To understand how mentorship supports professional growth in orthopedics and learn effective strategies for building strong mentor–mentee relationships
Dr. Janki Sharan Bhadani, Department of Orthopaedics, PARAS HMRI Hospital, Patna, Bihar, India. E-mail: jsbhadani@gmail.com
Introduction: Mentorship is essential to the professional and personal development of orthopedic surgeons. It promotes continuous learning, supports career development, and helps develop future leaders in the field. Our study explains key aspects of effective mentorship, differentiates mentorship from coaching, and highlights strategies to enhance mentor–mentee relationships.
Materials and Methods: A literature review was conducted to identify best practices in orthopedic mentorship using established models, expert opinions, and real-world training experiences.
Results: Strong mentorship positively impacts skill development, career progression, and overall job satisfaction. Key elements include structured guidance, open communication, and mutual commitment. Differences between mentorship and coaching were elucidated, emphasizing their distinct roles in professional development.
Discussion: Effective mentorship programs require formal structures, clear expectations, and institutional support. Successful mentor-mentee relationships thrive on trust, regular feedback, and goal alignment. Practical strategies to strengthen mentorship in orthopedic training include mentorship training for faculty, structured pairing programs, and promoting a supportive learning environment.
Conclusion: Mentorship is critical in orthopedic education and career development. Establishing strong mentorship programs can enhance learning, improve professional satisfaction, and develop future leaders in the specialty. Institutions should prioritize structured mentorship frameworks to ensure long-term success.
Keywords: Mentorship, professional development in orthopedics, mentor–mentee relationship, career growth, medical education, e-mentorship.
The professional development journey in orthopedics requires more than just acquiring technical expertise; it demands the guidance of mentorship to navigate clinical challenges, drive research advancements, foster leadership, and maintain ethical integrity [1]. Mentorship bridges the gap between theoretical learning and real-world application, shaping a surgeon’s growth toward mastery [2,3]. In a field that balances precision, innovation, and compassion, mentorship becomes indispensable for nurturing not only technical proficiency but also professional resilience and adaptability [4]. Historically rooted in an apprenticeship model where seasoned surgeons imparted their knowledge through hands-on guidance, orthopedic mentorship has evolved into a comprehensive, multifaceted framework [5,6]. Modern residency and fellowship programs now embed structured mentorship approaches alongside traditional experiential learning to address the growing complexities of the profession [7,8]. This shift highlights the essential role of mentorship in driving personal development, fostering clinical excellence, and promoting innovation [9]. Effective mentorship empowers orthopedic surgeons by refining their decision-making skills, enhancing leadership qualities, and fostering a commitment to lifelong learning [10]. Beyond skill acquisition, mentorship encourages surgeons to contribute to advancements in research, ethical practice, and health-care leadership [1,11]. Today, mentorship models have expanded to include one-on-one guidance, peer mentoring, and virtual e-mentorship opportunities [12]. These diverse formats cultivate continuous learning, strengthen professional confidence, and open doors to broader career possibilities [13]. Structured frameworks foster inclusivity, champion a growth mindset, and prepare the next generation of orthopedic leaders to meet future challenges and innovations [14]. This review explores the pivotal role of mentorship in building a skilled, resilient, and diverse orthopedic workforce – laying the foundation for enduring excellence in surgical practice, patient care, and research innovation.
This review article explores the role of mentorship in professional development in orthopedics, with a focus on building a culture of mentorship in orthopedic programs. A comprehensive literature review was conducted, including primary research studies, systematic reviews, and expert opinion papers related to mentorship in the field of orthopedics. The selection criteria for the reviewed articles were based on relevance to the core themes of mentorship, professional development, leadership, and career growth within orthopedic surgery.
Literature search strategy
A systematic search of academic databases, including PubMed, Google Scholar, and Scopus, was performed to identify relevant studies published between 2000 and 2024. Keywords used in the search included “mentorship,” “orthopedics,” “professional development,” “career growth,” “mentor–mentee relationships,” “leadership,” “clinical training,” “research mentorship,” and “e-mentorship.” The search was refined to include studies focused on mentorship in medical education, specifically within orthopedics, and articles discussing the different models of mentorship, challenges, and strategies for effective mentoring.
