Tuberculous synovitis of the knee may rarely present in the early synovitis stage, providing a chance for complete remission without permanent tissue damage; in diabetic patients, these infections may present with diabetic ketoacidosis as in our patient, which is an extremely rare phenomenon
Dr. Kaunteya Ghosh, Department of Orthopaedics, KPC Medical College and Hospital, Kolkata, West Bengal, India. E-mail: kaunteya@outlook.com
Introduction: Mono-articular tuberculosis in hip and knee to present with late features – articular cartilage destruction, muscle wasting, contractures, and deformity. Comorbidities such as diabetes predispose a patient to infections. Purpose: Herein, we present a case of tuberculosis of the knee with rare presenting features.
Case Report: A 74-year-old male, previously non-diabetic, presented to our emergency with features of diabetic ketoacidosis. His urine and blood cultures showed no growth. The physiotherapist noted hamstring spasm pain on motion, knee held at 30°, marked effusion (6th day). Purulent 40 cc aspirate was drained. No organism was found (Gram stain, India ink, or AFB) or culture (erobic, anerobic, and fungal) but aspirate showed marked leukocytosis and raised CRP. USG reported fibrotic lining and the presence of synovial fronds. A history of fatigue, weight loss, and anorexia was elicited. Nodes were impalpable, and the chest was normal. CBNAAT came out negative. The presence of pacemaker implanted 10 years back prevented us from getting a MRI. Biopsy considering diabetes, the procedure was out off. The pulmonologist diagnosed him with smear-negative TB. Anti-tubercular drugs were started.
Conclusion: Early detection of tubercular synovitis is based on clinical suspicion and may prevent the development of bony deformity.
Keywords: Tuberculosis, Knee, paucibacillary, smear-negative Tb, Tubercular synovitis.
The spine, hip, and knee are the three common sites of osteoarticular tuberculosis. Osteoarticular tuberculosis occurs in all age groups in endemic zones and can affect all genders. Classically a lower socioeconomic status, poverty, lack of hygiene awareness, nutritional deprivation, immunosuppression, and the presence of comorbidities such as uncontrolled diabetes, malignancy, HIV, and high-risk behavior such as injection drug abuse have been independent risk factors for tuberculosis. Tuberculosis occurs either as reactivation of latent disease, bacteremia from sites of active disease, spread from neighboring tissues, implantation, or full-blown miliary tuberculosis. Symptoms of systemic tuberculosis are classically not seen in osteoarticular tuberculosis affecting the appendicular skeleton [1]. Mono-articular tuberculosis is common in large weight-bearing joints such as the hip and knee and has a propensity to present with late features such as articular cartilage destruction, muscle wasting and soft-tissue contractures, resultant deformity from bone destruction, and soft-tissue imbalance [2]. Comorbidities such as uncontrolled diabetes mellitus predispose a patient to a host of chronic infections and increase morbidity.
Herein, we present a case of tuberculosis of the knee with rare presenting features
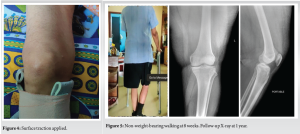
A 74-year-old retired government official presented to our emergency with features of diabetic ketoacidosis (fever, disorientation, fruity smell in breath, fatigue, reduced urine output, and severe weakness) and leukocyte count (TLC 6000, lymphocytes 35%, and neutrophils 64%). He was a known patient of ischemic heart disease and had undergone stenting in three coronary arteries 8 years previously. However, he was non-diabetic previously and DKA was the first presentation of underlying diabetes. He was managed by the ER physician for DKA promptly. On stabilization of vitals, his glycosylated hemoglobin came out to be 15, exposing uncontrolled diabetes – however, his general practitioner’s notes revealed his status as non-diabetic 6 months previously. He was referred to the institutional endocrinologist and started on insulin. On further workup and investigations, his urine and blood cultures showed no growth. From the 2nd day post-admission, he complained of right knee pain and the physiotherapist noted hamstring spasm. The symptoms (pain and hamstring spasm) increased steadily and gradually and on the 6th day post-admission, there was right knee pain on slightest motion, knee held at 30° flexion, and marked effusion in the classic inverted horseshoe pattern. The local temperature was raised (calor) and there was joint line tenderness and rubor. The pain was responding to intravenous paracetamol infusion; however, it was making the symptoms tolerable, pain was not resolving fully. With the development of severe knee pain, his general condition took a hit – he had a toxic look, developed anorexia, and started having night pain. Since the chief symptom was a large, painful, suddenly developed knee effusion with grossly reduced knee ROM, with no history of trauma, we decided to relieve the intraarticular tension in the knee.