Lateral condyle fracture of humerus in adults should not be treated as a trivial case. This injury can be a tip of the iceberg as seen in complex fracture dislocation of the elbow.
Dr. Ganesh R Shetty, Department of Orthopaedics, Dr. Muthus Hospital, Singanallur, Coimbatore, Tamil Nadu, India. E-mail: drgs701@hotmail.com
Introduction: Lateral condyle fracture with elbow instability is a rare injury. To our knowledge, this is the second case report describing the mechanism of injury and its management.
Case Report: We report the case of 42-year-old gentleman sustained injury to elbow following slip and fall. He presented to us after 2 weeks of injury diagnosed to have lateral condyle fracture of humerus managed conservatively with elbow instability which was missed initially. On further evaluation, he was found to have type 1 coronoid avulsion injury. Intraoperatively, we found that the capsular avulsion injury from coronoid was the primary reason for instability. We have tried to describe the possible mechanism of injury and management in this case report.
Conclusion: Lateral condyle fracture in adults is a rare injury which can disguise the more complex trauma associated with fracture dislocation of elbow. Proper preoperative evaluation with intraoperative assessment of elbow instability is crucial for obtaining good outcome.
Keywords: Lateral condyle fracture, complex elbow dislocation, elbow instability, terrible triad.
Elbow dislocation is the second most common major joint dislocation encountered in the casualty [1]. Complex elbow dislocation is associated with bony injury along with capsuloligamentous structures. Lateral ulnar collateral ligament (LUCL) complex is commonly injured ligamentous structure along with radial head and coronoid and proximal ulna fracture depending on the mechanism of injury [2]. Fracture of the lateral condyle of the humerus with elbow dislocation is commonly seen in children but is rare injury in adults [3]. Complex elbow dislocation involving the lateral condyle and coronoid tip avulsion fracture is uncommon injury pattern not frequently encountered with few case studies describing this injury. We describe a case report of this rare injury pattern, possible explanation of mechanism of injury and its surgical management.
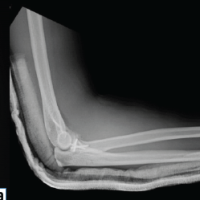
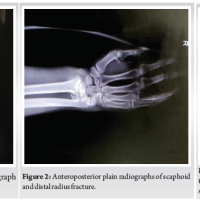
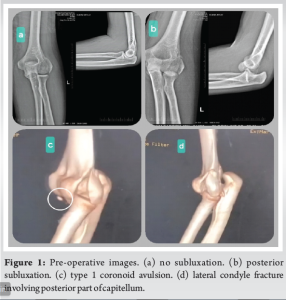
We report a case of 42-year-old gentleman with a history of slip and fall who sustained injury to left elbow. He was diagnosed to have lateral condyle fracture and was treated elsewhere with above elbow pop slab. After 2 weeks, slab was removed, and the elbow was mobilized. There was posterior subluxation of the elbow when extended beyond 70 degrees of flexion. He presented to us after 2 weeks of injury with lateral condyle fracture with elbow instability. There was no contusion/ecchymosis over the medial aspect of the elbow. Neurovascular examination was normal. Computed tomography (CT) scan with 3D reconstruction of the elbow was done which revealed minute bone fragments in front of the distal humerus anterior to coronoid which indicated type 1 (O’Driscoll) avulsion fracture of the coronoid. Lateral condyle fracture was seen involving the posterior half of the condyle (Fig. 1). No other bony injuries were seen.
Planning
In the absence of radial head/neck fracture with intact trochlea and sigmoid notch, we presumed that the elbow instability was due to the LUCL insufficiency caused by the lateral condyle fracture. The coronoid avulsion injury is inconsequential to the elbow stability. We planned for open reduction and internal fixation of the lateral condyle fracture. The lateral condyle fracture was extending in a coronal plane; hence, we decided to expose the lateral condyle through lateral paratricipital approach and fixation with posterolateral distal humerus plate.
