The accumulation of the bluish-black pigment in Alkaptonuria in the spine and major joints can lead to ochronotic degenerative arthropathy.
Dr. Javid Mohammadzadeh Azarabadi, Department of Orthopaedic and Traumatology, Faculty of Medicine, Baskent University, Konya, Turkey. E-mail: dr_jma_md@yahoo.com
Introduction: Alkaptonuria (AKU) is a genetic disease caused by a deficiency in the homogentisate 1,2-dioxygenase enzyme. This deficiency leads to elevated levels of homogentisic acid and its oxidized form, benzoquinone acetic acid. Together, these substances lead to the bluish-black coloring of the bone and cartilage, along with calcification, inflammation, degeneration, and ultimately osteoporosis. The accumulation of pigments in the spine and major joints can result in ochronotic degenerative arthropathy.
Case Report: In this study, we present the case of a 65-year-old Palestinian man who exhibited musculoskeletal manifestations of AKU for 15 years. He was successfully treated with hip replacement, and we conducted a literature analysis to provide a comprehensive summary of the etiology, clinical characteristics, and potential treatments.
Conclusion: AKU affects the spine and large joints. At present, there is no cure for this condition. A diet low in Vitamin C, antioxidants, tyrosine, and phenylalanine may delay the progression of AKU, but the long-term consequences are still unknown. Joint replacement may be recommended to relieve joint pain and improve mobility.
Keywords: Ochronotic alkaptonuria arthropathy, homogentisic acid, orthopedic surgery, hip arthroplasty.
In alkaptonuria (AKU), the third enzyme in tyrosine breakdown and homogentisic acid dioxygenase (HGD) is absent which results in the excretion of homogentisic acid (HGA) in urine and the formation of an ochronotic pigment in connective tissues and bones [1]. In most cases, children show no symptoms at all. However, ochronosis can start showing up as a blue-dark or brown pigment in the sclera or ear cartilage in the second to third decade of life. Other symptoms include kidney stones (prostatic, salivary glands, and, gall bladder), back or peripheral joint pain, tendon, muscle, or ligament tears, osteoporosis, fractures, or renal failure [2]. AKU is caused by missense mutations in the HGD gene, corresponding to human chromosome 3q21-q23. The prevalence of these variations ranges from around 1:1,000,000 to 250,000,000 in most ethnic group. Several reports in the literature have documented the successful treatment of ochronotic arthropathy with total hip arthroplasty (THA). Kerimoglu et al. highlighted the positive outcomes of hip arthroplasty in patients with ochronotic degeneration, emphasizing its role in alleviating pain and restoring mobility [4], Similarly, Prabhakar et al. described a series of cases where THA provided significant symptomatic relief and improved quality of life in patients with ochronotic arthropathy underscoring its efficacy in advanced stages of joint degeneration [5]. Bhattacharjee et al. reported a recent case demonstrating excellent functional recovery following THA in a patient with ochronosis, further validating the procedure’s benefits [6]. Liu et al. also documented the effective use of combined hip and knee arthroplasty in a patient with ochronotic arthropathy, showing the potential for comprehensive management of multiple joint involvements [7]. These findings collectively highlight THA as a reliable surgical intervention for managing severe ochronotic joint damage. In this case, we follow a 65-year-old man’s journey from a long list of orthopedic complaints to an AKU diagnosis and hip replacement. The occupied Palestinian territory has never before seen an instance of this uncommon sickness. Give a paragraph regarding previous reports of the same condition that successfully treated with THA (see suggested reference in the comment of the reference section).
A 65-year-old Palestinian man is a known case of hypertension, osteoarthritis (OA), AKU, and nephrolithiasis with a body mass index of 22.5, was seen in an orthopedic clinic due to his 15-year history of recurrent pain of the spine and peripheral joints, as well as a recent hip pain. This patient had rheumatology consulted and been managed with many painkiller and antiinflammatory drugs 8 years ago, and articulatory corticosteroid injections in the previous year, with no response or benefits, he also reported experiencing a few minutes of stiffness first thing in the morning, which gradually got worse as he got moving around. There is some black hyperpigmentation of the bilateral ear. The patient presented with soreness over the left hip joint, right glenohumeral joint, associated with recurrent joint pain, there are no any joint effusions. The patient’s left hip and wrist had limited mobility throughout the examination, but there was no effusion or infection.