Inclusion and exclusion criteria
The inclusion criteria for this review consist of peer-reviewed articles, reviews, and case studies that focus on mentorship in orthopedics. Eligible studies must address the impact of mentorship on clinical competence, career progression, personal development, and leadership within the field. In addition, articles exploring various models of mentorship, such as traditional one-on-one mentorship, peer mentorship, and e-mentorship, are included. Papers discussing mentorship programs or strategies designed for orthopedic residents, fellows, or early-career surgeons are also considered. The exclusion criteria include non-English language articles and studies that are unrelated to mentorship or focus on other medical specialties. Furthermore, studies that do not specifically address mentorship in orthopedics are excluded from the review.
Data extraction and synthesis
Data were extracted from the selected studies, focusing on key aspects of mentorship in orthopedics. The review examined different mentorship models, including one-on-one, team-based, peer, and e-mentorship, assessing their effectiveness in the field. It also explored the benefits of mentorship, highlighting its contributions to clinical skill development, career guidance, leadership training, and academic growth. Common challenges, such as time constraints, mismatched expectations, and lack of institutional support, were identified. In addition, strategies for fostering successful mentor–mentee relationships, including setting clear expectations, providing regular feedback, and promoting open communication, were analyzed. The review further evaluated institutional support and formal mentorship programs designed to enhance mentorship in orthopedics [15]. The extracted data were synthesized into thematic categories and analyzed to provide a comprehensive overview of the current state of mentorship. This review also discusses best practices, emerging trends, and the role of technology in facilitating mentorship relationships.
Defining mentorship and its importance
Mentorship is a dynamic, protected relationship where a more knowledgeable or experienced individual guides and nurtures the personal and professional growth of a less experienced mentee [13,16]. This process, distinct from coaching, tends to focus on short-term, task-specific guidance that fosters a long-term bond that promotes both career and personal development [17,18]. At its core, mentorship is a collaborative partnership wherein the mentor imparts wisdom, experience, and expertise while the mentee gains insights tailored to their unique goals and aspirations [19]. The mentor’s role is not only to provide guidance but also to offer feedback, support, and the tools necessary for the mentee to thrive in their career. In doing so, the mentor also hones their own skills, growing alongside the mentee [20]. Unlike traditional manager-subordinate relationships, mentorship is free from hierarchical constraints, creating a space for an open exchange of knowledge and ideas [21]. As the mentee progresses, the mentor adapts their approach to meet evolving needs, ensuring that the guidance remains effective and meaningful. Mentorship thus becomes a mutually beneficial relationship, driving the growth of both individuals involved, where learning is a shared, ongoing experience [22,23].
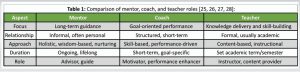
Comparison of mentor, coach, and teacher roles in professional development
Mentor, coach, and teacher are distinct roles, each with its unique approach and focus in fostering development. A mentor provides long-term guidance based on experience and wisdom, often in a less formal, ongoing relationship. A coach focuses on specific goals or performance improvement, offering structured, short-term, and targeted interventions. A teacher delivers knowledge in a structured environment, focusing on skill-building and content delivery through organized lessons. Below is a comparison table summarizing their key differences [13,24] (Table 1) [25-28].
Mentorship models and phases of mentorship
Mentorship in orthopedics is an evolving process that fosters professional growth through various structured models. These models, such as one-on-one, team-based, and peer mentoring, offer different approaches to development. A critical aspect of effective mentoring is the progression through different phases, ensuring the mentor–mentee relationship remains dynamic and purposeful. These phases help mentees transition from novices to experts [29] (Table 2) [5, 10, 30-34].

