When we cannot salvage the bone (radius/ulna) in case of extensive damage due to infection, trauma, post-malignancy, or crushed injury then the single-bone forearm is a good and viable option instead of sacrificing the forearm function entirely.
Dr. Sushant Srivastava, Department of Orthopaedics, Mata Gujri Memorial Medical College and Lions Seva Kendra Hospital, Kishanganj, Bihar, India. E-mail: sushant391992@yahoo.co.in
Introduction: Chronic osteomyelitis is a debilitating bone infection that can lead to significant morbidity and functional impairment. This condition is often challenging to treat due to its complex nature and the ability of bacteria to form biofilms, which make them resistant to antibiotics. Early diagnosis and a multidisciplinary approach are crucial for successful management. Orthopedic surgeons often encounter chronic osteomyelitis as a difficult and persistent problem. The key to effective treatment lies in prompt diagnosis and a combination of surgical intervention and antimicrobial therapy. In cases of extensive bone loss or complex infections, a multidisciplinary team, including infectious disease specialists and plastic surgeons, may be necessary to optimize patient outcomes. Isolated involvement of the radius shaft is an uncommon presentation of chronic osteomyelitis.
Case Report: A 13-year-old male presented with persistent pain, deformity, and multiple draining sinuses on his right forearm. Radiographic imaging confirmed the diagnosis of diffuse chronic osteomyelitis. A two-stage treatment approach was employed to address the infection and restore bone integrity. The first stage involved aggressive debridement of infected tissue, implantation of antibiotic-coated bone cement to deliver sustained drug levels, and stabilization of the fracture using Joshi’s External Stabilizing System (JESS). The second stage focused on removing the antibiotic-coated bone cement once the infection was controlled and centralizing the ulna to improve forearm alignment and function.
Conclusion: This case highlights the importance of a tailored treatment approach for chronic osteomyelitis. Early intervention, aggressive debridement, appropriate antibiotic therapy, and surgical stabilization are essential components of successful management. In complex cases, a multidisciplinary team can provide optimal care and improve patient outcomes.
Keywords: Chronic osteomyelitis, Forearm, Diaphyseal, Radius, Centralization of Ulna
The forearm is described as a joint [1] due to its complex articulation. Pathology of any one bone can lead to loss of function, instability, and deformities at the elbow and wrist joint. Bone loss can be encountered in various conditions such as congenital deficiency, post-tumor resection, post-infection treatment, and traumatic loss [2-4]. Recommended treatment is the Masquelet technique in which the first stage involves debridement of bone defect and placement of antibiotic-coated bone spacer soft-tissue reconstruction which creates the induced membrane. The second stage involves removing the antibiotic-coated bone cement spacer and filling the space with a bone graft. The single-bone forearm is a salvage technique for the massive loss of bone due to serious trauma, malignant tumors [5], infections, or congenital deformity [6-8]. It is also described to treat the sequelae of hereditary multiple exostoses disease that affects the distal end of the ulna. Its adequate pediatric surgical management allows the patient to recover the form and function of the forearm. A study by Rasool [2] proposed that these defects can either be treated by replacement grafting, vascularized grafting, bone lengthening procedures, or by fusion of radius to ulna thus creating a one-bone forearm to achieve maximum restoration of functionality and stability. In special circumstances, bone deficiencies are so much that defects cannot be reconstructed through grafting, or adjacent joints are affected due to the long-standing nature of the disease as well as difficulty in the incorporation of the graft. The creation of a single-bone forearm is a valid salvage option. It provides a stable and cosmetically acceptable extremity at the expense of mild limitation of function. Osteomyelitis has been one of the most difficult and challenging problems. At present, morbidity and mortality from osteomyelitis are relatively low because of modern treatment methods, including the use of antibiotics and aggressive surgical treatment. The incidence of osteomyelitis has increased with the upgrade of diagnostic technology, and the increase in prosthetic implants in orthopedic surgery. The key to successful management is early diagnosis and appropriate surgical and antimicrobial treatment. A multidisciplinary approach is required, involving an orthopedic surgeon, an infectious disease specialist, and a plastic surgeon in complex cases with significant soft-tissue loss [4].