Technique
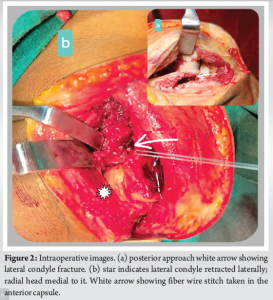
Under regional block lateral position, midline skin incision is given. Lateral paratricipital approach posterior aspect of lateral condyle exposed. Lateral condyle fracture site exposed and debrided. LUCL was found to be attached with the lateral condyle. Lateral condyle fragment was anatomically reduced and provisionally held with multiple k wires. Elbow range of motion and stability was checked to our surprise still posterior subluxation was present when elbow was extended beyond 70° to further extension. As all other structures were intact, we went ahead with the anterior capsule repair (Fig. 2). The lateral condyle fracture site was used to expose the anterior capsule. Number 2 fiber wire was used to anchor the anterior capsule which was passed through the coronoid exiting dorsally. The anterior capsule fixed through suture lasso pull out technique through two drill hole tunnels and tied over the dorsal surface of ulna. The lateral condyle was fixed with k wires, stability was checked, and the elbow was found to be stable through the range of motion. Lateral condyle was fixed with 4 mm cancellous screw and posterolateral distal humerus plate (Fig. 3).

Postoperatively, above elbow splint was given. After 5 days, elbow range of motion was started with hinged brace allowing full flexion and gradually increasing the extension over 4 weeks. At 5 weeks, full range of motion was achieved, and brace was discarded. At 1-year follow-up, patient had full range of motion (Fig. 4).

Mechanism of simple and complex fracture dislocation is determined by the direction of force, rate of application, and quality of bone. Simple dislocation of which posterolateral dislocation is the most common is supported by the valgus hyperextension theory. In which medial collateral ligament (MCL) fails first followed by LUCL. If the deforming force progresses, injury to the common flexor origin is followed by the disruption of common extensor origin [4]. Simple posteromedial dislocation accounts for 10% of all elbow dislocation follows a valgus external rotation mechanism. O’Driscoll [5] described it as a sequential injury of the soft tissues from lateral to medial as “Horii circle.” This can also result in fracture dislocation. Complex fracture dislocation with osseous injuries is associated with characteristic soft tissue injuries which contributes to instability. Based on the mechanism of injury, they are broadly classified into three types.
- Type 1: Posterolateral rotatory injury (PLRI) caused by valgus external rotation mechanism. Structures injured are LUCL, radial head, and anterolateral facet of coronoid also called terrible triad injury.
- Type 2: Posteromedial rotatory injury (PMRI) caused by varus internal rotation mechanism. Structures injured are LUCL, anteromedial facet of the coronoid and posterior band of MCL.
- Type 3: Monteggia type or trans-olecranon type fracture dislocation due to axial loading mechanism [6].
Fracture dislocation of the humoral condyle is a very rare injury in adults (1). Very few studies have mentioned this combination of injury. Aksu et al. mentioned eight cases of elbow dislocation with coronoid fracture of which one patient has lateral epicondyle fracture [7]. Lee et al. in his radiological study of CT and magnetic resonance imaging (MRI) scans of posterolateral elbow dislocation, in 54 complex elbow dislocation cases, eight patients had lateral epicondyle fractures; however, the study does not mention the combination of lateral epicondyle and coronoid fracture [8]. Fallah et al. (2022) described a case report of adult male patient with rare combination of this injury where lateral condyle was fixed with screws following which there was persistent instability of the elbow like our case. They went ahead with the extensor digitorum communis split approach to fix the anterior capsule to the coronoid restoring stability to the elbow resulting in an excellent outcome [9]. The mechanism of injury postulated in this paper is a combination of PLRI with some elements of PMRI. Due to the paucity of literature describing this type of complex fracture dislocation, the exact mechanism of injury and treatment protocol is not available. [10]. In their study terrible triad injury of elbow, which is type C of Wrightington classification, MRI studies revealed posterior capitellum contusion secondary to impaction of radial head or avulsion of the LUCL. Like this in our case, the fracture of the lateral condyle involves the posterior half of capitellum. As per these findings, we conclude that the mechanism of injury is similar to that of terrible triad injury, PLRI where the lateral column, i.e., the radial head which is the primary valgus restraint impacts the posterior part of capitellum and along with the LUCL avulsion force, lateral condyle is fractured involving the posterior half of capitellum with coronoid tip avulsion injury. Fixation of the coronoid tip avulsion in terrible triad injury is still debated. Many authors have shown no significant difference in clinical outcome in fixation and non-fixation group in terrible triad injuries of elbow when LUCL and lateral column are fixed [11,12,13]. Contrary to this in our case with the radial head intact and provisionally fixing the lateral condyle, the elbow was still unstable. After fixing the anterior capsule to the coronoid, the elbow was completely stable. This being a single case report large series study is needed to confirm these findings in this pattern of complex elbow fracture dislocation.