David Clutterbuck’s five-phase model for developmental relationships plays a crucial role in shaping the mentorship journey [34]. The first phase, Rapport Building, focuses on establishing trust and understanding between the mentor and mentee. This is followed by Direction Setting, where the mentor helps the mentee define clear and realistic goals. In the Progress-Making phase, the mentee takes actionable steps toward these goals with continuous guidance and feedback from the mentor. As the mentee gains independence, the relationship enters the Winding Down phase, where direct mentorship gradually decreases. Finally, in the Moving On phase, the mentee transitions into a new stage, either assuming greater responsibilities or taking on a mentorship role themselves. In addition to the models listed, mentorship can also be categorized based on key mentoring functions. The Kram model, for instance, defines psychosocial functions such as providing acceptance, counseling, friendship, and role modeling. These elements support the mentee throughout the mentorship journey, aligning with different phases of the relationship. This structure highlights how mentorship in orthopedics evolves through structured phases, with each model catering to distinct needs and stages in a surgeon’s career, enhancing their professional and personal growth [35].
Types of mentors in orthopedics
Mentors in orthopedics play diverse roles, including clinical supervision, career guidance, and research mentorship. From seasoned experts to supportive peers, they help trainees navigate challenges, develop technical skills, and achieve their goals [10,36]. Effective mentorship fosters collaboration, mutual growth, and a tailored approach to each mentee’s needs, enriching their professional journey [37] (Table 3) [10, 36-41].

Finding the right mentor
Finding the right mentor involves aligning career goals, personal values, and the mentor’s qualities. Effective mentors have experience, empathy, and a genuine interest in helping mentees grow. They challenge constructively, share values, and foster open communication. While great mentors inspire success, “tormentors” hinder progress by creating obstacles and discouragement [22,42]. Finding the right mentor is key for professional development. An effective mentor provides guidance, challenges you constructively, and aligns with your values and goals. To find the right mentor, assess their experience, communication style, and commitment [43]. Look for someone who can offer support, challenge you, and help you achieve your aspirations (Table 4) [22,42,43].
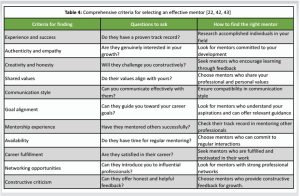
Successful mentor–mentee relationships thrive when built on mutual respect, shared goals, and open communication. Mentees should seek mentors who challenge their perspectives, encourage growth, and provide guidance without imposing their own career path [44,45].
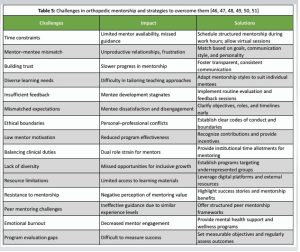
Challenges in orthopedic mentorship
Mentorship is vital for nurturing talent in orthopedics, yet it faces numerous obstacles, such as mismatched expectations, time constraints, and varying mentee needs [46]. Effective solutions require communication, adaptability, and institutional backing to foster impactful relationships. Effective mentorship in orthopedics demands continuous effort to overcome these challenges, ensuring a supportive environment for both mentors and mentees [47] (Table 5) [46-51].
Mentorship protocol: Steps for effective mentorship in orthopedics
Mentorship in orthopedics follows a structured process to help both mentors and mentees grow professionally, develop new skills, and build strong working relationships. The first step is to create a mentorship culture that strengthens trust, respect, and knowledge-sharing, ensuring that both mentors and mentees feel comfortable and supported [52]. Next, mentor–mentee pairs should be carefully matched based on their interests, goals, and experience to maximize the benefits of the relationship. Once paired, it is important to set clear expectations regarding roles, communication, and objectives to maintain a structured and productive mentorship experience [53]. As the mentorship progresses, regular feedback is essential to address challenges, provide guidance, and adjust approaches when necessary. Open discussions between mentors and mentees make the process more effective and supportive. Finally, the mentorship process should be regularly evaluated to track progress and implement improvements. As mentees gain confidence and skills, they gradually transition toward independence while maintaining a professional connection with their mentors. These steps ensure that mentorship in orthopedics remains well-organized, effective, and beneficial for everyone involved (Fig. 1) [13,39,48,52,53].

Effective mentorship strategies involve establishing a supportive culture, selecting appropriate mentor–mentee pairs, defining expectations, encouraging consistent feedback, and evaluating progress. These strategies guide different phases of mentorship, including preparation (discovery), negotiation (goal setting), enabling growth (learning), and closure (evaluation and wrap-up). A structured approach ensures that mentorship remains a dynamic and evolving process, fostering professional development and strong mentor–mentee relationships in orthopedics [54].
