Early diagnosis and timely imaging are crucial in preventing chronicity in anterior shoulder dislocations, with the Latarjet procedure proving effective for restoring stability and function in cases with significant bone loss.
Dr. Ibad Shah, Consultant Orthopaedic Surgeon, Department of Orthopaedic Surgery, The Lifeline Multi Speciality Hospital, Kerala, India, E-mail: ibadshah47@gmail.com
Introduction: Neglected anterior shoulder dislocations are rare and present significant diagnostic and therapeutic challenges due to progressive anatomical changes over time. Chronic cases often involve joint instability, bone erosion, and soft-tissue contractures, requiring complex surgical management.
Case Report: We present the case of a 45-year-old male with a 6-month-old neglected anterior shoulder dislocation, initially misdiagnosed, and unsuccessfully managed with a closed reduction. Imaging revealed a significant Hill-Sachs lesion and minimal glenoid bone loss. Open reduction with the Latarjet procedure was performed through a deltopectoral approach to restore joint stability. Postoperatively, the patient showed substantial functional improvement with forward flexion of 150° at 6 months and minimal complications.
Conclusion: This case highlights the importance of early diagnosis and intervention in shoulder dislocations to prevent chronicity and the need for complex surgical procedures. The Latarjet procedure proved effective in managing chronic dislocations with significant bone loss, providing reliable stabilization and functional recovery. Early imaging and individualized treatment planning are crucial for optimizing patient outcomes.
Keywords: latarget, Neglecked dislocation, locked shoulder dislocation
Neglected anterior shoulder dislocations are rare, accounting for approximately 0.12–0.18% of all shoulder dislocations [1]. These cases present significant challenges in diagnosis and treatment due to the complex anatomical changes that occur over time. Extensive surgical intervention is often required, as joint damage, bone loss, and soft tissue contractures can develop if left untreated [2]. Chronic anterior shoulder dislocations are also associated with significant morbidity, including pain, limited range of motion, and progressive osteoarthritis, which complicates treatment and affects patient outcomes [2,3]. The absence of an established treatment protocol for neglected dislocations further complicates management, and each case demands an individualized approach based on patient-specific factors, such as bone loss and soft-tissue involvement. This report presents a case of a 45-year-old male who sustained a right shoulder injury following a fall from a bike, leading to a neglected anterior dislocation that required surgical management with an open reduction and Latarjet procedure. The case highlights the importance of early diagnosis, appropriate imaging, and individualized treatment planning for achieving optimal outcomes in neglected shoulder dislocations.
A 45-year-old right-handed male presented to our orthopedic center with complaints of persistent pain and limited range of motion in his right shoulder. The symptoms began following a fall from his bike 6 months prior. At the time of the accident, he was evaluated at an outside hospital where no imaging studies were performed, and the injury was initially misdiagnosed. The patient was discharged with analgesics and advised conservative management. Despite ongoing pain and restricted function, the patient continued with his daily activities, although with significant limitations. Approximately 5 months post-injury, the patient sought evaluation at another hospital due to worsening pain and increasing stiffness in the shoulder. Imaging, including an X-ray, revealed an anterior dislocation of the right shoulder. Closed reduction was attempted at that facility, but it was unsuccessful. Consequently, the patient was referred to our institution for further evaluation and management. On examination at our center, the patient exhibited a marked reduction in both active and passive shoulder movements, with considerable pain on attempted movement. Physical examination revealed a prominent acromion and anterior bulging, consistent with an anterior shoulder dislocation. No neurovascular deficits were detected on examination, and the patient had intact sensation and motor function throughout the right upper limb.
Investigations
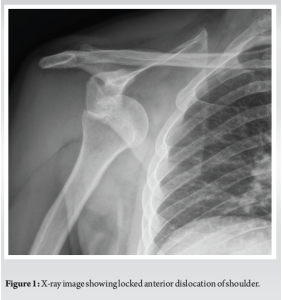
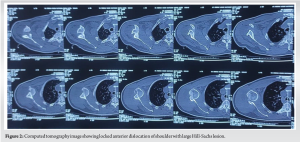
Initial radiographs confirmed an anterior dislocation of the right shoulder (Fig. 1). To further assess the extent of bone and joint damage, a computed tomography (CT) scan was performed (Fig. 2). The CT revealed a severely eroded posterior humeral head (Hill-Sachs lesion) and minimal glenoid bone loss. These findings indicated chronic dislocation with substantial bone damage, contributing to the failure of the closed reduction attempt.
Management
Due to the chronic nature of the dislocation, significant bone loss, and intraoperative instability risk, it was decided to proceed with open surgical intervention. The patient underwent open reduction with the Latarjet procedure, which involved transferring the coracoid process with its attached muscles to the anterior glenoid to enhance stability.
