While repeated casts and bracing may effectively correct flexion contracture in mild cases of congenital patella dislocation, surgical intervention is necessary to restore the displaced patella.
Dr. C Sitsabesan, Department of Orthopedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai - 600 116, Tamil Nadu, India. E-mail: sitsabesan@sriramachandra.edu.in
Introduction: Congenital patellar dislocation is a very rare knee disorder characterized by the lateral dislocation of patella from birth, which cannot be reduced. The disorder affects both knees and is a persistent condition. Bony and soft tissue anomalies are part of the pathoanatomy of this disorder. The diagnosis is clinically confirmed by the presence of a patella that is displaced posterolaterally. Neglected ailments may lead to severe functional impairment and degenerative changes in the knee joint, resulting in increasing disability over time. Usually, correction by surgery is the recommended treatment approach.
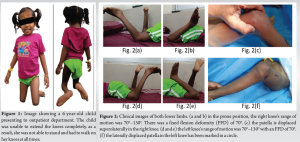
Case Report: A 6-year-old female child was diagnosed with congenital patella dislocation in both knees. The child was unable to walk due to this disorder. The range of movement was 70°-130° in both knees. Subsequently, the child had to undergo surgery to repair the knee defect in bilateral lower limbs. The patient’s condition at the time of presentation, the surgical procedure, and clinical outcomes at the end of 1 year has been described.
Conclusion: Congenital dislocation of the patella is an uncommon disease that typically develops from birth. Although repeated casting and braces are effective for treating the flexion contracture of the affected knee in case of congenital patella dislocation, repositioning the displaced patella requires surgical intervention. To prevent any possible problems and long-term consequences of the disease, it is essential to identify it and perform a surgical intervention to repair the deformity as soon as possible. Usually, surgical correction is the recommended treatment approach for this congenital disorder.
Keywords: Congenital dislocation of the patella, congenital patellar dislocation, knee defect, flexion contracture, congenital disorder.
Congenital patellar dislocation (CPD) is a very rare knee disorder where patella is dislocated laterally from birth, which cannot be reduced. The exact prevalence is undetermined and it may be isolated or syndromically associated with Down’s syndrome, Arthrogryposis, Nail-Patella syndrome, Larson syndrome, and diastrophic dysplasia. Additional factors that can contribute to patellofemoral instability include malalignment in the coronal plane like excess genu valgum, malalignment in the axial plane like excess femoral anteversion and/or outward rotation of the tibia, high-riding patella, pathology of the vastus medialis obliquus (VMO) muscle, trochlear dysplasia, hyper ligament laxity as in Down’s and Ehlers Danlos syndrome [1]. The disorder is often bilateral and refractory for non-operative treatment. The pathoanatomy of this disorder includes both bones and soft tissues. The bony component consists of hypoplastic or absent patella, shallow trochlea, and extorsion of the tibia. The soft-tissue pathology consists of contracted lateral tissues, such as the retinaculum, iliotibial band, and quadriceps femoris. The patella may not be detectable or may be placed superolateral to the trochlea, and it is firmly attached to the exterior surface of the lateral femoral condyle. The hypoplastic patella and the surrounding structures are covered by a common fascia, making it difficult to figure out the boundaries of the patella [2]. The diagnosis is clinically confirmed by the persisting superolateral displacement of the patella. Other associated deformities may include knock-knees, external tibial torsion, knee contractures, and fixed flexion deformity (FFD). Neglected ailments may lead to severe functional impairment and major degenerative changes in the knee joint, resulting in increasing disability. While non-operative care by monitoring may have a negative impact on untreated patellar dislocation on long-term knee function, usually correction by early surgery is the recommended treatment to restore patellofemoral function. The study demonstrates an uncommon case of a 6-year-old female child with neglected CPD in both knees. Subsequently, surgery was required to rectify the deformity and reestablish mobility. (Fig. 1)
The patient, a 6-year-old female child from southern India, presented to the orthopedic outpatient clinic for her bilateral knee deformity and inability to stand up or walk since birth. Although pain-free, the functional restriction in both of her knees was the primary source of considerable psychological distress, which in turn hindered her social relationships with individuals of her age. Born to a 2° consanguineous marriage, the child was delivered by a normal vaginal delivery at the expected gestational age. Her prenatal and postnatal phases were uneventful.

