Successful bone healing can occur despite significant complications like the Z-effect and implant failure.
Dr. Niranjan Sunil Ghag, Department of Orthopedics, Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai, Maharashtra, India. E-mail: niranjanghag95@gmail.com
Introduction: Intertrochanteric femur fractures are common in the elderly, often resulting from low-energy trauma such as falls. Standard treatment typically involves internal fixation, which generally leads to good outcomes. However, complications like the Z-effect, where proximal screws of an intramedullary nail migrate in opposite directions, and implant failure can significantly impact healing.
Case Report: A 58-year-old male patient sustained an intertrochanteric femur fracture following a fall. The fracture was treated with an intramedullary nail. Postoperatively, the patient developed the Z-effect, characterized by the migration of proximal screws in opposite directions. Subsequently, the implant failed, resulting in a broken nail and screw. Despite these complications, radiographic evaluations over time revealed progressive healing, and the patient eventually achieved complete bony union.
Conclusion: This case underscores the potential for successful bone healing even in the presence of significant complications such as the Z-effect and implant failure. The patient’s complete bony union despite these challenges emphasizes the importance of diligent follow-up and adaptive management strategies in orthopedic practice. This case contributes to the understanding of fracture healing dynamics and highlights the resilience of bone healing mechanisms.
Keywords: Healing against odds, intertrochanteric femur fracture complication, reverse Z effect.
Intertrochanteric femur fractures are prevalent, with increasing risk with aging [1]. Management of these fractures has plethora of options, but Proximal Femoral Nail (PFN) is widely considered as the optimal mode of treatment [1]. The purpose of these two lag screw intramedullary nail systems is to improve rotational stability and provide stable fixation in the femoral head [2]. This reduces the chances of cut-out and subsequent fixation failure by providing stability with a much higher strength against failure [2]. Nevertheless, this design brings about a unique form of failure referred to as the Z-effect phenomena [2,3]. This phenomenon takes place throughout the period of weight-bearing rehabilitation and is distinguished by the outward movement of the lower lag screw and the inward movement of the upper lag screw [2,3]. In contrast, the inverted Z-effect refers to the inward movement of the lower lag screw and the outward movement of the upper lag screw [2,3]. The Z-effect is thought to be a biomechanical phenomenon, maybe caused by an imbalance in the compressive strength of the head and neck, resulting in varus collapse with a caput-collum-diaphyseal angle <125 (angle be between the femoral neck axis and diaphysis) [2,4]. The Z-effect is caused by several reasons, including an unstable medial cortex, the medial migration resulting from a weakened lateral buttress, and continuous friction within the femoral head paired with axial loading in varus [2]. This report presents a rare instance of successful bony union despite the occurrence of the Z-effect and implant failure, highlighting the resilience of bone healing under adverse conditions. This case underscores the importance of understanding the biological and mechanical factors that can contribute to successful outcomes even when traditional expectations suggest otherwise.
Patient profile
A 58-year-old male presented to our emergency department following a fall that resulted in an intertrochanteric femur fracture of the right side. The patient had no significant medical history of note and was in generally good health before the injury (ASA-I). Physical examination and radiographic imaging confirmed a right-sided intertrochanteric femur fracture (Fig. 1).

Surgical intervention
The patient underwent surgical fixation with a short PFN implant (close reduction and internal fixation). Intraoperative fluoroscopy confirmed the satisfactory placement of the hardware. The surgery was uneventful, and post-operative radiographs showed appropriate alignment and fixation of the fracture fragments (Fig. 2).
Post-operative management
Following the surgery, the patient was encouraged to begin immediate weight-bearing as tolerated on 2nd day after the surgery. This approach aimed to promote early mobilization and enhance the biological environment for fracture healing. The patient was compliant with the post-operative rehabilitation protocol and experienced an initial satisfactory recovery.
Follow-up and complication
At the 13-month follow-up, the patient presented to the outpatient department with complaints of on-and-off pain in the right hip since past 3 months. Clinical examination revealed terminal restriction of movements with difficulty to sit cross-leg or squat. Radiographic evaluation revealed the reverse Z-effect with broken proximal de-rotation screw, characterized by the medial migration of the lag screw into the hip joint. This finding was concerning for mechanical failure and raised questions about the stability of the fracture site. Serial radiographs and clinical examinations were used to confirm the bone union preoperatively (Fig. 3 and 4).