His hemoglobin levels were 11.4 g/dL, which falls within the normal range of 13.3–17.7 g/dL. His whole metabolic panel, ferritin, and transferrin readings were all within the normal range as well, thus we may consider him to have mild anemia. Qualitative organic acid analysis revealed an increased content of HGA in the urine shows that his urine sample became brownish dark after being alkalinized (Fig. 1a). Our patient was American Society of Anesthesiologists III score as he has severe systemic disease (ochronotic arthropathy with hypertension and nephrolithiasis) that limits his daily activities but is not incapacitating.
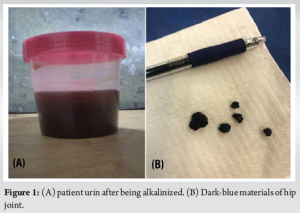
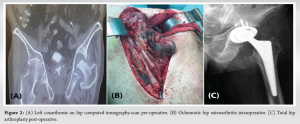
The computed tomography radiographic results of the hip joint showed some characteristic findings due to the deposition of HGA in the joint and surrounding tissues which include joint space narrowing, calcification of articular cartilage, subchondral sclerosis, and osteophyte formation, which are signs of ochronotic arthropathy. In addition, cystic changes in the bone and the elevated urine HGA levels confirmed the diagnosis of AKU. It was decided to perform a THA since the clinical picture showed severe OA. The surgical procedure was performed using a posterolateral approach to the hip, providing excellent exposure while preserving the abductor muscles essential for post-operative function. A modular, third-generation total hip replacement system was used, featuring a ceramic-on-polyethylene bearing surface to ensure durability and minimize wear. Both the femoral stem and acetabular cup were fixed using a cementless press-fit technique, promoting long-term bone integration. The patient underwent spinal anesthesia, which provided effective pain control and reduced the risks associated with general anesthesia, particularly given his comorbid conditions of hypertension and nephrolithiasis. Intraoperatively, bluish-black ochronotic pigmentation was observed in the bone and connective tissues, consistent with ochronosis (Fig. 1b). The degenerative changes and brittle nature of the bone required careful handling during implant placement to avoid fractures, and meticulous dissection was necessary to prevent tendon injuries. No significant intraoperative complications, such as fractures or excessive bleeding, were encountered. Postoperatively, the patient was mobilized early, beginning weight-bearing on the 1st day under the guidance of physical therapy. Pain was effectively managed with a combination of opioids and non-steroidal anti-inflammatory drug s. The surgical site healed well, with no signs of infection or wound dehiscence, and the patient reported significant pain relief and improved mobility within 25 days. Follow-up showed no signs of implant loosening or failure, and the range of motion in the hip was restored to a functional level, highlighting the success of the intervention (Fig. 2).
Ochronotic arthropathy is a rare manifestation of AKU, which characterized by progressive degeneration of the large joints, such as the hip and knee, due to the accumulation of HGA. Surgical intervention, specifically THA, is often the treatment of choice for patients with severe joint degeneration. This case highlights the successful management of ochronotic hip arthropathy with THA, consistent with findings reported in the literature. Several studies have documented the efficacy of THA in alleviating pain and restoring function in patients with ochronotic arthropathy. Arasu and Prasanna described three cases of ochronotic hip arthropathy successfully managed with THA, emphasizing the importance of meticulous surgical planning to address the challenges posed by ochronotic pigmentation and brittle bone tissue [8]. Similarly, Pachore et al. reported long-term outcomes of primary hip arthroplasty in patients with ochronotic hip arthritis, with follow-up periods ranging from 3 to 24 years, demonstrating sustained pain relief and functional improvement [9]. Prabhakar et al. further supported the role of THA, noting significant symptomatic relief and improved quality of life in patients with advanced ochronotic arthropathy [5]. Our findings align with those of Bhattacharjee et al., who documented a case of ochronotic arthropathy treated with THA, resulting in excellent functional recovery [6]. Liu et al. also highlighted the effective use of THA and total knee arthroplasty in managing multiple joint involvements in ochronotic patients [7]. These studies collectively underscore the importance of THA as a reliable intervention for managing advanced ochronotic joint damage, even in complex cases with extensive pigmentation and degenerative changes. Intraoperatively, ochronotic pigmentation presents unique challenges, including brittle bones and stiff connective tissues prone to tearing. As observed in our case, meticulous surgical technique and careful handling of tissues are essential to minimize complications. The use of cementless implants, as employed in this case and supported by , offers the advantage of better long-term bone integration and reduced risk of implant loosening [8]. In cases of alkaptonuria, the use of cementless implants in total hip replacement (THR) has been reported with favorable outcomes. For instance, a case study published in 2023 described a 57-year-old male patient with bilateral hip pain who underwent bilateral hip replacements. During surgery, black bone tissue and tendons were observed, leading to the diagnosis of alkaptonuria. The study did not specify the type of implants used, but it highlighted the importance of considering atypical arthropathy in such cases [9]. Despite the overall success of THA in ochronotic patients, certain limitations must be acknowledged. The metabolic nature of the disease predisposes patients to ongoing degeneration of other joints and tissues, necessitating a comprehensive approach to long-term management. In addition, as noted by Pachore et al., the outcomes of THA in ochronotic arthropathy may vary based on the extent of joint damage and the presence of systemic comorbidities [10]. Future research should focus on long-term outcomes, the role of adjunct medical therapies to slow disease progression, and strategies to optimize perioperative care in this unique patient population.
