Nerve compression syndromes can occur due to heterotopic ossification following minor trauma. A detailed understanding of heterotopic ossification and ulnar nerve compression necessary for management of these conditions is provided in this case report
Dr. Chiranjeevi Srinivasa Gowda, Department of Trauma and Orthopaedics, The Rotherham NHS Foundation Trust, S60 2UD, Rotherham, United Kingdom. E-mail: chiranjeevisrinivasa.gowda@nhs.net/gowda.chiranjeevi@gmail.com
Introduction: Heterotopic ossification (HO) is a known complication in the rehabilitation setting, involving the abnormal formation of bone in soft tissues. Ulnar nerve compression at the wrist due to HO is a rare occurrence, not widely reported in the literature. This case report highlights the unusual presentation of HO leading to ulnar nerve compression at the wrist, adding significant insight into the potential complications and management strategies for such cases.
Case Report: A 52-year-old woman of Caucasian ethnicity presented with a painful lump on the ulnar side of the volar aspect of her left wrist, 1 year after minor trauma. The patient initially forcefully dorsiflexed her wrist against a bus railing to prevent a fall, leading to a soft-tissue injury diagnosed through radiographs. Over the following months, she developed swelling, pain, and tingling in the ring and little fingers. Clinical examination revealed a firm 3 × 4 cm swelling associated with the flexor carpi ulnaris tendon and ulnar neurovascular bundle, indicated by increased pain on movement and a positive Tinel’s sign. Imaging showed calcific deposits and a lesion compressing the ulnar nerve. Surgical excision of the lesion was performed, and histopathology confirmed the diagnosis of HO. The patient experienced complete resolution of symptoms post-surgery, with no complications or recurrence observed at follow-up.
Conclusion: This case report discusses the importance of considering HO as a differential diagnosis for chronic ulnar-sided wrist pain with swelling post-trauma. The unusual presentation of ulnar nerve compression due to HO at the wrist enriches the orthopedic literature by highlighting a rare but significant complication.
Keywords: Heterotopic ossification, ulnar nerve compression, wrist trauma.
Heterotopic ossification (HO) is a common complication in rehabilitation, characterized by the formation of mature, lamellar bone in extra-skeletal soft tissue where bone usually does not exist [1]. The two main categories of HO are traumatic (fracture, arthroplasty, muscular trauma, joint dislocation, and burns) and neurogenic (stroke, spinal cord injury, traumatic brain injury, and brain tumors) [1]. The exact mechanism of HO in both categories is unknown, but trauma or a neurological event usually precedes HO formation [2]. HO typically presents with localized pain, tenderness, and swelling in early stages [3]. In later stages, swelling becomes more localized and firmer and may restrict motion if adjacent to a joint. It can also invade surrounding soft tissues and rarely present with neurovascular deficits. Ulnar nerve entrapment occurs most commonly in the cubital tunnel or the ulnar tunnel (Guyon’s canal) [4]. The exact location of compression determines the clinical presentation. This case report presents a 52-year-old woman with ulnar nerve compression at the wrist secondary to HO following minor trauma.
A 52-year-old woman presented with a painful lump on the ulnar side of the volar aspect of the left wrist, 1 year after sustaining trauma where she forcefully dorsiflexed her wrist against a bus railing to avoid falling. Initial radiographs diagnosed a soft-tissue injury without fractures which were managed conservatively. Over the next few months, she developed swelling and pain in her left wrist, aggravated by movement and associated with tingling and numbness in the ring and little fingers. There were no associated comorbidities, and she did not have history of HO anywhere else. On clinical examination, a 3 × 4 cm firm swelling was noted over the volar aspect of the ulnar side of the left wrist (Fig. 1). The swelling was associated with the flexor carpi ulnaris (FCU) tendon and the surrounding ulnar neurovascular bundle, demonstrated by increased pain on FCU movements and positive Tinel’s sign near the wrist, with reduced sensation in the ring and little fingers.

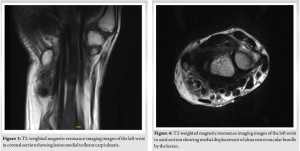
Radiographic evaluation showed calcific deposits over the ulnar head (Fig. 2). Magnetic resonance imaging (MRI) revealed a lesion pushing the ulnar neurovascular bundle medially and FCU laterally (Figs. 3 and 4). MRI findings suggested either HO or hydroxyapatite deposition disease (HADD).