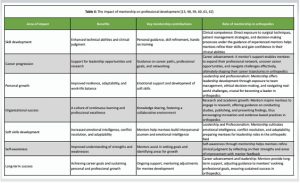
Mentorship benefits in orthopedics
Mentorship in orthopedics has a profound impact on clinical skill development, career guidance, leadership training, and promoting diversity and innovation. It plays a vital role in refining technical abilities, providing guidance in complex clinical decisions, and offering insights into leadership roles within the health-care environment [55]. Through structured mentorship, orthopedic professionals not only develop their clinical competence but also gain invaluable career advice, preparing them for future challenges and leadership positions [56].
Clinical skill development
Mentorship helps mentees enhance their technical abilities, making them proficient in performing procedures and managing clinical situations. Mentors provide direct guidance during surgeries and complex cases, instilling confidence and competence that help mentees grow into skilled professionals [9]. Through consistent feedback and hands-on practice, mentees learn to make informed decisions and improve their clinical judgment [57].
Career guidance and leadership training
Mentors also offer crucial career advice, helping mentees navigate professional pathways, access career opportunities, and manage work-life balance. Leadership training, including team management, ethical decision-making, and conflict resolution, is an essential part of mentorship [13,48]. This guidance prepares mentees for higher responsibilities within orthopedic departments, academic settings, or even research roles [10,51].
Promoting diversity and innovation
Mentorship fosters a culture of inclusion, encouraging diverse perspectives in the field. It ensures that underrepresented groups in orthopedics have access to support and guidance that may not have otherwise been available [55]. Furthermore, mentorship promotes innovation by inspiring mentees to engage in research and evidence-based practice, helping shape the future of orthopedics with new ideas and methodologies [58] (Table 6).
Institutional support and programs for mentorship
Institutional programs create a framework that supports mentorship at various levels of the academic hierarchy. By equipping faculty members with the right skills and providing leadership training, these programs foster a positive environment where both mentees and mentors can thrive [1]. The effectiveness of these programs can significantly impact the development of future orthopedic surgeons and medical professionals. Therefore, regular evaluation of these programs is essential to ensure they meet the evolving needs of mentorship in medical education [63].
Emerging trends in mentorship
Emerging trends in mentorship in orthopedics highlight the growing influence of digital platforms and e-mentorship [64]. These virtual tools offer flexibility, enabling mentees to connect with mentors worldwide, especially in underserved areas [65]. E-mentorship allows continuous learning through online meetings, discussion forums, and video tutorials, expanding access to expertise and fostering global collaboration [66]. Global collaborations in mentorship further enhance the learning experience by promoting cross-cultural exchanges and bridging regional training gaps [67]. These initiatives encourage inclusivity, equity, and the sharing of best practices, ensuring that orthopedic professionals stay updated on emerging techniques and advancements while fostering a more diverse and interconnected global community [68].
Limitations
One limitation of this manuscript is the variability in mentorship models and the lack of standardized definitions of mentorship across studies. Mentorship in orthopedics encompasses diverse models, ranging from traditional one-on-one guidance to more structured approaches such as peer and e-mentorship [69-71]. The absence of uniformity in defining and categorizing these mentorship frameworks complicates comparisons and evaluations of their effectiveness [72]. This variability is further compounded by regional, institutional, and cultural differences in how mentorship is implemented, which can influence both the mentoring process and its outcomes [13,73]. Another limitation lies in the potential biases in self-reported data from mentees, a common issue in many mentorship studies. Mentees may overstate the benefits of their mentorship experiences due to social desirability or a desire to maintain positive relationships with mentors, leading to inflated perceptions of the mentorship’s impact [74]. In addition, the rapidly evolving nature of mentorship models, particularly in the realm of digital and e-mentorship, means that newer studies and innovations may emerge after this review is conducted [75]. These changes in mentorship delivery could offer new insights that challenge or expand upon the findings of this review [38].
Ethical considerations
As this is a review article, no direct patient data was collected or analyzed. The studies included in the review were selected based on ethical guidelines as described in the original research. The findings from this review are intended to provide insights into the importance and effectiveness of mentorship in orthopedics, with a focus on fostering professional development and leadership within the field. This approach ensures that the review is both comprehensive and focused on actionable strategies for improving mentorship within orthopedic programs.
