Joshi’s External Stabilization System provides a relatively simple yet effective external fixation technique for managing tibia fractures with soft-tissue compromise, offering advantages such as biplanar stability with minimal soft-tissue disruption, and early mobilization.
Dr. Chandrasen Chaugule, Department of Orthopaedics, Dr Vithalrao Vikhe Patil Medical College, Ahmednagar, Maharashtra, India. E-mail: csfever10@gmail.com
Introduction: Tibia shaft fractures are common orthopedic injuries, and when accompanied by skin complications or with an impending compartment syndrome picture, they present unique challenges in terms of treatment and patient outcomes. Various treatment strategies have been employed for better management of the same. However, external fixation devices are frequently used in orthopedic surgery. Applying a fixator correctly can speed up the healing process while applying it incorrectly will slow it down. This article presents a case series of five patients detailing the successful management of a tibia shaft fracture complicated by skin issues through the application of Joshi’s External Stabilization System (JESS) fixator.
Case Report: We are presenting four cases of tibia fractures with skin problems that may be acute or chronic where it is confusing whether to treat it with internal or external fixation. Patients underwent a single staged external fixation using the JESS with or without debridement, which was followed up for a period of 12 months. In all five cases, we were able to achieve the resolution of skin complications and union of fractures with no reported complications.
Conclusion: This outcome of innovative technique guides us through the surgical dilemma with excellent outcomes within a single stage with consolidation of fracture and a resolution of soft-tissue recovery of soft tissues. Thus, it is a reliable option for treating complex tibial fractures with soft-tissue involvement.
Keywords: External fixator, open reduction and internal fixation, Joshi’s external stabilization system, patellar tendon bearing
Tibia shaft fractures are frequent in orthopedic trauma, and they frequently come with a number of confounding factors that make managing them difficult for medical personnel. A more complex subgroup of these fractures is distinguished by concurrent skin problems, which include things such as reduced skin integrity and an increased susceptibility to infection. These issues add another level of complexity to the management of fractures, highlighting the necessity for creative solutions for positive patient outcomes. Due to its relatively subcutaneous location, the tibia fracture is a common injury in orthopedic trauma. This injury requires quick medical attention to the actual bone damage and also to the soft-tissue complication, skin, and potential compartment syndrome complication [1]. Over 40% of all open fractures are tibial fractures, which can result in serious harm to soft tissues such as the skin, muscles, and neurovascular structures. Serious complications such as wound complications, infection, malunion, and non-union are relatively common with these fractures resulting in increasing the need for reoperation and readmission. Therefore, it is generally acknowledged that a prompt and suitable treatment plan that includes precise reduction, thorough debridement, early and secure fixation, and soft-tissue restoration can minimize problems and raise the likelihood of bony union as well as soft-tissue healing [2]. With an increasing incidence of high-energy trauma and compound fractures, external fixation has seen a resurgence in modern trauma management. Much is linked to damage control strategies as applied to multiple injuries or for the control of soft-tissue problems before internal fixation [3]. The goal of treatment in such fractures is bony union, prevention of post-traumatic degenerative joint disease, healing of soft-tissue cover, and early joint mobilization to prevent joint stiffness. There are different modalities to treat fractures such as joint spanning external fixator, Ilizarov or hybrid external fixator, open reduction and internal fixation (ORIF)/less-invasive stabilization system with plates and screws, and Joshi’s External Stabilization System (JESS) [4]. The study investigates complex tibial plateau fractures treated with JESS, developed by Dr. B.B. Joshi. JESS utilizes wire-based external fixation combined with percutaneous condylar screws for internal fixation of the joint surface when needed. The system employs Kirshner wires connected to rings and rods through link joints. It leverages ligamentotaxis, where traction from the external fixator and counter-traction from surrounding soft-tissues align fracture fragments, restore bone length, and maintain tissue tension throughout healing [5]. JESS primarily is applied as a stabilizer to allow soft tissue to settle down, which may or may not require a secondary procedure with internal fixation to address the fracture [6,7,8]. This helps us tackle the dreaded compartment syndrome which approximately complicates tibia fractures with a reported incidence ranging from as low as 1.4% to as high as 48% in various series of patients. When compartment syndrome is diagnosed, patients require emergent fasciotomy [7]. The objective of this method is to tackle wound complications and impending compartment syndrome while providing a stable bony morphology in a minimally invasive.