She had repeated applications of plaster casts at another hospital until the age of 3 years but no interventional procedures were performed. Her developmental history showed the ability to achieve gross motor milestones except for walking, inclusive of achieving fine motor skills, language development, and social milestones were normal for her age.
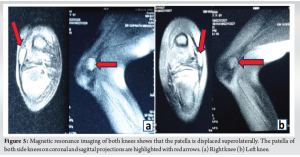
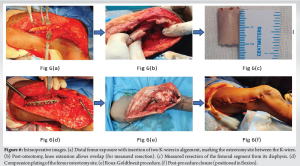
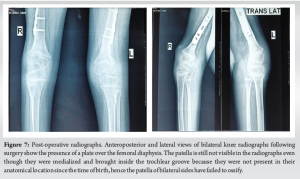
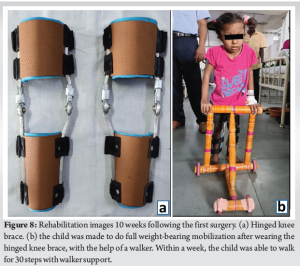
On physical examination, in supine, the child’s hips were in flexion, bilateral knees in flexion with bilateral ankle at ease. Prominent FFD in bilateral knees was noted. There was no tenderness on palpation in either knee. Both knees showed prominent femoral condyles with shallow sulcus between the condyles, absence of patella in trochlear groove bilaterally, and hypoplastic patella present on the lateral aspect of knees. Bilateral FFD of 70° was due to flexion contracture and bowstring effect of extensors of the knee. The range of motion (ROM) was measured in the prone position to be 70°–130° bilaterally. The thigh foot angle was found to be around 45° suggesting an external tibial torsion. No deformities were noted in the upper limbs or any other parts of the body. Bilateral hip examination was found to be normal with no associated spine pathology. (Fig. 2) Plain radiographs (frontal, lateral projection, and skyline view) of both knees showed absent patella from the trochlear groove bilaterally. Magnetic resonance imaging (MRI) revealed that the patella was hypoplastic and was located superolaterally on both sides. The patient underwent staged surgery for correction of her bilateral knee deformity – the right knee, followed by the left knee at 6 weeks interval. For distal soft-tissue realignment, the Roux-Goldthwait procedure was planned and performed. Intraoperatively, the hamstrings were found to be tight on attempting knee extension. Furthermore, keeping in mind that the knees of this child being in FFD since birth, and sudden extension of the knee is likely to stretch the neurovascular structures, femoral shortening osteotomy was performed before soft-tissue realignment. The steps include lateral thigh soft tissue and intermuscular septum release + posterolateral knee capsulotomy + femoral shortening osteotomy and fixation by plate and screws + medialization of patella. The vastus medialis insertion was transferred to the lateral half of patella. The lateral half of the patellar tendon was partially medialized and distalized (Roux-Goldthwait procedure). Postoperatively, the knee was placed in an above-knee cast at 15° of flexion. The same procedure was repeated on the left knee after 6 weeks. Post-surgery, the lower limbs were immobilized in an above-knee plaster of Paris cast for a month, with 15° of knee flexion. After the removal of the cast, the patient was started on active physiotherapy: Isometric quadriceps and hamstring strengthening exercises. After 2 and a 1/2 months following surgery, a hinged knee brace was provided for both knees. Initially, the child was instructed to stand using the knee brace. As time progressed, she was gradually encouraged to put her entire body weight on her legs and move about with the assistance of a walker.
