The aim of reporting this case is to convey the message that genu valgum may not always be due to distal femoral deformity.
Dr. Mayank Rajput, Section Hospital, Pathankot, Punjab 145001, India. E-mail: mayank_rajput52@outlook.com
Introduction: The term “Genu valgus” originates from the Latin “Genu” meaning Knee and “valgus” is bent outward; referring to an outward angular deformity in the knee joint which is commonly seen in children. In Genu Valgus, there is lateral deviation of the mechanical axis of the lower limb which leads to an abnormal loading force significantly affecting knee movements and maltracking of the patella. Genu valgus (femorotibial alignment) of more than 12° above 8 years of age is considered pathological and needs correction.
Case Report: We report a case of a 17-year-old skeletally matured male who presented with progressive deformity in bilateral knees of 6 years duration with complaints of difficulty in walking, running, and worsening knee pain. After careful assessment, investigations, and pre-operative planning, the patient was found to have an isolated bilateral tibial origin valgus deformity with no femoral contribution to the valgus deformity; which is very rare. An individual was managed with a serial Single-level Proximal Medial Closed Wedge Osteotomy of both sides at an interval of 3 months with good correction of the deformity. At the final follow-up, the patient reported a good functional result following the corrective osteotomy.
Conclusion: A Single Level Proximal Medial Tibial Closed Wedge Osteotomy is a safe and appropriate strategy to manage the rare cases of idiopathic bilateral genu valgum with tibia valga in the absence of any femoral component. Genu valgum may not always be due to distal femoral deformity.
Keywords: Osteotomy, tibia valga, single level osteotomy, closed wedge osteotomy, bilateral genu valgum, isolated tibial angulation deformity.
Genu valgum, commonly known as knock-knees, is a condition characterized by outward deviation of legs resulting in medial angulation at the knee which is commonly seen in children [1]. In a growing child, the coronal alignment of the knee passes through various stages of alignment, which change according to the age of the child. At birth, it is genu varum with internal tibial torsion which aligns to a neutral axis by the 18th month to the 24th month. At 5 years, the knee further drifts into valgus of about 12° which spontaneously corrects by the age of 7 years to the normal adult value of approximately 7–8° [2]. As the child attains 7 years of age, correction of excessive physiologic genu valgum may be warranted [3]. The mechanical axis of the lower limb passes through the middle of the knee joint, from the femoral head to the midway point of the talus dome [1]. Lateral displacement of the mechanical axis relative to the midpoint of the knee joint results in deformities, such as genu valgus [4]. Persistence of genu valgum in adolescents results in abnormal gait and functional disturbances, such as difficulty in running, patellar malalignment, knee discomfort, pain, lateral patellar instability, and ligamentous instability [5]. Genu valgum usually originates from the distal femur, which may be confirmed by various angle measurements on standing radiographs of both lower limbs [6]. Tibia valga following proximal tibial metaphyseal injury (Cozen’s phenomenon) is a common cause of genu valgum in children [7] but our patient; first, presented with no history of previous trauma, second, the deformity being bilateral is unlikely to be of traumatic etiology. Our case presented with an idiopathic deformity localized to the proximal tibia only resulting in genu valgum of both knees and thus needed a Bilateral Single Level Proximal Medial Tibial Closed Wedge Osteotomy with successful correction of the abnormalities in both legs and a good functional result.
We report a case of a 17-year-old male nearing skeletal maturity who presented with progressive deformity in bilateral knees for 6 years with complaints of difficulty in walking, running, and worsening knee pain limiting activity for the past couple of years. On careful history taking, any associated congenital malformations were ruled out and clinical examination revealed an unusual gait and bilateral valgus deformity which was not obliterated on knee flexion suggesting a tibial component. No tenderness could be elicited over both knee joints and patellar tracking was normal. All ligaments around the knees were intact with no laxity. The patient’s past and present medical history and family history were unremarkable. The patient was desirous of being free from deformity and consented for further treatment in the form of corrective surgery. He underwent specific pre-operative radiological investigations (Fig. 1-5), which a standing bilateral lower limb scanogram for exact measurement of deformity. The pre-operative clinical picture is shown in Fig. 6.

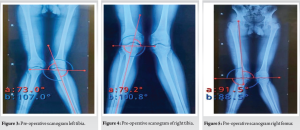

The medial proximal tibial angle (MPTA) in the worse affected left knee was 107° instead of 87° suggestive of an almost 20° of deviation from the normal whereas lateral distal femoral angle (LDFA) measured 84.4° which is almost normal. On the right side, the MPTA and LDFA were 100.8° and 88.5° suggestive of an overall deformity of 14° on the tibial side. Overall mechanical alignment on the right was 194° and on the left measured to be 200° against the normal mean of 180 with a deviation of 3° (177–193°) suggestive of gross valgus deformity on both sides with left worse than the right knee.