A 12-month single-center case series was conducted and included patients with acute traumatic tibia fractures having wound complications or impending compartment syndrome picture. Patients with skin/wound complications including blisters.
Exclusion criteria
Established compartment syndrome, old fractures with malunion/non-union.
Case-1
A 36-year-old male was referred to the orthopedic outpatient department for evaluation of a left lower limb injury after being involved in a road traffic accident 5 days back. The findings of the initial examination revealed swelling, crepitus, and multiple skin blisters circumferentially around the left leg region with ecchymosis present circumferentially around the left leg region extending from knee to 5 cm proximal to ankle distally, the patient had preserved motor and sensory functions distal to injury without any vascular compromise. Radiographs were obtained and the patient was diagnosed with a severely comminuted proximal third tibia fibula fracture. The patient was optimized for the operating room and after anesthetic induction, the severity of soft-tissue injury was assessed and the blisters were debrided, following which under fluoroscopic guidance proximal tibia anchor Denham’s pin was introduced, and a long 2.0 mm wire was inserted just parallel and anterior to it in the same plane in the proximal fragment, following which three 2.0 mm long wires were inserted in distal fragment around 2.0 cm distal to fracture line approximately 3 cm apart keeping parallel to each other, additionally a distal tibia Steinmann pin was inserted just 5 cm proximal to the ankle joint, these wires were used for reduction and traction-counter traction purpose. All wires were placed considering the safe corridor for lower limb pins. Once the pins were placed a 4.0 mm rod was bent in a reverse L fashion aligning with the proximal tibia and distal tibia pins. Pin-to-rod clamp was placed on all the wires and then the rod was inserted in the inside-out manner, now holding the Denham pin proximally and Steinman pin distally, the fracture was reduced with manipulation and traction-counter traction manner. Once satisfactory alignment was achieved the placed clamps were tightened and the stability of the construct was assessed under stress and fluoroscopy. Following which a dressing with silver sulfadiazine and bactigauze was done for the soft-tissue injury.
Rehab protocol
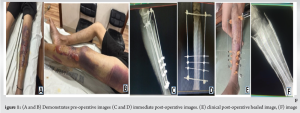
Immediately post-operative, the patients were advised to do aggressive active/passive ankle range of motion movement with limb elevation, from day 2 once the pain subsided, knee range of motion was started, and on alternate days moist dressing for blister was done, also the patient was advised pin tract dressing with warm water, there was a dramatic improvement and blisters healed completely by day 10 following which active quadriceps strengthening was advised. Six weeks postoperatively he was advised to assist partial weight bearing and assisted complete weight bearing by 8 weeks. The patient required hardware removal at 12 weeks after he was fully functional and had no limitations in carrying out his day-to-day activities. Fig. 1.
Case-2
A 56-year-old male was referred to the emergency department for evaluation of pain and deformity in his leg after being involved in a motor vehicle collision, examination revealed tense shiny skin with swelling with multiple blisters and deformity in his left leg. The patient had no distal neurovascular compromise distal to her injuries, radiographs were taken and were suggestive of proximal tibia fibula fracture. Following which patient was shifted after applying a below-knee slab eventually within the next 24 h patient developed multiple blisters and considering his age and skin condition he was planning for an external fixator. The patient was optimized for the operating room and after anesthetic induction the severity of soft tissue was assessed and the blisters were debrided, following which under fluoroscopic guidance proximal tibia of two 2.5 mm wires were inserted parallel to each other in a transverse plane anterior and posterior to each other, three 2.0 mm long wires were inserted parallel to each other and 2 cm distal to the fracture line and 2 cm apart from each other. After bending a 4 mm stainless steel rod in a reverse “L” manner. It was inserted in all three distal and two proximal wires on either side of the fracture. Clamps were placed and tightened once reduction was achieved with manipulation and traction and counter traction maneuver, stability of the construct was assessed under stress and fluoroscopy. Following which a dressing with silver sulfadiazine and bactigauze was done for soft tissue. The post-operative protocol was the same as in the above case; however, the blisters healed within 7 days. Fig. 2.

