventing long-term complications. We encourage further case reports on atypical presentations with extended follow-up to strengthen the evidence base.
References
- 1.Jain VK, Iyengar KP, Samy DA, Vaishya R. Tuberculosis in the era of COVID-19 in India. Diabetes Metab Syndr 2020;14:1439-43. [Google Scholar | PubMed]
- 2.Jagtap SA, Sonawane DV, Saraogi AA. Isolated tuberculosis of scapula in a young adult. Int J Mycobacteriol 2013;2:114-7. [Google Scholar | PubMed]
- 3.Uden L, Barber E, Ford N, Cooke GS. Risk of tuberculosis infection and disease for health care workers: An updated meta-analysis. Open Forum Infect Dis 2017;4:ofx137. [Google Scholar | PubMed]
- 4.Subasi M, Necmioglu S, Tuzuner T. The evaluation of our patients with bone and soft tissue tuberculosis. In: XVI. National Turkish Orthopaedic and Trauma Congress Book In: Ege R, editor. Ankara: Sargın Ofset; 1999. p. 1043-5. [Google Scholar | PubMed]
- 5.Watts HG, Lifeso RM. Current concepts review-tuberculosis of bones and joints. J Bone Joint Surg Am 1996;78:288-99. [Google Scholar | PubMed]
- 6.Nas K, Kemaloğlu MS, Çevik R, Ceviz A, Necmioğlu S, Bükte Y, et al. The results of rehabilitation on motor and functional improvement of the spinal tuberculosis. Joint Bone Spine 2004;71:312-6. [Google Scholar | PubMed]
- 7.Evanchick CC, Davis DE, Harrington TM. Tuberculosis of peripheral joints: An often missed diagnosis. J Rheumatol 1986;13:187-9. [Google Scholar | PubMed]
- 8.Jain D, Jain VK, Singh Y, Kumar S, Mittal D. Cystic tuberculosis of the scapula in a young boy: A case report and review of the literature. J Med Case Rep 2009;3:1. [Google Scholar | PubMed]
- 9.Jaumet E, Maisin J. A case of chondroma developed on tuberculosis of the coracoid apophysis of the scapula. J Belge Radiol 1961;44:359-61. [Google Scholar | PubMed]
- 10.Nataraj AR, Patro DK, Sreenivas T, Sharma D, Dhanapathi H. Multifocal skeletal tuberculosis presenting as periarthritis of shoulder joint: A case report. Eur Orthop Traumatol 2011;2:93-5. [Google Scholar | PubMed]
- 11.Kapukaya A, Subasi M, Bukte Y, Gur A, Tuzuner T, Kilnc N. Tuberculosis of the shoulder joint. Joint Bone Spine 2006;73:177-81. [Google Scholar | PubMed]
- 12.Chandane PG, Shah I, Mehta R, Jadhao N. Isolated scapular involvement: Uncommon presentation of childhood tuberculosis. Oxford Med Case Rep 2016;2016:omw039. [Google Scholar | PubMed]
- 13.Balaji G, Arockiaraj J, Roy AC, Ashok A. Isolated tubercular osteomyelitis of scapula-a report of two cases and review of literature. J Orthop Case Rep 2013;3:7. [Google Scholar | PubMed]
- 14.Mousa HL. Tuberculosis of bones and joints: Diagnostic approaches. Int Orthop 1998;22:245-6. [Google Scholar | PubMed]
- 15.Sharma BK, Singh VK, Nishant K, Das D. Scapular bone destruction: Do not forget to think of tuberculosis in endemic areas. Case Rep 2013;2013:bcr2013200051. [Google Scholar | PubMed]
- 16.Shannon FB, Moore M, Houkom JA, Waecker Jr NJ. Multifocal cystic tuberculosis of bone. Report of a case. J Bone Joint Surg Am 1990;72:1089-92. [Google Scholar | PubMed]
- 17.Greenhow TL, Weintrub PS. Scapular mass in an adolescent. Pediatr Infect Dis J 2004;23:84. [Google Scholar | PubMed]
- 18.Ghanshyam DE, Sharma S, Ilyas M. Isolated scapular tuberculosis: An uncommon presentation of skeletal tuberculosis. Eur Res J 2018;4:289-93. [Google Scholar | PubMed]
- 19.Darraj M. Delayed presentation of shoulder tuberculosis. Case Rep Infect Dis 2018;2018:8591075. [Google Scholar | PubMed]
- 20.Agarwal A. Paediatric osteoarticular tuberculosis: A review. J Clin Orthop Trauma 2020;11:202-7. [Google Scholar | PubMed]