At 1 year follow-up, the patient could perform active flexion and extension of both her knees. The ROM was 15°–80° bilaterally. The patient started to walk without any assistance and she has started going to school as well. (Fig. 3 & 4).
CPD is believed to occur because of a lack of internal rotation in the myotome responsible for the development of the femur, quadriceps muscle, and extensor mechanism. Usually, failure occurs during fetal growth phase, which is from the 8th to 10th week [3]. Due to this reason, the whole extensor mechanism is located towards the lateral aspect of the knee, and on contraction of the muscles, it acts as a flexor mechanism, and active extension is restricted. Prompt detection of CPD is essential; however, it may sometimes go undetected. This is mostly because a child’s patella usually undergoes ossification by the age of 3 years, rendering it invisible on a plain radiograph. Radiological assessments, particularly MRI, and computed tomography are crucial for the identification and characterization of pathology related to CPD, such as cartilage lesions or trochlear dysplasia. Nevertheless, the identification of this condition mostly relies on clinical assessment [4]. MRI is capable of accurately differentiating within the cartilages of neighboring joint components [5], making it important during pre-operative evaluations and planning a surgical intervention. Given the pathological characteristics seen in individuals with CPD, such as patellar malformations, trochlear dysplasia, and pathology in the vastus medialis oblique, surgical correction is the only successful treatment. Repeated application of casts and the use of braces are efficient techniques for managing the minimal flexion contracture in the affected knees. However, repositioning the displaced patella requires surgical intervention [6]. Several procedures have been mentioned in the literature that would achieve the correction by bringing the patella inside the trochlear groove and performing distal soft-tissue repair to maintain the patella in its anatomical location. Some of these distal soft-tissue repair procedures are the modified Langenskiöld procedure[7] and Roux-Goldthwait procedure [8]. Undetected and untreated CPD naturally progresses to cause many knee abnormalities, such as flattened hypoplasia of lateral femoral condyle, exacerbation of knock-knee deformity, and external tibial rotation. The patella that has been dislocated stays underdeveloped and, due to the uneven distribution of weight, there is an early reduction in the space between the joints on the side of the knee, along with the formation of cysts under the cartilage. Therefore, it is crucial to identify and perform surgical intervention for this issue in early childhood [9]. With regard to the reduction and restoration of a displaced patella, Gordon and Schoenecker [10] evaluated the outcomes of seventeen surgical treatment procedures. In addition, lateral release and advancement of the VMO were performed on each and every one of their patients as part of a comprehensive surgery. A transfer of the patellar tendon or the tibial tubercle medially was performed during that surgery. (Fig. 5) The choice was made based on the condition of the physis. Each of these patients witnessed an improvement in their range of movement and level of physical activity after an average follow-up period of 5.1 years, with the exception of one with re-dislocation in the early post-operative period. The case that has been discussed here had bilateral knee ROM of 70°–130° at the time of presenting to the hospital. This caused problems with activities of daily living like walking, going to school, and playing with kids of the same age. The child was given false reassurance and underwent multiple casting and bracing for almost 3 years elsewhere, without any positive results. The diagnosis of CPD was suspected clinically and through X-ray imaging [11]. In the normal knee, patellar ossification begins in the age range of 3–5 years [12] but in cases of CPD with shallow trochlea, the delayed ossification of the hypoplastic patella remains challenging for its diagnosis. Due to the presence of the patella in a non-anatomical position as in this case, that is, superolaterally, and non-visibility on plain radiographs, MRI scan is mandatory to confirm the diagnosis and for surgical planning. Lateral thigh soft tissue and intermuscular septum release + posterolateral knee capsulotomy were done. Femoral shortening osteotomy was done to prevent stretch on the neurovascular structures [13]. This allowed medialization of patella followed by the final distal realignment procedure. Postoperatively, the knee was placed in an above-knee cast at 15° of flexion. This would prevent neurovascular stretching, provide support to the hypoplastic patellar reduction, and protect the distal repair that was performed (Roux-Goldthwait procedure). The casts were removed after 6 weeks post-procedure and this was followed by a strict physiotherapy regimen, and after 1 year, the child had a knee ROM of 15°–80° on both knees. The child was able to walk without any kind of support and had no complaints of knee instability. She also started going to school and this improved her social life to a tremendous extent. Although the knee ROM achieved after 1 year of surgery was just 65° (15°–80°), with a residual FFD of 15°, still the activities of daily living such as walking, climbing up and down stairs, sitting on a chair were all possible. The functionality of both knees was better than before. (Fig 6-9).