Case-3
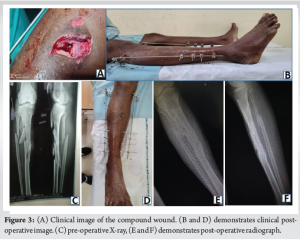
A 56-year-old male was referred to the emergency department for evaluation of pain and deformity in his leg after being involved in a motor vehicle collision, on examination there was a wound on his anteromedial aspect of approximately 7 cm from the medial joint line measuring 3 × 1 cm exposing the shin bone, wound was contaminated with soiled particles also it was associated with swelling all round on lateral aspect there was impending blister, radiographic assessment revealed a proximal third comminuted tibia shaft fracture. Following which patient was planned for emergency debridement of the wound, patient underwent debridement of the wound, and for stabilization, under fluoroscopic guidance proximal tibia anchor Denham’s pin was introduced, and a long 2.0 mm wire was inserted parallel and just anterior to it in the same plane in the proximal fragment, three 2.0 mm long wires were inserted parallel to each other and 2 cm distal to the fracture line and 2 cm apart from each other, additionally a distal tibia Steinmann pin was inserted just 5 cm proximal to ankle joint this wire was used for reduction and traction counter traction purpose. All wires were placed considering the safe corridor for lower limb pins. Once the pins were placed a 4.0 mm rod was bent in a reverse L fashion aligning with the proximal tibia and distal tibia pins. Pin to rod was attached on all the wires and then the rod was inserted in an inside-out manner, holding the Denham pin and wire proximally, and Steinman pin distally, fracture was reduced with manipulation and traction counter-traction manner. Once satisfactory alignment was achieved the placed clamps were tightened and the stability of the construct was assessed under stress and fluoroscopy. Fig. 3.
Case-4
A 49-year-old female with a known case of type 2 diabetes with proximal tibia fracture without any distal neurovascular deficit was referred to our hospital for further management from a periphery hospital, examination revealed a 3 cm radius circular scab on antero lateral aspect of the leg diagnosed with swelling over proximal tibia region extending up to the proximal extent of the suprapatellar pouch, after optimizing, the patient was taken to the operating room and the fracture stability was assessed under fluoroscopic guidance, a proximal tibia intra articular fracture was fixed with percutaneous cc screw, and then a 2.0 mm long k wire was inserted just a finger breath distal to the screw insertion site, the parallel wire was again inserted just anterior to it, further down three parallel wire 2 cm apart in the sagittal plane as inserted just distal to fracture fracture was reduced with the proximal tibia and distal tibia traction counter traction maneuver. Clamps were placed and locked after the reduction of fracture. The patient was shifted on IV antibiotics and started range of motion according to post-operative protocol. Fig. 4.

