Fractures in patients with fibrous dysplasia, particularly in the pediatric population, require careful consideration to preserve bone growth and prevent complications. Surgical interventions, such as osteotomy and internal fixation, can be effective in achieving good functional outcomes
Dr. Sushant Srivastava, Department of Orthopaedics, Mata Gujri Memorial Medical College and Lions Seva Kendra Hospital, Kishanganj, Bihar, India. E-mail: sushant391992@yahoo.co.in
Introduction: Fibrous dysplasia (FD) is a benign, non-heritable, intramedullary fibro-osseous lesion described by Lichtenstein in 1938. It is considered that a developmental failure occurs during remodeling of woven bone so that lamellar bone fails to form. The bone also fails to remodel in response to mechanical stress. It has a considerable risk of pathological fractures particularly in proximal femur in younger age group. These are challenging to treat, especially in younger population. Several treatment modalities have been proposed, each having its own pros and cons. Attention should be given in pediatric population in choosing technique and selection of implants to preserve growth of the limb and to prevent implant prominence and soft-tissue irritation.
Case Report: We are reporting a case of pathological proximal shaft of femur fracture secondary to FD, in an 14-year-old obese boy, managed with corrective osteotomy, 135° angle blade plate fixation and bone graft.
Conclusion: At subsequent follow-ups, he showed good consolidation at fracture site, stable implant, and an excellent functional outcome in terms of pain and range of motion, without any radiological sign of recurrence.
Keywords: Fibrous dysplasia, pediatric pathological fracture, proximal shaft fracture, corrective osteotomy, angle blade plate, bone graft.
Fibrous dysplasia (FD) is a non-heritable, benign, and fibro-osseous lesion that is commonly medullary monostotic (80%), or sometimes polyostotic (20%). Monostotic FD may be present at any age though it is most common in those aged below 30 years while polyostotic FD is seen much early and most commonly presents before puberty. There is equal sex distribution [1]. This was first described by Lichtenstein in 1938 and later further elucidated by Lichtenstein and Jaffe in 1942 [2]. It is considered that a developmental failure occurs during remodeling of woven so that mature lamellar bone fails to form. The bone also fails to remodel in response to mechanical stress (i.e., does not follow Wolff’s law). Due to loss of maturation, an unorganized mass of immature trabeculae is left enmeshed in dysplastic fibrous tissue [3]. Malignant transformation into osteosarcoma is a potential complication in 7% of cases with multiple bone involvement [4]. Pathological fractures, often without prior warning signs, can occur in 20–40% of cases [5, 6]. Surgical intervention is considered for severe pain, significant deformity, or impending/pathological fractures. Treatment options include removing the diseased bone (curettage) and filling the defect with bone grafts (cancellous bone, fibula bone, or donor bone) [7, 8]. The primary goal for Shepherd’s Crook deformity treatment is to correct the deformity, restore normal bone alignment, prevent recurrence, and ensure healing of the fracture and bone cut. This case report presents a case of pathological proximal shaft of femur fracture secondary to FD, in an 14-year-old obese boy, managed with corrective osteotomy, 135° angle blade plate fixation and bone graft.
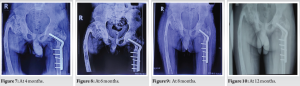
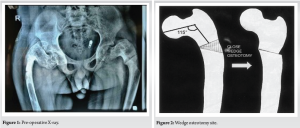
A 14-year-old male student presented to out-patient department of MGM medical college with pain left hip and thigh for 1 and 1/2 months. Initially, the pain was on and off but then persistent for the past 1 week. It was dull in character, non-radiating but aggravated with walking and relived with rest and analgesics. There was no history of fever and weight loss. He had history of fracture femur of the right side at age of 9 years which was treated surgically (open reduction and internal fixation with plating) at that time. His physical examination revealed deformity, abnormal mobility, tenderness, and crepitus felt upper left thigh with anterolateral convexity. There were no open wounds and the neurovascular state was completely intact. Straight leg test could not be performed; hip movements were painful and limited in all planes, especially in coronal plane. There was true shortening of 3 cm of left side. Distal neurovascular status was normal. Sensation and power were normal in both lower limbs. Spine was normal. Plain radiographs of pelvis with bilateral hip anteroposterior view were done (Fig. 1); it showed Shepherd’s Crook deformity of proximal femur of both sides. His alkaline phosphatase was 400 IU/L apart from that rest of the endocrinological test, serum calcium, and phosphorus came out to be normal. The patient was counseled, and consent taken for surgery and publication of his case report. Under general anesthesia, the patient was placed on traction table and as per aseptic setting, a lateral approach is used to make incision from tip of greater trochanter continuing distally to mid shaft of femur. Soft tissue was dissected to reveal proximal femur. The patient underwent lateral closed wedge osteotomy of approximately 20° for correction of the left proximal femur deformity (Fig. 2-4). Proximal and distal fragments were stabilized using 5 holed 135° angle blade plate. Corticocancellous iliac crest graft from ipsilateral side was harvested and placed. Limb length discrepancy was corrected. Wound was closed in layers and dressing applied. Postoperatively, institutional standard antibiotic along with injection paracetamol 1 g iv bd was given. On post-operative day 7, supervised physiotherapy (isometric exercises) was started in the hospital. On post-operative day, 14 stitches were removed. At the time of discharge injection teriparatide 20 mcg s/c once daily, oral sodium alendronate 70 mg tablet once every week was prescribed. Non-weight-bearing was advised for first 2 months, partial weight-bearing for another 1 month, and full weight-bearing deferred until radiological signs of union were observed, that is, around 3 months. The patient came for subsequent follow-up at – 1, 2, 4, 6, 8, and 12 months (Fig. 5-10). At 1-year follow-up, the osteotomy site and fracture site were united, and the patient was mobile without support. No recurrence or deformity was noted.