The operation was performed with the patient in the beach-chair position using a deltopectoral approach. The deltopectoral groove and the cephalic vein were identified, followed by transection of the coracoacromial ligament 1.5 cm from its insertion at the coracoid. The pectoralis minor was then released from the coracoid, and the conjoint tendon was carefully individualized. An osteotomy of the coracoid process was performed at the vertical and horizontal junction. The subscapularis muscle was split at the junction between the upper two-thirds and lower one-third, followed by a capsulotomy to access the joint. On exploration, an anteromedial dislocation of the humeral head was confirmed, with significant wear of the humeral head. Fibrotic tissue was removed, and the dislocation was reduced. The Latarjet procedure was then performed, with the coracoid graft placed and fixed to the anteroinferior border of the glenoid using two 4 mm partially threaded cannulated cancellous screws. Post-operative radiographs showed a good position of the bone block with a reduced shoulder joint (Fig. 3).

Post-operative management
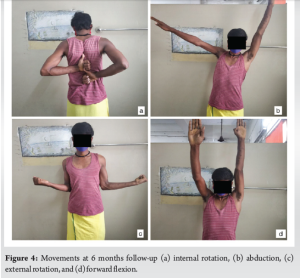
Postoperatively, the patient’s right shoulder was immobilized in a sling for 4 weeks to facilitate healing of the transferred coracoid and to maintain joint stability. Physiotherapy was initiated after 4 weeks, starting with a passive range of motion exercises to gradually improve shoulder mobility while minimizing stress on the surgical site. Active-assisted and active range of motion exercises were introduced progressively, followed by strengthening exercises focused on the rotator cuff and scapular stabilizers. The rehabilitation process was carefully monitored to avoid overloading the joint during the early healing phase. At the 6-month follow-up, the patient demonstrated substantial improvement in shoulder function, with significant reduction in pain levels. He was able to achieve forward flexion of up to 150°, although external rotation remained limited to 20° (Fig. 4). Follow-up radiographs showed stable incorporation of the coracoid graft and maintenance of joint congruity without signs of recurrent dislocation.
This case highlights the challenges associated with neglected anterior shoulder dislocations and underscores the importance of early diagnosis and intervention. In this patient, the initial lack of imaging and subsequent misdiagnosis at the outside hospital resulted in a missed opportunity for the early reduction, allowing the dislocation to become chronic. Chronic anterior dislocations are associated with progressive bone erosion, joint capsule contracture, and damage to the surrounding structures, all of which complicate eventual treatment and can lead to poor outcomes if not managed appropriately [4]. Recurrent instability may result from the bone defect, depending on the size and depth of the defect. In cases where the bone defect comprises more than 40–50% of the humeral head, rotational osteotomy of the proximal humerus or partial/complete humeral head replacement is recommended [5]. For defects >25% but <40%, the Latarjet procedure and non-anatomic procedures such as bone or soft-tissue transfer (remplissage) of the infraspinatus are recommended [6]. These techniques may include allograft repair of the head and humeral head disimpaction/humeroplasty, depending on the extent of damage. The Latarjet procedure, which provides bony augmentation, dynamic stabilization, and capsular support, is generally preferred for defects >25% due to its efficacy in preventing recurrent dislocations [7]. The Latarjet procedure is validated for its ability to treat recurrent anterior shoulder dislocations with or without significant glenoid bone defects, as evidenced by outcomes reported in the literature [6,7]. Lubis et al. reported a case of a 27-year-old patient with a 10-month-old anterior shoulder dislocation successfully managed with open reduction and the Latarjet procedure, achieving a 95% success rate in preventing recurrence and a significant improvement in range of motion [8]. Similarly, Abdulahi et al. documented satisfactory outcomes in a 56-year-old patient with a 5-month-old dislocation, noting stable incorporation of the coracoid graft and restored joint stability [9]. Despite the high success rates, there is also a risk of complications, including a 5% recurrence rate, loss of external and internal rotation, and the onset of glenohumeral osteoarthritis [10]. Latarjet procedure has been shown to be effective in cases of recurrent anterior dislocation with large glenoid osseous defects, which may justify its use for treating neglected anterior shoulder dislocations. The transfer of the osteotomized coracoid process into the glenoid rim, initially described by Latarjet in 1958, reconstructs the depth and width of the glenoid [11]. The procedure also enhances dynamic reinforcement of the inferior part of the capsule through the coracobrachialis muscle, which is particularly effective when the arm is abducted and externally rotated [3,6,8]. Compared to the Bristow procedure, the Latarjet procedure is generally preferred for glenoid bone loss >20–25%, as it offers greater stability due to the “triple effect” of the bone block, capsular repair, and dynamic sling [12]. The current case demonstrates the successful use of the Latarjet procedure to address large Hill-Sachs lesion with minimal glenoid bone loss and chronic instability. Soft-tissue imbalance is another risk factor for post-operative redislocation or subluxation, particularly in patients with neglected dislocations where long-term dislocation may lead to muscle lengthening and biomechanical imbalances. Post-operative complications, such as osteoarthritis, can also occur due to avascular necrosis of the humeral head, with factors such as age at first dislocation, time of surgery, and preexisting arthritis contributing to the risk.