The precise measurements led to the conclusion that the knee deformity on both sides were purely of tibial origin and hence corrective surgery at one level can lead to the resolution of the deformity. Hence it was decided to do perform a single-level closing wedge osteotomy at the level of the proximal tibia. The left side being worse was chosen first. The length of the bony wedge to be removed to achieve correction was calculated before surgery (9 mm) using computer software. The goal was to achieve neutral to slight valgus alignment and to avoid varus alignment. Furthermore, the patient was counseled regarding the procedure of corrective osteotomy and the associated complications related to anesthesia and surgery. A written and informed consent was obtained from the patient and the surgery on the left knee was scheduled.
Surgical procedure
The Goals of correction were to restore the mechanical axis of the bilateral lower limb while maintaining knee joint line obliquity and to achieve single-stage correction without neurovascular injury. A Closing wedge osteotomy was chosen over an opening wedge due to better biomechanical stability and the prospect of allowing early weight-bearing post-operative. After giving Spinal Anesthesia, the patient was placed in a supine position with a high thigh tourniquet. After painting and draping, an incision over the lateral aspect of the knee was given to explore the common perineal nerve and to release it from surrounding tissues. This was done to avoid nerve injury due to traction once such a large deformity is corrected. Afterward, a 7 cm incision was taken over the medial tibia surface. After adequate exposure, a wedge measuring almost 9 mm was removed on the medial side under c-arm guidance while as lateral hinge was protected. The deformity was corrected by medial gentle traction till the osteotomy gap was completely obliterated. Correction was confirmed intra-operative by imaging and after achieving satisfactory reduction the osteotomy site was fixed with a strong locking plate construct. The patient was allowed immediate weight bearing on day 1 the post-operative period and discharged on day 2. This was followed by rehab for a couple of weeks. A similar procedure was repeated on the other side after a gap of 3 months.
Post-operative protocol
The patient was allowed weight bearing from post-operative day 02 and taught Quadriceps strengthening exercises and knee range of motion exercises to increase stability around the knee joint.
Complications
The patient developed paresthesia over the dorsum of the left foot along with weakness of the Extensor hallucis longus tendon indicating deep peroneal nerve involvement on the right side as the common perineal nerve was not released thinking that the correction required was less. He underwent targeted physiotherapy and the neuropraxia affecting the deep peroneal nerve subsided in about 4 weeks with no residual effect.
Follow-up
Following discharge from the hospital on post-operative day 7, the patient followed up regularly up till 6 months. At the 6th month, the patient achieved a neutral mechanical axis on the right side whereas the left side is now in 5° of valgus (Figs. 7 and 8) with complete resolution of clinical valgus. Both Osteotomies eventually have healed successfully. The patient has no instability or pain and is extremely satisfied with the outcome of the surgery. The post-operative clinical picture and radiographs are as Figs. 7 and 8, respectively.


Genu valgum is a coronal plane deformity affecting the knee joint and is a frequent cause of joint instability, gait abnormalities, pain, and patellar malalignment, especially among children and adolescents. Patients often present with recurrent patellar dislocations and the complications associated with the patellar dislocations, such as loose bodies and osteochondral defects in the knee. Genu varum is mainly associated with deformity of the proximal tibia, whereas genu valgum is related to deformities of the distal femur and proximal tibia. Considering the predominant deformity of the proximal tibia, performing hemi-epiphysiodesis only at the proximal tibia is ideal in most adolescents with genu varum [8]. With advancing age, it increases the risk of development and progression to osteoarthritis [9]. Surgical angular correction is only undertaken over a measured intermalleolar distance of 8 cm [10] and mechanical alignment deviation of 12° from the normal; to avoid patellofemoral instability, anterior knee pain, and abnormal gait patterns. Therefore, severe genu valgum deformity warrants surgical intervention to restore biomechanics and improve function, gait, and cosmesis [11]. Changes associated with Genu valgum include an increase in anteversion, Q angle, flat foot, knee hyperextension, and internal rotation of the hip [12]. Before the onset of skeletal maturity, various techniques (fusion of growth plates or temporary suspension of growth) involving growth modulation at the level of growth plates have been described to achieve the desired corrections of alignment. Once the skeletal maturity has been achieved, corrective osteotomies need to be done to correct angular deformity around the knee and restore biomechanics. This involves the removal or addition of wedge-shaped bone pieces based on geometric calculations to correct angular deformity. They are called closing wedge and opening wedge osteotomy, respectively. In the case of wedge osteotomies (either open or closed type), the calculation of the wedge is based on trigonometric calculations or by specific software these days to calculate the precise size of the wedge [13]. Often patients are found to have a deformity in the distal femur with decreased LDFA and require an opening wedge osteotomy to correct the deformity. However, our patient presented with an idiopathic bilateral genu valgum deformity solely caused due to the proximal tibial deformity which is quite unique and rarer with only a few cases reported in the literature. Since our patient was slightly shorter in height (152 cm) radiographs of the spine and a complete metabolic workup were done to rule out any other disorder. A pediatrician consultation was also sought to rule out any unrecognized metabolic disorders. Bilateral Single Level Proximal Medial Tibial Closed Wedge Osteotomy was undertaken due to the prospect of better biomechanical stability and the feasibility of allowing early weight-bearing post-operative. The patient responded well with improved functional status, a satisfactory deformity correction, and a shorter recovery period post-surgical correction. A few complications reported in the literature include infection, thrombophlebitis, neurovascular injury, iatrogenic fracture, under-correction as well as over-correction. Our patient only experienced mild paresthesia over the dorsum of his right foot along with weakness of the Extensor hallucis longus tendon indicating deep peroneal nerve neuropraxia which resolved completely with targeted physiotherapy with no residual effects or functional compromise.