Shepherd’s Crook deformity may present at a different stage and in a different way thus warrants a “Customized” or “Tailored” approach to treat this deformity. The paramount importance however should be given to achieve union with simultaneous correction of the deformity irrespective of the approach being used. We used double angle blade plate fixation because the quality of bone was poor, and intramedullary nails were difficult to pass due to excessive bowing of the proximal femur [9]. Literature supports single stage fracture fixation and corrective surgery as it tends to decrease morbidity of the patient and helps in early rehabilitation [10]. Internal fixation aids in the early weight-bearing and should be considered wherever possible. Oral bisphosphonates have been used to treat FD and to inhibit osteoclastic remodulation of osteoid. We shared the outcome of our case study after a year of follow-up. Our patient had fully recovered, walking independently, and bearing weight without any assistance. There were no signs of the original issue returning or any deformity, and both the fracture and the surgical cut had healed completely. Nevertheless, we suggest continued monitoring of our patient to further validate the success of our surgical method.
Excellent functional and radiological outcome can be achieved in patients of FD presented with Shepherd’s Crook deformity and pathological fracture shaft of femur managed with corrective osteotomy, 135° angle blade plate fixation, and bone graft. To prevent recurrence of the deformity, the length of the plate must be adequate to span the lesion.
Our patient, a 14-year-old obese boy with Shepherd’s Crook deformity and a pathological fracture of the ipsilateral femur shaft, was treated with corrective osteotomy, 135° angle blade plate fixation, and bone grafting. Literature supports a single-stage approach to fracture fixation and corrective surgery, as it tends to reduce patient morbidity and facilitate early rehabilitation. An angle blade plate was used for fixation due to poor bone quality and the difficulty of inserting intramedullary nails caused by excessive bowing of the proximal femur.
References
- 1.Varshney MK. Essential Orthopedics Principles and Practice. Delhi: Jaypee Brothers; 2016. p. 228. [Google Scholar]
- 2.Nagda TV, Singh H, Kandoi M, Samant A, Patel BR. Two stage reconstruction for the Shepherd’s crook deformity in a case of polyostotic fibrous dysplasia. J Postgrad Med 1997;43:83. [Google Scholar]
- 3.Harris WH, Dudley HR Jr., Barry RJ. The natural history of fibrous dysplasia. An orthopaedic, pathological, and roentgenographic study. J Bone Joint Surg Am 1962;44:207-33. [Google Scholar]
- 4.Ruggieri P, Sim FH, Bond JR, Unni LK. Malignancies in fibrous dysplasia. Cancer 1994;73:1411-24. [Google Scholar]
- 5.Saglik Y, Atalar H, Yildiz Y, Badarir K, Erekul S. Management of fibrous dysplasia. A report on 36 cases. Acta Orthop Belg 2007;73:96-101. [Google Scholar]
- 6.Kushare IV, Colo D, Bakhshi H, Dormans JP. Fibrous dysplasia of the proximal femur: Surgical management options and outcomes. J Child Orthop 2014;8:505-11. [Google Scholar]
- 7.Stanton RP. Surgery for fibrous dysplasia. J Bone Miner Res 2006;21:105-9. [Google Scholar]
- 8.Wai EK, Davis AM, Griffin A, Bell RS, Wunder JS. Pathologic fractures of the proximal femur secondary to benign bone tumors. Clin Orthop 2001;393:279-86. [Google Scholar]
- 9.Stephenson RB, London M, Hankin F, Kaufer H. Fibrous dysplasia. An analysis of options for treatment. J Bone Joint Surg Am 1987;69:400-9. [Google Scholar]
- 10.Kandhari VK, Bava SS, Desai MM, Wade RN. Single stage treatment of non-union of transcervical neck femur fracture with shepherd crook deformity of proximal femur in a case of fibrous dysplasia using dynamic hip screw fixation. J Orthop Case Rep 2015;5:41-4. [Google Scholar]