Recurrent hip dislocations are rare in adults, residual instability after closed reduction may indicate ligamentous damage or acetabulum fractures. Early detection and concentric reduction are crucial for optimal results and minimizing complications.
Dr. Rohit Tyagi, Department of Orthopaedics, Mahatma Gandhi Medical College and Hospital, Jaipur, Rajasthan, India. Phone: +9773548662. E-mail rohittyagi9491@gmail.com
Introduction: Recurrent hip dislocations are quite uncommon, and only 2% of cases of all hip dislocations exhibit recurrence. Ligamentous laxity, joint capsule lesion, or structural hip abnormalities can all lead to such presentation. They are usually associated with acetabulum fractures and labrum injuries. To the best of our knowledge, there are no cases of adult recurrent posterior hip dislocation in the literature that we could find.
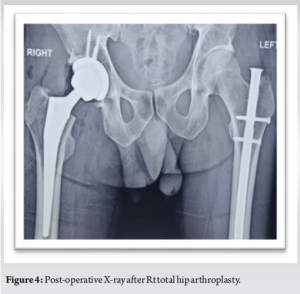
Case Report: We present a case of 37-year-old male with a history of recurrent posterior hip dislocation with 17-year duration. Magnetic resonance imaging demonstrated significant osteoarthritic changes in Rt hip along with posterior labrum tear. The patient was planned for right total hip arthroplasty. Intraoperatively, we found an intra-articular bony fragment of the posterior wall of the acetabulum along with posterior labrum tear of about 1 cm.
Discussion: This case highlights the importance of early recognition and stable reduction in the management of traumatic hip dislocations, as well as the need for thorough investigation and individualized treatment options for recurrent hip dislocation in adults.
Conclusion: Recurrent hip dislocations are rare in adults, but residual instability after closed reduction suggests ligamentous damage or acetabulum fractures. Early detection and stable reduction are the cornerstones of effective management.
Keywords: Recurrent hip dislocation, labrum tear, avascular necrosis.
Hip is one of the most stable synovial joints with excellent coverage of an acetabular cup over a large spherical head with supporting labrum and capsule. Merely 2% of all hip dislocations present with episodes of recurrent dislocation. Children are more likely to experience similar dislocations again, making adult recurrence extremely uncommon. In adults, posterior dislocations are 5–10 times more common than anterior dislocations. Etiology for recurrent hip dislocation includes structural hip abnormalities (fracture, labrum injury), ligamentous laxity, or existence of a localized lesion in the joint capsule. Pathoanatomy and prognosis are variable in adults and pediatric population. Multiple studies have shown that recurrent traumatic posterior dislocation of the hip was directly associated with fractures of the acetabulum [1]. Multiple studies have also shown the significance of labrum injuries in the stability of hip joint in comparison to the rest of soft tissue envelope around the hip (capsule and muscles) [2, 3]. Traumatic hip dislocations are very rare, lacking worldwide treatment guidelines for its management and rehabilitation [4]. An early recognition and stable reduction are the mainstay of effective management. In literature, we could not found any case with of adult recurrent posterior hip dislocation. Here, we describe a rare case of adult post-traumatic recurrent posterior hip dislocation associated with posterior wall acetabulum fracture and labrum avulsion with 17-year duration.