Mentorship in orthopedic professional development bridges the gap between formal education and the practical demands of clinical practice [76]. The evolving models of mentorship – from traditional apprenticeships to structured, multidimensional frameworks – highlight the increasing recognition of its importance in nurturing both technical competence and professional growth [9]. Through personalized guidance, mentorship fosters the development of essential skills, supports emotional resilience, and helps orthopedic surgeons navigate complex challenges inherent in patient care, research, and leadership roles [9,10].
Best practices for mentorship
Effective mentorship in orthopedic surgery relies on several best practices that enhance its impact. Structured mentorship programs integrated within residency and fellowship curricula ensure a consistent approach to skill development and career preparedness [77]. At the same time, personalized guidance tailored to individual learning styles, goals, and challenges fosters deeper engagement and professional growth [78]. Mentorship also plays a crucial role in promoting diversity and inclusion, supporting underrepresented groups, and encouraging diverse leadership roles within the field [79]. In addition, the rise of digital platforms has expanded mentorship opportunities, enabling virtual connections across geographic boundaries and facilitating global knowledge sharing [80]. By combining these strategies, mentorship becomes a powerful tool for professional development and equity in orthopedic surgery. Studies have demonstrated that mentorship not only accelerates technical and academic progress but also offers critical support in navigating unforeseen challenges [78]. Through cultivating professional networks and fostering collaboration, mentorship helps build a community of orthopedic professionals dedicated to lifelong learning and innovation [76].
Future directions
To further enhance the value of mentorship, several key areas warrant consideration. Practical steps, such as structured mentorship workshops, clear documentation of mentorship goals, and scheduled progress reviews, can provide a more organized framework for mentor-mentee relationships. Formal evaluation and feedback mechanisms are essential for refining mentorship programs, ensuring they align with the evolving needs of orthopedic trainees [47]. In addition, enhanced digital integration can expand virtual mentorship initiatives, increasing accessibility and inclusivity by connecting mentees with mentors worldwide [65]. Developing dedicated mentorship platforms with interactive features like case discussions, virtual simulations, and live surgical mentoring can further enrich the experience. Interdisciplinary mentorship models that foster collaboration across specialties can provide orthopedic surgeons with a broader perspective on patient care and research strategies [47,81]. Finally, mentorship training for mentors through standardized programs can equip them with effective communication and leadership skills, ultimately optimizing mentorship outcomes [39,82]. By addressing these areas, mentorship programs can become more structured, inclusive, and impactful. By synthesizing best practices and embracing future advancements, mentorship can continue to be a transformative force in orthopedic professional development – shaping the next generation of surgeons and driving progress in surgical innovation, patient care, and health-care leadership [83,84].
Mentorship plays a crucial role in shaping the professional development of orthopedic trainees and early-career surgeons. Structured mentorship programs have demonstrated significant benefits in skill development, career progression, and professional networking. However, the success of mentorship depends on well-defined roles, institutional support, and continuous assessment of effectiveness. By cultivating effective mentor–mentee relationships and dynamic mentorship practices, the growth of both individuals and the field as a whole is ensured. By prioritizing mentorship, the orthopedic community can build a legacy of excellence and adaptability to meet the evolving demands of patient care and scientific discovery. Future research should focus on optimizing mentorship models and evaluating long-term outcomes.
Mentorship helps orthopedic surgeons grow by bridging the gap between theory and practice. Strong mentor–mentee relationships support skill development and career advancement. Structured mentorship programs can improve learning and patient care.