( Fig. 1 & 2). A purulent 40 cc aspirate was obtained under ultrasound guidance(Fig. 3 ). The aspirate was examined in the departments of biochemistry, pathology, and microbiology for biochemical markers, physical examination, cellular examination, routine microscopic examination, and culture sensitivity, respectively. On physical assessment, the aspirate was deeply turbid yellow in color with a hint of cobweb coagulum. No organism was found on staining and examination under a microscope (Gram stain, India ink, or AFB). The culture reports (both erobic, anerobic, fungal, and bactec) were negative as well. Cellular counts, however, showed marked leukocytosis (90% polymorphs) and raised CRP (73). The leukocyte esterase strip test was unavailable at that date (November 2021) in our institute. He was treated with supportive measures and injection linezolid 600 tds empirically – to cover for common soft-tissue organisms, especially Staphylococcus. Aspiration provided some mechanical relief to the patient, including pain relief; however, ROM did not improve much. We provided him with a compression bandage, ice pack, and systemic anti-inflammatory medication to alleviate symptoms. Below-knee traction was provided to immobilize the limb and further help in achieving analgesia (7.5 lbs weight), particularly at night.(Fig. 4 ). A repeat aspiration under USG guidance was performed after 2 days for the same complaints – staining and culture reports came back negative again. Ultrasound assessment of the knee joint post aspiration showed fibrotic lining of the synovial pouch and the presence of synovial fronds – radiological markers of chronic insult to the knee, though not specifically pointing to a particular etiology. A history of increasing fatigue on exertion particularly long walks, weight loss of 6 kg over 9 months, gradually developing anorexia, and conjunctival pallor was elicited. Popliteal nodes were impalpable, and chest examination and X-rays were normal. Synovium appeared thickened and inflamed on clinical examination and a similar swelling appeared in the ipsilateral ankle. The knee was held at 30° flexion and any movement was exquisitely painful. Cartridge-based nucleic acid amplification test or CBNAAT from arthrocentesis came out negative both times, X-ray knee showed hamstrings swelling. The presence of a pacemaker ruled out MRI as an imaging option. A biopsy was being planned – but due to consideration of chronic non-healing wounds (diabetes) and tuberculosis, both independently and in additive measure, the procedure was decided against. HIV seronegative status was confirmed and the pulmonologist was consulted. Consultation with Chest and Tb specialist classified him as smear-negative/paucibacillary Tb. Anti-tubercular therapy was started according to Index TB guidelines – a joint project of the World Health Organization (WHO) and the Ministry of Health and Family Welfare, the government of India. The drug regimen prescribed that there is 2 HRZE/10-16 HRE. Initially, the patient was asked to wear a knee brace and below-knee surface traction (7.5 lbs) and strict non-weight-bearing for 8 weeks – since the patient had a severe antalgic gait. Post 8 weeks physiotherapy regimen was instituted with an aim to retrain him in gait stretch, strengthen his muscles, and prevent deformity and contractures. The patient was screened regularly for complications of ATD such as raised liver enzymes and loss of visual acuity. [3, 4]. Gradual physiotherapy, dietary support, home care, family support, and strict compliance to anti-tubercular medication helped him recover fully with no bony deformity (Fig. 5).

Osteoarticular tuberculosis of the appendicular skeleton commonly affects the large, weight-bearing joints of the lower limb such as the hip and knee. These infections are classically monoarticular, and paucibacillary, with minimal synovial deposits (sicca variety). Infections in these sites may or may not present with systemic symptoms. Since there are no systemic problems and the acute phase of the disease is clinically silent, these patients present late with bone destruction, limb deformity, and soft-tissue contractures. The natural history of the disease consists of three phases – synovitis, early arthritis, and late arthritis. In the early stage of the disease, acute inflammation of the joint is the only clinical presentation with non-specific X-ray findings. Articular cartilage destruction and bony deformity follow in the ensuing course. In endemic countries, clinical suspicion of tuberculosis is warranted owing to the presence of a high incidence of cases and the presence of a host of high-risk factors. The presence of crippling morbidity in the late stages of osteoarticular tuberculosis should alert us to diagnose the disease early in the synovitis stage. The presence of comorbidities such as uncontrolled diabetes and systemic signs such as fatigue, anemia, anorexia, loss of body weight, and listlessness prompted us to keep tuberculosis on the list of differential diagnoses. Other differential diagnoses for the same symptoms – pyogenic infections, fungal infections, and malignancy – were conspicuous by the absence of clinical pointers in their favor (negative cytology and culture). USG imaging showed evidence of chronic pathology (fibrotic bands and fronds). The inability to get a positive culture