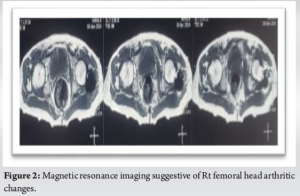
A 37-year-old male was brought to the emergency with complaint of right hip pain following fall from height. On examination, Rt lower limb was short with the attitude of hip flexion, adduction, and internally rotation. Distal pulses were equally palpable with the inability to dorsiflex his Rt foot and no sensory deficit with no associated injuries. X-ray pelvis with both hip anteroposterior AP view suggestive of Rt posterior hip dislocation, with no visible acetabular or femoral head fracture. He had a past history of recurrent right hip dislocation with his first episode encountered 17 years back following RTA Road traffic accident . He also sustained Lt shaft femur fracture. On further examination, he was diagnosed with Rt sciatic nerve injury leading to foot drop. The patient underwent closed reduction in the emergency for the right hip without anesthesia and was operated for Lt shaft femur fracture 2 days later. He had a recurrent episode 5 months later following a trivial fall which was managed by close technique but since then, he experienced mild pain while walking. Gradually, he was able to perform his activities of daily living. Post 3 years to it, the patient again sustained Rt hip dislocation after fall while playing and was reduced with closed reduction in a nearby hospital. A similar episode was again experienced after 2 years and the patient underwent closed reduction. So when the patient presented to us for the first time, he sustained posterior hip dislocation for the 5th time which was again managed by close reduction method. The patient was not investigated in the past for recurrent dislocation. Post-reduction radiographs confirmed a concentric reduction with degenerative changes in the femoral head (Fig. 1). Post-reduction magnetic resonance imaging (MRI) demonstrated significant osteoarthritic changes in Rt hip along with posterior labrum tear (Fig. 2).
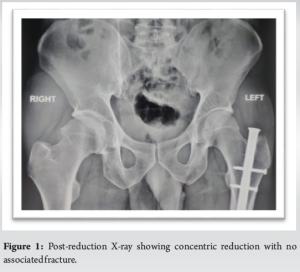
After discussion with the patient, he planned for right total hip arthroplasty through standard posterior approach. Short external rotators and posterior capsule were found to be completely intact but lax capsule. A tear of about 1 cm was identified in posterior acetabular labrum along the superior quadrant. After dislocating the hip, we found an intraarticular bony fragment of the posterior wall which might be the cause of early arthritic changes (Fig. 3). This fragment was removed and further arthroplasty was done with regular porous coated cup with standard liner (Fig. 4). Intraoperative assessment showed good stability with adequate ROM.
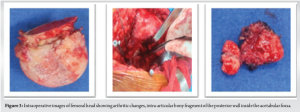
At 6-month follow-up, the patient has painfree functional range of motion with grade 5 muscle strength with no apprehension on joint loading attempts. Radiographs suggestive of stable implant. The patient did not experience any further episodes of instability (Fig. 5).
With the excellent support provided by surrounding soft tissue envelope and bony architecture, hip joint is highly stable than other joints like shoulder which frequently experiences repeated dislocations, resulting in rare incidences of recurrent hip dislocations with scarce literature. Usually, traumatic hip dislocations in adults develop complications such as avascular necrosis of femoral head, post-traumatic osteoarthritis, heterotopic ossification, and sciatic nerve palsy [5, 6]. In 1–17% of hip dislocations and up to 25% of subluxations, avascular necrosis develops [7]. One of the most important variables in the development of avascular necrosis is the time period from injury to hip reduction, which should not be longer than 24 h [5, 8]. 20% of cases with neurological injury are neuropraxia, which affects the sciatic nerve and is typically resolved on its own [5, 6]. In over 85% of cases, adequate reduction is accomplished by closed methods [9]. Open reduction may be required if reduction is non-concentric, unstable hip, or any accompanying lesion that requires surgical correction [9, 10]. Osteochondral fragments or soft tissue interposition is the main cause of repeated dislocations [5]. Hence, in such cases, high quality radiographs and additional evaluation by computed tomography or MRI are advised. Early MRI also enables to diagnosis intra-articular injuries, such as chondral shear damage to the acetabulum or femoral head with assessment of labrum and capsule [11, 12]. Hence, it helps to identify at-risk patients for recurrent instability which may require early surgical intervention. In literature, two case reports of young adults with recurrent posterior hip dislocation were found, and both patients exhibited a Bankart-type lesion. In one study, femoral head allograft was done for acetabular reinforcement with labral repair through bone tunnels and capsular plication was done [3]. In the second report, the lesion was treated without labral repair using an iliac crest bone block to reinforce the acetabulum [13]. Hence, in cases with labral injuries, capsulorrhaphy, bone block augmentation, or capsulorrhaphy in conjunction with bone block augmentation may be considered when the arthritic changes have not set in. However, in our case, the patient sustained arthritic changes most probably secondary to intra-articular bony fragment of posterior acetabulum wall leaving us with total hip replacement as the only option. Based on our understanding with available data, conservative measures can effectively treat single episode of hip dislocation or subluxation with no significant bone involvement. However, recurrent episodes warrant posterior stability testing under anesthesia with further investigation in the form of computed tomography (CT) or MRI to prevent such irreversible complications as we have encountered in our patient. Although reports of acetabular labrum injuries and their subsequent surgical repair have been documented in the literature. This is the first case report of adult recurrent posterior hip dislocation involving an intra-articular bone fragment with labral tear with osteoarthritic changes, which has changed the treatment approach totally in the form of arthroplasty.