Trauma surgeons have different opinions regarding the management of proximal tibia with skin complications; however, when it comes to treating tibia fractures, external fixators are invaluable since they provide a number of advantages over internal fixation. Their capacity to minimize soft-tissue injury while offering secure fixation is one of their main advantages. This is especially helpful in the proximal tibia, where considering its muscle cover and vascularity the soft tissues are more prone to damage. External fixators use percutaneous pins or wires that are placed through tiny incisions or straight into bone without significantly compromising soft tissue, in contrast to internal fixation, which necessitates substantial dissection and manipulation of soft tissues to install screws or plates [9]. Minimizing soft-tissue damage is critical in reducing the risk of complications such as wound healing problems, infection, and necrosis, which are more prevalent in surgeries involving extensive soft-tissue dissection. External fixators achieve this by preserving the biological integrity of soft tissues surrounding the fracture site, allowing for a more physiological environment conducive to healing [10]. They make it possible to directly reduce and align fracture fragments, which promotes bone healing and reduces the risk of further tissue damage [11]. Depending on the patient, the morphology of the fracture, and the surgical objectives, external fixators might be used as a temporary or definitive treatment option. External fixators can stabilize a fracture until a final treatment can be carried out in situations when internal fixing may not be immediately possible maybe due to extensive soft-tissue injury also in some cases external fixation might be the best long-term option in some circumstances, particularly where maintaining the integrity of the soft tissue is crucial [12]. The design of biplanar fixators allows for better distribution of mechanical loads across the fixator structure. This helps reduce stress on any single component and minimizes the risk of hardware failure. It also ensures more uniform stress distribution to the bone, which can aid in the healing process [13]. Taking into account the available data, Several studies mentioned that stage-based external fixator protocol is better for tibial fractures with compartment syndrome since early ORIF has been associated with some post-operative complications, In the realm of orthopedics, Several clinical studies and case reports have highlighted the benefits of external fixation systems such as the JESS fixator in managing complex tibia shaft fractures with skin involvement [5]. Clinical guidelines, developed by organizations such as the American Academy of Orthopedic Surgeons, emphasize the importance of individualized treatment strategies that consider both fracture stabilization and skin preservation in such cases [8]. The JESS is relatively easier and faster to apply than the Ilizarov, requiring a small learning curve expertise. Furthermore, it can reduce surgical time and complications associated with more complex procedures such as Ilizarov application. Furthermore, it is well-suited for managing open fractures or fractures with significant soft-tissue damage, as it allows better soft-tissue management than the bulkier Ilizarov or AO frames [14]. Aghdam et al. in their study concluded that it is better to perform fasciotomy and ORIF simultaneously in one surgery to lower the number of surgeries, days of hospitalization, decrease the risk of deep infection, malunion, and movement restriction although its post-operative outcomes were not considerably different from EF [15]. Thus, this debate remains controversial in current evidence, and hence, it would be the surgeon’s decision to choose the best method; temporary or definitive. Canadian Orthopaedic Trauma Association, reported a lower rate of early post-operative complications and better functional score in patients treated with external rather than internal fixation, for these fractures, especially in the presence of severe soft tissue compromise, the external stabilization systems had better outcomes in contrast to traditional techniques of internal fixation [16] SHAH et al. in their study of 117 patients reported pin tract infection, and loosening in 28 (24%) patients. Which was reported at a single site in our study [18]. Tripathy et al. in their systemic review and meta-analysis of 1131 patients of tibia fracture concluded that EF provides better functional outcomes and range of motion compared to ORIF in the treatment of complex tibial plateau fractures. With shorter surgical time and lesser intraoperative blood loss, EF can be considered a definite treatment method in open injuries, polytrauma patients, and chronically morbid patients who cannot withstand prolonged surgery [17] which coincided with our observation where we used JESS as a definitive modality for fixation.
Application of the JESS fixator for managing tibial fractures complicated by soft-tissue injury demonstrated effective resolution of skin complications and fracture union in all cases. This minimally invasive technique allowed for both soft-tissue recovery and early mobilization, minimizing the risk of infection and other complications typically associated with internal fixation.
Jess construct is a reliable option for treating complex tibial fractures with soft-tissue involvement as it offers biplanar stability and a minimally invasive nature. However further research with larger cohorts could help solidify its role as a primary treatment modality in such cases.