Lateral condyle fracture of the distal humerus is a rare injury in adults. This fracture may be associated with elbow instability which can be missed in the initial X-rays. Since the radial head and the medial column of the elbow are intact, injury to the anterior capsular structure can be overlooked. Lateral condyle fracture should be considered as LUCL avulsion injury and should be evaluated to rule out instability and injury to the coronoid and anterior capsule. These injuries should be treated similarly to terrible triad injury of the elbow.
Lateral condyle fracture with elbow instability is a rare injury where the mechanism of injury and treatment protocol are not well defined. Based on our understanding and review of literature, this injury is caused by PLRI similar to the mechanism seen in terrible triad. In the presence of elbow instability, the lateral condyle fracture site should be used to address the anterior coronoid tip avulsion which is much easier as compared to a lateral approach with intact radial head, followed by fixation of the lateral condyle. Early protected active range of motion should be initiated for excellent outcome.
References
- 1.Sanjay A, Vijayvargiya M. Lateral condyle fracture dislocation of the elbow joint in an adult: A Rare case report. J Orthop Bone Disord 2018;2:000158. [Google Scholar | PubMed]
- 2.Bentounsi A. Fracture-dislocation of the humeral condyles in adults: Results of surgical treatment. Acta Orthop Belg 2015;81:493-500. [Google Scholar | PubMed]
- 3.Valencia M, Barco R, Antuña SA. Elbow instability secondary to lateral epicondylar nounion in an adult. J Orthop Traumatol 2013;14:311-4. [Google Scholar | PubMed]
- 4.Schreiber JJ, Warren RF, Hotchkiss RN, Daluiski A. An online video investigation into the mechanism of elbow dislocation. J Hand Surg Am 2013;38:488-94. [Google Scholar | PubMed]
- 5.O’Driscoll SW. Elbow instability. Acta Orthop Belg 1999;65:404-15. [Google Scholar | PubMed]
- 6.Singh J, Elvey MH, Hamoodi Z, Watts AC. Current perspectives on elbow dislocation and instability. Ann Joint 2021;6:10. [Google Scholar | PubMed]
- 7.Aksu N, Korkmaz MF, Göğüş A, Kara AN, Işiklar ZU. Surgical treatment of elbow dislocations accompanied by coronoid fractures. Acta Orthop Traumatol Turc 2008;42:258-64. [Google Scholar | PubMed]
- 8.Lee SH, Nam DJ, Yu HK, Kim JW. The lateral ligament is injured preferentially in posterolateral dislocation of the elbow joint. Bone Joint J 2020;102-B:227-31. [Google Scholar | PubMed]
- 9.Fallah Y, Baghianimoghadam B, Daneshi SA. Elbow dislocation with lateral condyle and coronoid fractures. Case Reports Plast Surg Hand Surg 2022;9:185-8. [Google Scholar | PubMed]
- 10.Al-Ani Z, Wright A, Ricks M, Watts AC. The three-column concept of elbow joint stability and the Wrightington elbow fracture-dislocation classification, emphasizing the role of cross-sectional imaging. Emerg Radiol 2022;29:133-45. [Google Scholar | PubMed]
- 11.Ahn YS, Woo SH, Kim S, Lim JH, An TH, Kim MS. Does the coronoid fracture in terrible triad injury always need to be fixed? BMC Surg 2024;24:125. [Google Scholar | PubMed]
- 12.De Klerk HH, Ring D, Boerboom L, van den Bekerom MPJ, Doornberg JN. Coronoid fractures and traumatic elbow instability. JSES Int 2023;7:2587-93. [Google Scholar | PubMed]
- 13.Kim BS, Kim DH, Byun SH, Cho CH. Does the coronoid always need to be fixed in terrible triad injuries of the elbow? Mid-term postoperative outcomes following a standardized protocol. J Clin Med 2020;9:3500. [Google Scholar | PubMed]