Adult cases of recurrent hip dislocation are quite uncommon. When residual instability persists following closed reduction, there should be a strong suspicion of ligamentous damage or acetabulum fractures, for which MRI and CT scan should be advised. Effective management is based on early detection and stable reduction.
Despite the limited cases of recurrent hip dislocation, the approach to management like any other dislocation requires an emergent reduction for optimal results and minimizes the risk of complications such as avascular necrosis and post-traumatic arthritis.
References
- 1.Choyce CC. Traumatic dislocation of the hip in childhood, and relation of trauma to pseudocoxalgia: Analysis of 59 cases published up to January, 1924. Br J Surg 1924;12:52-9. [Google Scholar]
- 2.Dameron TB Jr. Bucket-handle tear of acetabular labrum accompanying posterior dislocation of the hip. J Bone Joint Surg Am 1959;41-A:131-4. [Google Scholar]
- 3.Lieberman JR, Altchek DW, Salvati EA. Recurrent dislocation of a hip with a labral lesion: Treatment with a modified Bankart-type repair. Case report. J Bone Joint Surg Am 1993;75:1524-7. [Google Scholar]
- 4.Sahin V, Karakaş ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture-dislocation of the hip: A long-term follow-up study. J Trauma 2003;54:520-9. [Google Scholar]
- 5.Wilchinsky ME, Pappas AM. Unusual complications in traumatic dislocation of the hip in children. J Pediatr Orthop 1985;5:534-9. [Google Scholar]
- 6.Engelbrecht PR, Grabe RP. Traumatic dislocation of the hip in children. A report of 4 cases. S Afr J Surg 1992;30:175-7. [Google Scholar]
- 7.Shindle MK, Ranawat AS, Kelly BT. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med 2006;25:309-26, ix-x. [Google Scholar]
- 8.Sahin V, Karakaş ES, Türk CY. Bilateral traumatic hip dislocation in a child: A case report and review of the literature. J Trauma 1999;46:500-4. [Google Scholar]
- 9.Başaran SH, Bilgili MG, Erçin E, Bayrak A, Öneş HN, Avkan MC. Treatment and results in pediatric traumatic hip dislocation: Case series and review of the literature. Ulus Travma Acil Cerrahi Derg 2014;20:437-42. [Google Scholar]
- 10.Yuksel S, Albay C. Early reduction of pediatric traumatic posterior hip dislocation is much more important than the treatment procedure. Pediatr Emerg Care 2019;35:e206-8. [Google Scholar]
- 11.Laorr A, Greenspan A, Anderson MW, Moehring HD, McKinley T. Traumatic hip dislocation: Early MRI findings. Skeletal Radiol 1995;24:239-45. [Google Scholar]
- 12.Ongeti K, Pulei A, Maru M, Kigera JW, Gakuya E. Recurrent traumatic posterior hip dislocation in labral avulsion: Case report. East Afr Orthop J 2017;11:33-5. [Google Scholar]
- 13.Rashleigh-Belcher HJ, Cannon SR. Recurrent dislocation of the hip with a “Bankart-type” lesion. J Bone Joint Surg Br 1986;68:398-9. [Google Scholar]