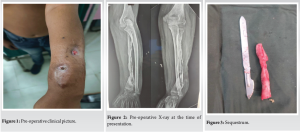
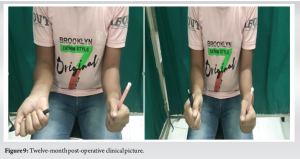
A 13-year-old boy presented to our outpatient department with complaints of pain, deformity, and multiple discharging sinus over Rt forearm for 5 months (Fig. 1 and 2) along with restricted forearm movement (supination and pronation). The pain was insidious in onset, dull aching in nature initially but after some time it was continuous in nature, non-radiating but aggravated on movement of the affected limb. Discharge was purulent in nature, scanty in amount, yellowish in color with thick viscous and no foul odor. Seven months back the boy had swelling for which incision and drainage were done. He did not have constitutional symptoms such as loss of weight, loss of appetite, or an evening rise in temperature. No history of pulmonary tuberculosis or similar illness in the family. His physical examination revealed deformity of the right forearm, multiple discharging sinus [1], tenderness, restriction in supination and pronation, and temperature was not raised. A plain radiograph of the forearm with wrist and elbow joint was done, and it showed diffuse chronic osteomyelitis (according to Cerny and Mader classification) lesion in the diaphysis of radius along with sequestrum along with distal radioulnar joint instability [DRUJ] and positive ulnar variance [2,3]. His erythrocyte sedimentation rate and C-reactive protein were raised and all other investigations were normal. The patient was counseled, and consent was taken for surgery and publication of his case report. Under regional block, the patient was placed on a table and the hand was placed on the hand (side) table as per the aseptic setting, Sequestrectomy (Fig. 3) and curettage were performed under anesthesia. Radius was exposed throughout its length through a dorsal “THOMPSON” approach. Bony sinuses were thoroughly curetted, dead and necrotic bone were removed, pus and gelatinous/fibrous tissue were curetted from the medullary cavity and wash was given with copious amounts of normal saline. Antibiotic-coated bone cement was implanted on K-wire and placed at the site of the bone. The patient was treated with a Joshi external stabilization system (JESS) [9] for correction of positive ulnar variance. The wound was closed in layers and was covered with dry dressings (Fig. 4 and 5). After 6 weeks the patient was again taken for removal of antibiotic-coated bone cement implantation, JESS removal and centralization of the ulna were done with a locking compression plate (Fig. 6). Follow-up X-ray showed signs of callus formation. The patient was followed up for 1 year (Fig. 7-9).


There are reports in the literature on the use of the Masquelet technique [11] in the treatment of bone gaps of the distal radius of infected non-union in children. Single-bone forearm creation generally consists of an osteotomy of the radius as well as the ulna, then fixing the radius to the ulna with or without resection of part of one or both bones of the forearm. Options in the management of bone gap due to infection, crushed injury, or post-malignancy, include tri cortico-cancellous grafting, tibial or fibular inlay or onlay grafting, free vascularized grafting, bone transport by distraction osteogenesis or the creation of a single bone forearm, either by centralizing the ulna over the carpus or achieving the union of the radius to the ulna to create a single-bone forearm. Other different techniques were described using the Masquelet technique, vascularized fibular graft [10], a free fibula flap [11], a different fixation [9], or adding a fusion of the distal radioulnar joint. Rasool [2] proposed that these defects can either be treated by replacement grafting, vascularized grafting, bone lengthening procedures, or by fusion of radius to ulna thus creating a one-bone forearm [3]. Devis et al. and Micev et al. reported problems in union after using allograft alone or mixed with bone graft substitutes and autograft. Allende [12] reported one case of the distal radius infected atrophic non-union with a bone gap of 2 cm in a 56-year-old female and five cases in which the bone gap was in radial diaphysis managed using a similar technique. This technique was comparable to our study where we used an external fixator along with cement spacer in stage one in case of distal radius pathology. The elbow joint, DRUJ, and PRUJ were not affected by the long-standing nature of the disease so we have created a single-bone forearm by joining the ulna with radius. An ample number of cases have been reported in the literature where one-bone forearm has provided satisfactory results in young individuals. Another reason for preference over grafting is also due to the important fact that one bone forearm continues to provide longitudinal growth. This salvage procedure has mostly been described in developing nations as there is a lack of facilities, limited financial resources yielding, lengthening procedures burdensome, and possible loss of follow-up. Distal radial physis is the major contributor to bone growth in this regard and chiefly it was preserved and functional in our case as well as other cases available in the literature.