of tuberculosis or positive yield from CBNAAT is perhaps owing to the paucibacillary nature of the disease in the knee. Biopsy was being planned but was not performed keeping in mind the two etiologies of diabetes and probable tuberculosis – which independently and additively lead to chronic non-healing wounds, the biopsy tract in this case. MRI was not possible owing to the presence of his pacemaker configurations though in afterthought it was likely that the findings that MRI would throw up would be non-specific marrow edema or articular fragmentation. Since invasive diagnostic procedures were not practicable, in such a circumstance the treating medical team had to use their powers of judgment and discretion with regards to starting anti-tubercular treatment or watching for a period of time. The INDEX TB guidelines assert that in TB endemic areas it is reasonable to institute ATT in patients with strong clinical/radiological suspicion.The absence of response to injectable antibiotics (linezolid) as demonstrated by repeated effusions further pointed to a non-polyogenic agent. The prompt response to anti-tubercular treatment demonstrated by improved general condition, pain, and systemic symptoms after only 6 weeks of therapy further substantiated our diagnosis in retrospect. The patient was examined regularly for the development of other symptoms or aggravation of tubercular symptoms and preventive measures instituted for the same helped our patient recover without any remarkable problems. Physiotherapy was critical to helping relieve muscle spasms, strengthening the muscles, regaining their tone and conditioning, and improving balance and gait control. The patient was gradually started on non-weight-bearing and progressed to partial weight-bearing and full weight-bearing with necessary gait aids. Nutritional support with amino acid supplementation, Vitamin B6 supplementation (due to isoniazid use), and advice on dietetics proved to be vital. The patient took his course of anti-tubercular treatment for 12 months and was regularly under the supervision of the district tubercular officer who assessed the monthly intake of drugs and other prescribed practices. Following the achievement of satisfactory independent mobility status with no deformity or symptoms and completion of a minimal 12 months of treatment, he was declared as treatment complete/cured as per the Government of India guidelines. Glycemic control was under regular supervision by the institutional internist/endocrinologist and was monitored accordingly at regular intervals. Cardiac assessment revealed that the fatigue and shortness of breath suffered by our patient had no cardiac cause. In retrospect, we decided to treat our patient as a smear-negative category patient owing to strong clinical risk factors and clinical findings. The presence of diabetic ketoacidosis was a rare presenting feature which is extremely rare if not unheard of in the literature survey. The remarkable recovery of our patient with no complications or development of new symptoms provided further backing to the treatment rationale.
Early detection of tubercular synovitis is based on strong clinical suspicion as the imaging findings are non-specific. However, in TB endemic zones, the diagnosis must be kept in mind as it may prevent the development of crippling bony deformity and risks arising out of recumbency. The presentation of tuberculosis is extremely variable such as the presence of DKA in this case. Ketoacidosis usually rings alarm bells for decompensated systemic infection – however, we must be wary of our old foe – tuberculosis, that too in uncommon sites such as the knee joint in the survey of a patient presenting with DKA.
There should be a high index of suspicion for tuberculosis in synovitis of the knee presenting in endemic zones, especially if infections are suspected and cultures/smears are negative.
References
- 1.Pigrau-Serrallach C, Rodríguez-Pardo D. Bone and joint tuberculosis. Eur Spine J 2013;22 Suppl 4:556-66. [Google Scholar]
- 2.Uboldi MF, Limonta S, Ferrua P, Manunta A, Pellegrini A. Tuberculosis of the knee: A case report and literature review. Joints 2017;5:180-3. [Google Scholar]
- 3.Govt of India MOHFW and WHO. INDEX-TB Guidelines. Switzerland: WHO; 2023 [Google Scholar]
- 4.Government of India. NTEP.pdf-National Tuberculosis Elimination Programme. New Delhi: Government of India; 2023 [Google Scholar]
- 5.Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res 2004;120:316-53. [Google Scholar]
- 6.Phemister DB. The effect of pressure on articular surfaces in pyogenic and tuberculous arthritides and its bearing on treatment. Ann Surg 1924;4:481-500. [Google Scholar]
- 7.Henderson MS, Fortin HJ. Tuberculosis of the knee joint in the adult. J Bone Joint Surgery (Am) 1927;9:700-13. [Google Scholar]
- 8.Alberquerque-Jonathan G. Atypical tuberculosis of the knee joint. SA J Radiol 2006;10:28. [Google Scholar]
- 9.Vaughan KD. Extraspinal osteoarticular tuberculosis: A forgotten entity? West Indian Med J 2005;54:202-6. [Google Scholar]
- 10.Adler CP. Bone Diseases: Macroscopic, Histological and Radiological Diagnosis of Structural Changes in the Skeleton. Germany: Springer; 2000. [Google Scholar]