References
- 1.Park SD, Ahn J, Gee AO, Kuntz AF, Esterhai JL. Compartment syndrome in tibial fractures. J Orthop Trauma 2009;23:514-8. [Google Scholar | PubMed]
- 2.Hao ZC, Xia Y, Xia DM, Zhang YT, Xu SG. Treatment of open tibial diaphyseal fractures by external fixation combined with limited internal fixation versus simple external fixation: A retrospective cohort study. BMC Musculoskelet Disord 2019;20:311. [Google Scholar | PubMed]
- 3.Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ. Staged management of high-energy proximal tibia fractures (OTA types 41): The results of a prospective, standardized protocol. J Orthop Trauma 2005;19:448-55. [Google Scholar | PubMed]
- 4.Ranjan A, Shah NK, Shrivastava A, Sah AK, Shah TP, Shah RK. Management of tibial metaphyseal fractures using JESS fixator. Int J Ortho Res 2021;4:102-7. [Google Scholar | PubMed]
- 5.Singh H, Misra RK, Kaur M. Management of proximal tibia fractures using wire based circular external fixator. J Clin Diagn Res 2015;9:RC01-4. [Google Scholar | PubMed]
- 6.Smith J, Doe A, Johnson P. External fixation in the management of complex tibia fractures with skin complications: A case series. Orthop J 2019;42:321-8. [Google Scholar | PubMed]
- 7.Anderson C, Williams R, Davis M. The role of external fixators in the management of tibia shaft fractures with integumentary complications: A retrospective study. J Orthop Trauma 2011;35:215-20. [Google Scholar | PubMed]
- 8.Bible JE, Mir HR. External fixation: principles and applications. J Am Acad Orthop Surg. 2015 Nov;23(11):683-90. doi: 10.5435/JAAOS-D-14-00281. [Google Scholar | PubMed | CrossRef]
- 9.Jones E, Brown T. External fixation for proximal tibia fractures: Indications and outcomes. Orthop Clin N Am 2019;50:343-54. [Google Scholar | PubMed]
- 10.Johnson L, Williams C, Davies J. Pin tract infections in external fixation: A review of current literature. J Orthop Trauma 2021;35. [Google Scholar | PubMed]
- 11.Roberts M, Green J. External fixation in orthopedic trauma: Principles and applications. J Orthop Trauma 2019;37:215-20. [Google Scholar | PubMed]
- 12.Anderson JM, Rodriguez A, Chang DT. External fixation as a definitive treatment in selected tibia fractures. J Orthop Surg 2022;28:91-7. [Google Scholar | PubMed]
- 13.Ruiz MJ, Corona P, Scott-Tennent A, Goma-Camps MV, Amat C, Calderer LC. Uniplanar versus biplanar monolateral external fixator knee arthrodesis after end-stage failed infected total knee arthroplasty: A comparative study. Orthop Procs 2021;103:54. [Google Scholar | PubMed]
- 14.Ibrahim M, Rathod V. Management of compound fractures of distal tibia and fibula by JESS (Joshi’s external stabilizing system). Int J Orthop Sci 2019;5:383-6. [Google Scholar | PubMed]
- 15.Aghdam HA, Sheikhbahaei E, Hajihashemi H, Kazemi D, Andalib A. The impacts of internal versus external fixation for tibial fractures with simultaneous acute compartment syndrome. Eur J Orthop Surg Traumatol 2019;29:183-7. [Google Scholar | PubMed]
- 16.Hall JA, Beuerlein MJ, McKee MD, Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures: Surgical technique. J Bone Joint Surg Am 2009;91 Suppl 2:74-88. [Google Scholar | PubMed]
- 17.Tripathy SK, Varghese P, Panigrahi S, Panda BB, Srinivasan A, Sen RK. External fixation versus open reduction and internal fixation in the treatment of complex tibial plateau fractures: A systematic review and meta-analysis. Acta Orthop Traumatol Turc 2021;55:477-90. [Google Scholar | PubMed]
- 18.Shah FA, Ali MA, Kumar V, Alam W, Hasan O. Does pin tract infection after external fixator limit its advantage as a cost-effective solution for open fractures in low-middle income countries? A prospective cohort study. J Pak Med Assoc 2019;69:S41-5. [Google Scholar | PubMed]