One-bone forearm provides a stable upper limb with a good range of motion in younger patients. However, it must be considered only as a salvage procedure if other methods of treatment are not applicable.
In situations where the radius or ulna bone is severely damaged due to infection, trauma, post-cancer treatment, or crushing injuries, and cannot be repaired or salvaged, a single-bone forearm can be a viable surgical option. This procedure involves removing the damaged bone and allowing the remaining bone to adapt and function. This approach can preserve limb function and prevent the need for amputation, offering a better quality of life for the patient.
References
- 1.Allende C, Allende BT. Posttraumatic one-bone forearm reconstruction. A report of seven cases. J Bone Joint Surg Am 2004;86:364-9. [Google Scholar]
- 2.Rasool MN. Radioulnar fusion for forearm defects in children-a salvage procedure. SA Orthop J 2008;7:60-7. [Google Scholar]
- 3.Dabovic GD. Osteomyelitis. In: Azar FM, Canale ST, Beaty JH., editors. Campbell’s Operative Orthopaedic. 14th ed. Amsterdam, Netherlands: Elsevier; 2020. p. 786. [Google Scholar]
- 4.Kesani AK, Tuy B, Beebe K, Patterson F, Benevenia J. Single-bone forearm reconstruction for malignant and aggressive tumors. Clin Orthop Relat Res 2007;464:210-6. [Google Scholar]
- 5.Schiffman B, Hanel D. The one bone forearm. Hand Clin 2020;36:531-8. [Google Scholar]
- 6.Multani I, Xu J, Manji J, Lawson RD, Graham DJ, Sivakumar BS. The one-bone forearm: A review. Hand (N Y) 2022;19:12-23. [Google Scholar]
- 7.Wang KK, Vuillermin CB, Waters PM. Single-bone forearm as a salvage procedure in recalcitrant pediatric forearm pathologies. J Hand Surg Am 2020;45:947-56. [Google Scholar]
- 8.Schachinger F, Girsch W, Farr S. Soft-tissue distraction prior to single bone forearm surgery in ulnar longitudinal deficiency: A report of two cases. J Hand Surg Asian Pac Vol 2018;23:153-7. [Google Scholar]
- 9.Artiaco S, Ciclamini D, Teodori J, Dutto E, Benigno T, Battiston B. One bone forearm with vascularized fibular graft. Clinical experience and literature review. Injury 2020;51:2962-5. Wang Y, Zhou M, Wu Y, Ma Y, Liu J, Rui Y. One-bone forearm reconstruction and distal radioulnar joint fusion for emergency one-stage operation in traumatic major bone defect of forearm. Injury 2020;51:1828-33. [Google Scholar]
- 10.Kim SY, Chim H, Bishop AT, Shin AY. Complications and outcomes of one-bone forearm reconstruction. Hand (N Y) 2017;12:140-4. [Google Scholar]
- 11.Mukhopadhaya J, Bhadani JS. Masquelet technique for infected distal radius fractures with gaps in paediatric age group. Trauma Case Rep 2021;37:100568. [Google Scholar]
- 12.Allende D. Cement spacers with antibiotics for the treatment of posttraumatic infected nonunions and bone defects of the upper extremity. Tech Hand Up Extrem Surg 2010;14:241-7. [Google Scholar]
- 13.Davis JA, Choo A, O’Connor DP, Brinker MR. Treatment of infected forearm nonunions with large complete segmental defects using bulk allograft and intramedullary fixation. J Hand Surg Am 2016;41:881-7. [Google Scholar]
- 14.Micev AJ, Kalainov DM, Soneru AP. Masquelet technique for treatment of segmental bone loss in the upper extremity. J Hand Surg Am 2015;40:593-8. [Google Scholar]