Neglected anterior shoulder dislocations are complex injuries that require a high index of suspicion for accurate diagnosis, particularly in patients presenting with shoulder pain following trauma. Early imaging and appropriate intervention are essential to prevent the progression to a chronic state, which necessitates more complex surgical intervention. In this case, delayed diagnosis led to significant bone loss and chronic dislocation, requiring open reduction and a coracoid transfer using the Latarjet procedure. This approach provided satisfactory functional outcomes, with the patient regaining significant shoulder mobility and stability. The Latarjet procedure remains a reliable option for managing chronic dislocations with associated bone loss, offering both static and dynamic stabilization.
- Timely imaging is essential in evaluating shoulder injuries to prevent missed dislocations.
- Chronic shoulder dislocations often present with significant bone loss and joint contracture, complicating management.
- The Latarjet procedure is effective in treating chronic anterior shoulder dislocations with bone deficiency, providing both static and dynamic stabilization of the joint.
- Early and appropriate intervention is crucial in preventing the need for complex surgical procedures and ensuring better functional outcomes.
References
- 1.Rai AK, Bandebuche AR, Bansal D, Gupta D, Naidu A. Chronic unreduced anterior shoulder dislocation managed by latarjet procedure: A prospective study. Cureus 2022;14:e21769. [Google Scholar | PubMed]
- 2.Bauer S, Collin P, Zumstein MA, Neyton L, Blakeney WG. Current concepts in chronic traumatic anterior shoulder instability. EFORT Open Rev 2023;8:468-81. [Google Scholar | PubMed]
- 3.Werthel JD, Sabatier V, Schoch B, Amsallem L, Nourissat G, Valenti P, et al. Outcomes of the latarjet procedure for the treatment of chronic anterior shoulder instability: Patients with prior arthroscopic bankart repair versus primary cases. Am J Sports Med 2020;48:27-32. Erratum in: Am J Sports Med 2020;48:NP33. [Google Scholar | PubMed]
- 4.Chung H, Yoon YS, Shin JS, Shin JJ, Kim D. Chronic irreducible anterior dislocation of the shoulder without significant functional deficit. Clin Orthop Surg 2016;8:333-8. [Google Scholar | PubMed]
- 5.Valencia Mora M, Ruiz-Ibán MÁ, Heredia JD, Ruiz Díaz R, Cuéllar R. Management of humeral defects in anterior shoulder instability. Open Orthop J 2017;11:1011-22. [Google Scholar | PubMed]
- 6.Chaudhary D, Joshi D, Jain V, Mohindra M, Mehta N. A six months old neglected anterior shoulder dislocation managed by closed reduction and Latarjet procedure. Chin J Traumatol 2016;19:295-7. [Google Scholar | PubMed]
- 7.Wang L, He S, Wu X, Lv X, Wang T, Tan H. Efficacy and safety of the latarjet procedure for the treatment of athletes with glenoid bone defects ≥ 20%: A single-arm meta-analysis. J Orthop Surg Res 2024;19:159. [Google Scholar | PubMed]
- 8.Lubis AM, Primaputra MR, Dilogo IH. A case report of ten-month-neglected anterior shoulder dislocation managed by open reduction combined with latarjet procedure. Int J Surg Case Rep 2019;57:93-6. [Google Scholar | PubMed]
- 9.Abdulahi M, Ali AO, Said AI, Walhad H, Elmi HS. 5 months old neglected anterior shoulder dislocation treated with open reduction and laterjet procedure: A case report. Int J Surg Case Rep 2024;124:110402. [Google Scholar | PubMed]
- 10.Kee YM, Kim HJ, Kim JY, Rhee YG. Glenohumeral arthritis after latarjet procedure: Progression and it’s clinical significance. J Orthop Sci 2017;22:846-51. [Google Scholar | PubMed]
- 11.Bradley H, Lacheta L, Goldenberg BT, Rosenberg SI, Provencher MT, Millett PJ. Latarjet procedure for the treatment of anterior glenohumeral instability in the athlete - key considerations for rehabilitation. Int J Sports Phys Ther 2021;16:259-69. [Google Scholar | PubMed]
- 12.Domos P, Lunini E, Walch G. Contraindications and complications of the latarjet procedure. Shoulder Elbow 2018;10:15-24. [Google Scholar | PubMed]