References
- 1.Choi AM, Moon JE, Steinecke A, Prescott JE. Developing a culture of mentorship to strengthen academic medical centers. Acad Med 2019;94:630-3. [Google Scholar | PubMed]
- 2.Kerdegari N, Tandanu E, Lee K, Zakri R, Dasgupta P, Chandak P. A prospective cohort study on the role of surgical mentorship on medical students’ surgical experience and attitudes towards surgery. BMC Med Educ 2024;24:1116. [Google Scholar | PubMed]
- 3.Platz J, Hyman N. Mentorship. Clin Colon Rectal Surg 2013;26:218-23. [Google Scholar | PubMed]
- 4.Treasure AM, Hall SM, Lesko I, Moore D, Sharan M, Van Zaanen M, Yehudi Y, et al. Ten simple rules for establishing a mentorship programme. PLoS Comput Biol 2022;18:e1010015. [Google Scholar | PubMed]
- 5.Steelman K, Fleifel D, Waheed M, Vaidya R. Mentorship in a surgical residency: A comprehensive review of the literature. Cureus 2023;15:e43422. [Google Scholar | PubMed]
- 6.Entezami P, Franzblau LE, Chung KC. Mentorship in surgical training: A systematic review. Hand (N Y) 2012;7:30-6. [Google Scholar | PubMed]
- 7.Teo MY, Ibrahim H, Lin CK, Abdul Hamid NA, Govindasamy R, Somasundaram N, et al. Mentoring as a complex adaptive system - a systematic scoping review of prevailing mentoring theories in medical education. BMC Med Educ 2024;24:726. [Google Scholar | PubMed]
- 8.Joe MB, Cusano A, Leckie J, Czuczman N, Exner K, Yong H, et al. Mentorship programs in residency: A scoping review. J Grad Med Educ 2023;15:190-200. [Google Scholar | PubMed]
- 9.Burgess A, Van Diggele C, Mellis C. Mentorship in the health professions: A review. Clin Teach 2018;15:197-202. [Google Scholar | PubMed]
- 10.Mulcahey MK, Waterman BR, Hart R, Daniels AH. The role of mentoring in the development of successful orthopaedic surgeons. J Am Acad Orthop Surg 2018;26:463-71. [Google Scholar | PubMed]
- 11.Francis J, George J, Peng E, Corno AF. The role of teamwork and mentorship in pediatric and congenital heart surgery. Transl Pediatr 2024;13:1870-8. [Google Scholar | PubMed]
- 12.Kaufman MR, Levine D, Casella A, DuBois DL. E-mentoring to address youth health: A systematic review. Adolesc Res Rev 2022;7:63-78. [Google Scholar | PubMed]
- 13.Hill SE, Ward WL, Seay A, Buzenski J. The nature and evolution of the mentoring relationship in academic health centers. J Clin Psychol Med Settings 2022;29:557-69. [Google Scholar | PubMed]
- 14.Burger E, Ghanayem A, Mulcahey MK. AOA critical issues: Promoting leadership development among orthopaedic faculty. J Bone Joint Surg Am 2024; 106(15):p 1439-1444 [Google Scholar | PubMed]
- 15.Jackevicius CA, Le J, Nazer L, Hess K, Wang J, Law AV. A formal mentorship program for faculty development. Am J Pharm Educ 2014;78:100. [Google Scholar | PubMed]
- 16.Krishna LK, Pisupati A, Teo KJ, Teo MY, Quek CW, Chua KZ, et al. Professional identity formation amongst peer-mentors in a research-based mentoring programme. BMC Med Educ 2023;23:787. [Google Scholar | PubMed]
- 17.Mohamed I, MacBeth R, Stephens K, Ramaiya N, Plecha D. Women in academic radiology: Barriers and benefits of representation, mentorship, coaching, and advocacy. Curr Probl Diagn Radiol 2025;54:108-14. [Google Scholar | PubMed]
- 18.Agarwal BB, Agarwal N, Dhamija N, Chintamani. Mentoring in Surgery-Mentor, Parshuram, Dronacharya, Krishan. Indian J Surg 2018;80:81-3. [Google Scholar | PubMed]
- 19.Nassour I, Balentine C, Boland GM, Chu D, Habermann E, Holscher C, et al. Successful mentor-mentee relationship. J Surg Res 2020;247:332-4. [Google Scholar | PubMed]
- 20.Niazi M, Mahboob U, Shaheen N, Gul S, Saeed MHB, Kiyani A. Exploring the factors affecting career progression in informal faculty mentoring sessions within mentor and mentee relationships: A qualitative study. BMC Med Educ 2024;24:1242. [Google Scholar | PubMed]