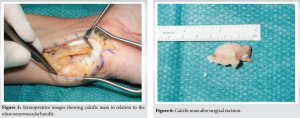
Surgical excision of the lesion was performed after obtaining informed consent, as the lesion was compressing the ulnar nerve. Surgery involved a longitudinal incision overlying FCU and the Pisiform bone, mobilizing FCU radially while protecting and retracting the ulnar nerve and artery medially. A 3 × 2 cm lump with calcific deposits was excised, including part of the pisotriquetral joint capsule (Figs. 5 and 6). Histopathology confirmed the diagnosis of HO.
The surgical outcome was good. Post-operative care included analgesia, wound care, and physiotherapy. The patient’s symptoms resolved completely by 6 months post-surgery, with no complications such as neurovascular injury, recurrence, or infection. She was discharged with no further follow-up after being advised on possible recurrence [3,5].
HO involves bone formation outside the skeletal system, typically in muscles and soft tissues. It can range from minor, clinically insignificant lesions to those causing significant morbidity. HO affects individuals of all ages, most commonly men. A history of trauma often triggers HO, although unrecognized microtrauma or repetitive mechanical stress can also be cause [6,7]. In this case report, minor trauma was the cause. The exact mechanism of HO remains unclear, but physical trauma or a triggering neurological incident and tissue expression of bone morphogenetic proteins are primary factors [2,3]. HO typically arises 3–12 weeks post-injury, sometimes up to 6 months [8]. Symptoms include joint pain, stiffness, swelling, and fever, with the highest risk 3–4 months post-injury, and in rare cases, tingling and numbness if associated with neurovascular infiltration as reported in our patient [9]. Investigations for HO include blood parameters and imaging. Blood tests such as alkaline phosphatase, erythrocyte sedimentation rate, C-reactive protein, and creatinine kinase can aid diagnosis but are not specific for HO [1,3]. Radiographs are highly specific but only detect late-stage HO, while triple-phase bone scans are most sensitive for the early HO [1]. Ultrasonography and MRI are useful if HO affects neurovascular structures. Computed tomography helps outline bone formation for surgery but has limited diagnostic use [9]. Treatment includes conservative and surgical options. Prophylaxis involves gentle range-of-motion exercises, non-steroidal anti-inflammatory drugs, and bisphosphonates [10,11]. Early passive range of motion exercises prevents joint ankylosis. Prophylactic measures are used as treatment in the early disease. External beam radiation is used after failure of conservative management in arthroplasty [12]. Surgical resection is the definitive treatment, typically done 12–18 months post-injury after mature bone formation [13]. Surgical resection is considered only if it resolves symptoms. Complications of HO include decreased function and mobility due to ankylosis, peripheral nerve entrapment, vascular compromise, lymphedema, and pressure ulcers [13]. Prognosis is generally good after surgery. Histopathology of HO shows hypercellular spindle cells and woven bone surrounded by trapped muscle and normal osteoblasts. The central zone of immature fibrous tissue surrounded by mature bone distinguishes HO from osteosarcoma [1]. Ulnar nerve compression occurs at the elbow (cubital tunnel) or wrist (Guyon’s canal). Symptoms depend on the compression site. The ulnar nerve originates from the brachial plexus, passes through the arcade of Struthers, then the cubital tunnel. In the forearm, it runs between the FCU and flexor digitorum profundus and enters Guyon’s canal, innervating these muscles and intrinsic hand muscles. It also relays sensory signals from the ulnar border of the ring and little fingers and the hypothenar region [4]. Ulnar nerve compression can be acute (trauma-related) or chronic (idiopathic, diabetes, leprosy, alcoholism, infiltrating mass like HO, HADD, and tumors). Presentation involves sensory and motor deficits in ulnar-innervated regions. Diagnosis includes clinical examination, nerve conduction studies, and electromyography. Treatment options include conservative management (physiotherapy and splinting) and surgery (nerve decompression, repair, transfer, and tendon transfer in advanced cases) [4,14,15]. In this case, additional evaluation of the ulnar nerve was not performed as clinical signs correlated with the anatomical location and HO diagnosis confirmed by biopsy. Additional tests such as nerve conduction studies and electromyography would increase treatment costs without providing additional information. The association of HO and nerve compression near calcifications is less common. HO has been reported to cause ulnar compression at the elbow but not at the wrist. A thorough understanding of HO, differential diagnoses, and the anatomy and pathophysiology of ulnar nerve disorders is recommended for similar cases.