CPD is a very rare medical condition that typically develops at birth. It could give rise to varying degrees of knee flexion deformity in addition to physical, mental, and social deterioration of the affected individual. If left untreated, the disorder could give rise to refractory severe deformities. While repeated casts and bracing may effectively cure mild flexion deformity, surgical intervention is necessary to restore the displaced patella. To avoid any complications and long-term consequences of CPD, it is essential to promptly identify it and perform a surgical intervention to repair the deformity as soon as possible. Usually, correction by surgery is the recommended treatment approach for this congenital disorder.
In this case of congenital dislocation of patella with severe knee deformity, femoral osteotomy and shortening were performed to reduce the tightness of the quadriceps and the hamstring muscles and also, to prevent stretch on the neurovascular structures.
References
- 1.Ramos O, Burke C, Lewis M, Morrison MJ, Paley D, Nelson SC. Modified Langenskiöld procedure for chronic, recurrent, and congenital patellar dislocation. J Child Orthop 2020;14:318-29. [Google Scholar]
- 2.Ghanem I, Wattincourt L, Seringe R. Congenital dislocation of the patella. Part I: pathologic anatomy. J Pediatr Orthop 2000;20:812-6. [Google Scholar]
- 3.Koplewitz BZ, Babyn PS, Cole WG. Congenital dislocation of the patella. AJR Am J Roentgenol 2005;184:1640-6. [Google Scholar]
- 4.Miguel Sá P, Raposo F, Santos Carvalho M, Alegrete N, Coutinho J, Costa G. Congenital dislocation of the patella - clinical case. Rev Bras Ortop 2015;51:109-12. [Google Scholar]
- 5.Recht M, Bobic V, Burstein D, Disler D, Gold G, Gray M, et al. Magnetic resonance imaging of articular cartilage. Clin Orthop Relat Res 2001;391:S379-96. [Google Scholar]
- 6.Langenskiöld A, Ritsilä V. Congenital dislocation of the patella and its operative treatment. J Pediatr Orthop 1992;12:315-23. [Google Scholar]
- 7.Mo Y, Jing Y, Wang D, Paley D, Ning B. Modified Langenskiöld procedure for congenital patella dislocations in pediatric patients. BMC Musculoskelet Disord 2022;23:241. [Google Scholar]
- 8.Ruzzini L, Donati F, Russo R, Costici PF. Modified roux-goldthwait procedure for management of patellar dislocation in skeletally immature patients with down syndrome. Indian J Orthop 2019;53:122-7. [Google Scholar]
- 9.Thabit G 3rd, Micheli LJ. Patellofemoral pain in the pediatric patient. Orthop Clin North Am 1992;23:567-85. [Google Scholar]
- 10.Gordon JE, Schoenecker PL. Surgical treatment of congenital dislocation of the patella. J Pediatr Orthop 1999;19:260-4. [Google Scholar]
- 11.Stanisavljevic S, Zemenick G, Miller D. Congenital, irreducible, permanent lateral dislocation of the patella. Clin Orthop Relat Res 1976;116:190-9. [Google Scholar]
- 12.Jones RD, Fisher RL, Curtis BH. Congenital dislocation of the patella. Clin Orthop Relat Res 1976;119:177-83. [Google Scholar]
- 13.Congenital Dislocation of the Patella. Available from: https://www.limblength.org/conditions/congenital-dislocation-of-the-patella [Last accessed on 2024 Aug 30]. [Google Scholar]