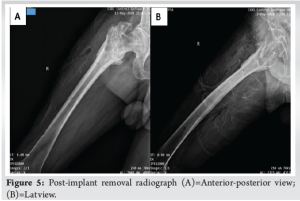
Implant removal and outcome
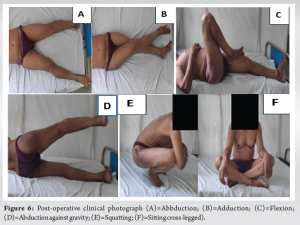
Given the implant failure, the decision was made to proceed with the removal of the broken PFN. Post-removal radiographs confirmed the absence of the fracture and the integrity of the bony union. The patient was instructed to avoid putting any weight on the affected limb for a period of 6 weeks, after which they might gradually begin to bear weight as tolerated. They were also recommended to schedule regular appointments for clinical and radiological evaluations. Patient was full weight bearing post 3 months with only terminal restriction of movement at hip joint. Patient was followed up for 15 months post-implant removal and showed no complications at the last visit (Fig. 5 and 6).
This case presents a remarkable example of successful bone healing in the face of significant mechanical challenges. The Reverse Z-effect is typically associated with poor outcomes, including non-union and the need for revision surgery. However, this patient’s experience defies these expectations, suggesting that bone healing can sometimes overcome mechanical adversities.
Factors contributing to successful healing
The successful healing of the intertrochanteric fracture, despite the eventual implant failure, can be attributed to several factors working in concert. The PFN likely provided sufficient initial stability to allow for the early stages of fracture healing, supporting the formation and mineralization of the callus [5]. This stability was complemented by the rich blood supply in the intertrochanteric region, which enhanced the healing process. The patient’s overall good health and compliance with weight-bearing protocols further contributed to creating a favorable biological environment for healing. The practice of encouraging immediate weight-bearing postoperatively may have stimulated bone remodeling. In addition, patient-specific factors played a crucial role in the successful outcome [5]. The absence of significant comorbidities and the patient’s proactive engagement in rehabilitation likely positively impacted the healing process. Furthermore, individual factors such as bone quality and metabolic health significantly influenced the fracture’s ability to heal effectively, even in the face of implant failure [5].
Comparison with literature
The literature on intertrochanteric fractures and the Z-effect predominantly reports poor outcomes associated with mechanical failure of the implant [3,4]. Werner-Tutschku et al. [4] described Z-effect, which is known for its association with screw migration, implant cut-out, and non-union [4]. We were unable to find a single documented case showing successful bone union despite such complications, making this report a valuable contribution to the understanding of bone healing dynamics. These findings of mechanical failure of the implant with z effect were reproduced in laboratory by Strauss et al. [6] their finite element-based study revealed that one key component in comprehending the two screws’ separate performances was the variations in bone density at the sites where they were fixed [6]. In cases of unstable fractures, it is usual for the femoral neck to have lower bone mineral density than the femoral head, resulting in the inferior screw being prone to movement (Table 1) [6,10].

Strengths and limitations
Strengths
This case report documents a rare and successful outcome in the face of significant mechanical complications. Furthermore, it provides insights into the factors that may contribute to successful bone healing despite adverse conditions.
Limitations
This research is limited to a single instance, and the findings may not be applicable to all patients with comparable fractures and sequelae.
This case report illustrates an extraordinary instance of bone healing despite significant mechanical failure and the Reverse Z-effect. It emphasizes the importance of considering both biological and mechanical factors in the management of intertrochanteric fractures. Further research is needed to explore the underlying mechanisms that enable successful bone healing despite complications and to refine post-operative management protocols to optimize outcomes for patients with similar conditions.
This case illustrates the potential for complete bony union in intertrochanteric femur fractures despite complications, emphasizing the importance of vigilant monitoring, adaptive treatment strategies, and individualized patient care.
References
- 1.Cheng YX, Sheng X. Optimal surgical methods to treat intertrochanteric fracture: A Bayesian network meta-analysis based on 36 randomized controlled trials. J Orthop Surg Res 2020;15:402. [Google Scholar | PubMed]
- 2.Smeets SJ, Kuijt G, Van Eerten PV. Z-effect after intramedullary nailing systems for trochanteric femur fractures. Chin J Traumatol 2017;20:333-8. [Google Scholar | PubMed]
- 3.Pires RE, Santana EO Jr., Santos LE, Giordano V, Balbachevsky D, Dos Reis FB. Failure of fixation of trochanteric femur fractures: Clinical recommendations for avoiding Z-effect and reverse Z-effect type complications. Patient Saf Surg 2011;5:17. [Google Scholar | PubMed]
- 4.Werner-Tutschku W, Lajtai G, Schmiedhuber G, Lang T, Pirkl C, Orthner E. Intra-und perioperative Komplikationen bei der Stabilisierung von per-und subtrochantären Femurfrakturen mittels PFN [Intra-and perioperative complications in the stabilization of per-and subtrochanteric femoral fractures by means of PFN]. Unfallchirurg 2002;105:881-5. [Google Scholar | PubMed]
- 5.Sheen JR, Mabrouk A, Garla VV. Fracture healing overview. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551678 [Last accessed on 2023 Apr 08]. [Google Scholar | PubMed]
- 6.Strauss EJ, Kummer FJ, Koval KJ, Egol KA. The “Z-effect” phenomenon defined: A laboratory study. J Orthop Res 2007;25:1568-73. [Google Scholar | PubMed]
- 7.Brunner A, Jöckel JA, Babst R. The PFNA proximal femur nail in treatment of unstable proximal femur fractures--3 cases of postoperative perforation of the helical blade into the hip joint. J Orthop Trauma 2008;22:731-6. [Google Scholar | PubMed]
- 8.Tyllianakis M, Panagopoulos A, Papadopoulos A, Papasimos S, Mousafiris K. Treatment of extracapsular hip fractures with the proximal femoral nail (PFN): Long term results in 45 patients. Acta Orthop Belg 2004;70:444-54. [Google Scholar | PubMed]
- 9.Rethnam U, Cordell-Smith J, Kumar TM, Sinha A. Complex proximal femoral fractures in the elderly managed by reconstruction nailing-complications and outcomes: A retrospective analysis. J Trauma Manag Outcomes 2007;1:7. [Google Scholar | PubMed]
- 10.Kobayashi N, Inaba Y, Yukizawa Y, Takagawa S, Ike H, Kubota S, et al. Bone mineral density distribution in the proximal femur and its relationship to morphologic factors in progressed unilateral hip osteoarthritis. J Bone Miner Metab 2015;33:455-61. [Google Scholar | PubMed]