HO should be considered among differentials for chronic ulnar-sided wrist pain with swelling following trauma. Understanding the disease pathology is necessary for optimum outcomes as early surgical resection can cause recurrence. The decision for surgical excision can be particularly difficult in the presence of nerve compression syndromes, warranting a patient-specific treatment approach.
The association of HO and nerve compression syndrome is not very common. While HO may not be the direct cause of nerve compression, it promotes compression. A detailed understanding of the disease and patient-specific problems is vital for favorable outcomes in treatment of nerve compression syndrome due to HO.
References
- 1.Shehab D, Elgazzar AH, David Collier B. Heterotopic Ossification. Available from: https://www.snm.org/education/ce_online.html [Last accessed on 2024 Sep 07]. [Google Scholar | PubMed]
- 2.Chen HC, Yang JY, Chuang SS, Huang CY, Yang SY. Heterotopic ossification in burns: Our experience and literature reviews. Burns 2009;35:857-62. [Google Scholar | PubMed]
- 3.Sun E, Hanyu-Deutmeyer AA. Heterotopic Ossification. StatPearls; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519029 [Last accessed on 2024 Sep 05]. [Google Scholar | PubMed]
- 4.Singh V, Trescot AM. Ulnar nerve entrapment. In: Peripheral Nerve Entrapments: Clinical Diagnosis and Management. 2023. p. 383-96. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555929 [Last accessed on 2024 Sep 05]. [Google Scholar | PubMed]
- 5.Meyers C, Lisiecki J, Miller S, Levin A, Fayad L, Ding C, et al. Heterotopic ossification: A comprehensive review. JBMR Plus 2019;3:e10172. [Google Scholar | PubMed]
- 6.Nuovo MA, Norman A, Chumas J, Ackerman LV. Myositis ossificans with atypical clinical, radiographic, or pathologic findings: A review of 23 cases. Skeletal Radiol 1992;21:87-101. [Google Scholar | PubMed]
- 7.Isse HM, Sereke SG, Vincent M, Zeridah M. Non‐traumatic myositis ossificans circumscripta in the anterior abdominal wall of a seven‐year‐old Ugandan child: A case report. Clin Case Rep 2022;10:e6145. [Google Scholar | PubMed]
- 8.Tao MJ, Probyn L, Poon M, Kreder H, Nousiainen M, Jenkinson R, et al. Potential discrepancy between plain films and CT scans in Brooker classification of heterotopic ossification. Br J Radiol 2017;90:20170263. [Google Scholar | PubMed]
- 9.Yoon BH, Park IK, Sung YB. Ankylosing neurogenic myositis ossificans of the hip: A case series and review of literature. Hip Pelvis 2018;30:86. [Google Scholar | PubMed]
- 10.Joice M, Vasileiadis GI, Amanatullah DF. Non-steroidal anti-inflammatory drugs for heterotopic ossification prophylaxis after total hip arthroplasty. Bone Joint J 2018;100B:915-22. [Google Scholar | PubMed]
- 11.Aubut JA, Mehta S, Cullen N, Teasell RW, Group E, Team SR. A comparison of heterotopic ossification treatment within the traumatic brain and spinal cord injured population: An evidence based systematic review. Neuro Rehabil 2011;28:151. [Google Scholar | PubMed]
- 12.Ruo Redda MG, De Colle C, Bianco L, Ruggieri A, Nassisi D, Rossi A, et al. Heterotopic ossifications: Role of radiotherapy as prophylactic treatment. Radiol Med 2018;123:463-8. [Google Scholar | PubMed]
- 13.Behery OA, Dai AZ, McLaurin TM. Posttraumatic heterotopic ossification of the hip. J Orthop Trauma 2018;32 Suppl 1:S18-9. [Google Scholar | PubMed]
- 14.Carballo Cuello CM, De Jesus O. Neurapraxia. StatPearls; 2024. Available from: https://pubmed.ncbi.nlm.nih.gov/32809336 [Last accessed on 2024 Sep 07]. [Google Scholar | PubMed]
- 15.Bhandari PS. Management of peripheral nerve injury. J Clin Orthop Trauma 2019;10:862. [Google Scholar | PubMed]