Although there is no definitive treatment for AKU, joint replacement may be recommended to relieve joint pain and increase the range of motion in patients with ochronotic degenerative arthropathy.
In degenerative joint diseases, the aim is not only to treat that joint, but also to investigate the cause of that disease and, if possible, to eliminate it. Although there is no definitive treatment for some genetic diseases such as AKU, early diagnosis and initiation of treatment may reduce or delay the damage of the disease.
References
- 1.Mistry JB, Bukhari M, Taylor AM. Alkaptonuria. Rare Dis 2013;1:e27475. [Google Scholar | PubMed]
- 2.Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of alkaptonuria. N Engl J Med 2002;347:2111-21. [Google Scholar | PubMed]
- 3.Nemethova M, Radvanszky J, Kadasi L, Ascher DB, Pires DE, Blundell TL, et al. Twelve novel HGD gene variants identified in 99 alkaptonuria patients: Focus on ‘black bone disease’ in Italy. Eur J Hum Genet 2016;24:66-72. [Google Scholar | PubMed]
- 4.Kerimoglu S, Onder C, Aynaci O, Malkoc CH. Hip arthroplasty for ochronosis. Saudi Med J 2005;26:1812-4. [Google Scholar | PubMed]
- 5.Prabhakar R, Ponnaian G, Gopal P, Prasad R, Pathania K. Total hip arthroplasty in ochronotic arthropathy. J Arthroscopy and Jt Surg 2022;9:43-6. [Google Scholar | PubMed]
- 6.Bhattacharjee S, Ahlawat A, Prasad A, Das RK. Total hip arthroplasty in ochronotic arthropathy: A case report. J Orthop Case Rep 2023;13:86-91. [Google Scholar | PubMed]
- 7.Liu Y, Li C, Zhang Z, Lu X, Zhang H. Ochronotic arthropathy effectively treated with total hip and total knee arthroplasty: a case report. Front Med (Lausanne). 2023 Sep 19;10:1212580. doi: 10.3389/fmed.2023.1212580. PMID: 37795417; PMCID: PMC10546056. [Google Scholar | PubMed | CrossRef]
- 8.Arasu JA, Prasanna AA. Total hip arthroplasty for ochronosis: A report of three cases. J Orthop Case Rep 2022;12:23-7. [Google Scholar | PubMed]
- 9.Shayan-Moghadam R, Zolghadr H, Babaei-Nejad E, Shafiee H. Non-cemented Total Hip Arthroplasty in a Rare Case with Black Hip, A Case Report. Adv Biomed Res. 2024 Oct 28;13:95. doi: 10.4103/abr.abr_199_23. PMID: 39717259; PMCID: PMC11665151. [Google Scholar | PubMed | CrossRef]
- 10.Pachore JA, Shah VI, Upadhyay S, Shah K, Sheth A, Kshatriya A. Primary hip arthroplasty for the treatment of alkaptonuric hip arthritis: 3- to 24-year follow-ups. Arthroplasty 2019;1:8. [Google Scholar | PubMed]