A Single Level Proximal Medial Tibial Closed Wedge Osteotomy is a safe and appropriate strategy to manage the rare cases of idiopathic bilateral genu valgum with tibia valga in the absence of any femoral component. A satisfactory functional status is achievable with good surgical technique and standard post- operative practices.
Genu Valgum is traditionally understood as a deformity of the knee arising from abnormal distal femoral anatomy. However, our case demonstrates that deformity could be of tibial origin as well. Therefore, a thorough clinical examination and assessment of deformity by measuring different angles is warranted in all cases of Genu valgum deformity to provide correct treatment to the patients.
References
- 1.Vaishya R, Shah M, Agarwal AK, Vijay V. Growth modulation by hemi epiphysiodesis using eight-plate in genu valgum in paediatric population. J Clin Orthop Trauma 2018;9:327-33. [Google Scholar | PubMed]
- 2.Jowett C, Barry M. Lower limb alignment and leg length discrepancy. In: Aresti NA, Ramachandran M, Paterson M, Barry M, editors. Paediatric Orthopaedics in Clinical Practice. In Clinical Practice. London: Springer; 2016. p. 189-203. [Google Scholar | PubMed]
- 3.Ekwedigwe HC, Enweani UN, Madu KA, Nwadinigwe CU, Okwesili IC, Ekwunife RT. Clinical measurement of angular profile of the knee and correlation with intermalleolar distance in children in Enugu metropolis. Niger J Clin Pract 2020;23:7-11. [Google Scholar | PubMed]
- 4.Gupta P, Gupta V, Patil B, Verma V. Angular deformities of lower limb in children: Correction for whom, when and how? J Clin Orthop Trauma 2020;11:196-201. [Google Scholar | PubMed]
- 5.Castañeda P, Urquhart B, Sullivan E, Haynes RJ. Hemiepiphysiodesis for the correction of angular deformity about the knee. J Pediatr Orthop 2008;28:188-91. [Google Scholar | PubMed]
- 6.Gautam VK, Maini L, Gupta R, Sabharwal A, Arora S. Flexion test in the coronal plane deformities of knee. J Clin Orthop Trauma 2013;4:115-8. [Google Scholar | PubMed]
- 7.White GR, Mencio GA. Genu valgum in children: Diagnostic and therapeutic alternatives. J Am Acad Orthop Surg 1995;3:275-83. [Google Scholar | PubMed]
- 8.Shim JW, Lee SS, Ko KR. Contributions of the distal femur and proximal tibia to idiopathic genu varum and genu valgum in adolescents. Clin Orthop Surg 2024;16:1010-8. [Google Scholar | PubMed]
- 9.Dean RS, Beck EC, Waterman BR. Knee malignment: Is there a role for correction in primary ACLR? Oper Tech Sports Med 2021;29:150833. [Google Scholar | PubMed]
- 10.Heath CH, Staheli LT. Normal limits of knee angle in white children-Genu varum and genu valgum. J Pediatr Orthop 1993;13:259-62. [Google Scholar | PubMed]
- 11.Ambrožič B, Slokar U, Brulc U, Novak S. Anatomic knee joint realignment. In: Bozkurt M, Açar Hİ, editors. Clinical Anatomy of the Knee. Berlin: Springer International Publishing; 2021. p. 207-47. [Google Scholar | PubMed]
- 12.Mozafaripour E, Rajabi R, Minoonejad H. Anatomical alignment of lower extremity in subjects with genu valgum and genu varum deformities. Phys Treat Specif Phys Ther J 2018;8:27-36. [Google Scholar | PubMed]
- 13.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res 1992; 280:65-71. [Google Scholar | PubMed]









