Xanthogranulomatous osteomyelitis is a rare form of chronic inflammation affecting bone. It usually presents as lytic lesion with or without pathological fracture. Condition is benign which is fully curable after complete excision of the lesion.
Dr. Syam Gangadharan Nair, Department of Orthopaedic surgery, Lourdes Hospital, Kochi, Kerala, India. E-mail: syamgangan@gmail.com
Introduction: Xanthogranulomatous inflammation is a specific form of chronic inflammatory disease histologically characterized by collection of foamy macrophages along with polymorphonuclear leukocytes, activated plasma cells, and lymphocytes of polyclonal origin, in a mosaic-like pattern. The involvement of xanthogranulomatous inflammation of the bone is termed as xanthogranulomatous osteomyelitis (XO). It often presents as a mass-like lesion extending into adjacent structures and so radiological features have little role in pointing to a diagnosis. Definitive diagnosis can only be made by histopathological examination.
Case Report: This report describes a case of 62-year-old male patient who sustained a pathological fracture of shaft of radius which on evaluation, was diagnosed as XO, its management and 2- year follow-up results. This case report highlights a rare cause of pathological fracture, that is, XO.
Conclusion: Clinical examination and radiology have little role in the diagnosis of the condition. Definitive diagnosis is achieved by histopathological examination and the disease has a good prognosis.
Keywords: Xanthogranuloma, inflammation, osteomyelitis, fracture, radius.
Xanthogranulomatous inflammation is a specific form of chronic inflammatory disease histologically characterized by the collection of foamy macrophages along with polymorphonuclear leukocytes, activated plasma cells, and lymphocytes of polyclonal origin, in a mosaic-like pattern [1]. Although it can be encountered in various organs such as lymph nodes, colon, appendix, pancreas, urinary bladder, prostate, testis, epididymis, endometrium, ovaries, fallopian tubes, vagina, and salivary glands, the most common site of involvement are kidney and gallbladder. Lung, brain, and bone are rare sites of occurrence of the disease [2]. The involvement of xanthogranulomatous inflammation of the bone is termed as xanthogranulomatous osteomyelitis (XO). It often presents as a mass-like lesion extending into adjacent structures [3] and so radiological features have little role in pointing to a diagnosis. Definitive diagnosis can only be made by histopathological examination. The important differential diagnosis of XO includes infiltrative carcinoma, Langerhans cell histiocytosis (LCH), Erdheim-Chester disease (ECD), and chronic recurrent multifocal osteomyelitis [4]. Here we present a case of XO involving the shaft of the radius presenting as pathological fracture, its management, and long term follow-up.
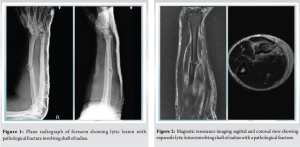
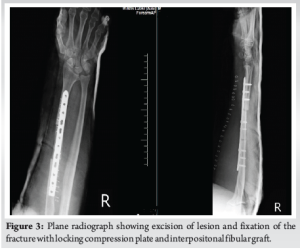
A 62-year-old male patient with no previous comorbidities presented to our outpatient department with complaints of right forearm pain following trivial trauma where his forearm was hit on the side of a table. On clinical examination, there was swelling and tenderness over the shaft of radius. Both pronation and supination were painfully restricted. X-ray revealed lytic lesion and pathological fracture involving the shaft of radius (Fig. 1). Blood parameters showed elevated alkaline phosphatase (375IU/L) and a normal white blood cell count, erythrocyte sedimentation rate, and C-reactive protein. Magnetic resonance imaging (MRI) showed a 2.2 × 1.4 × 1.8 cm T1 isointense, T2 hyperintense expansile lesion centered on the lateral cortex of mid shaft of the right radius with pathological fracture. The lesion showed moderate enhancement on contrast images (Fig. 2). The differential diagnoses according to MRI films were osteoblastoma and multiple myeloma. Patient underwent an excision biopsy of the lesion and fracture fragments along with fixation of radius with 3.5 mm locking compression plate and an interpositonal fibular graft (Fig. 3). Intraoperatively the lesion appeared soft, gritty, yellowish grey material along with fractured bone fragments. The excised specimen was sent for both culture and histopathological examination. Culture was sterile and histopathological examination revealed bony trabeculae with normal marrow elements and dense sheets of foamy histiocytes and a few histiocytic giant cells along with focal dense neutrophilic infiltrate. Furthermore, seen were chronic inflammatory infiltrate against fibrinous background seen (Fig. 4). There was no evidence of epithelioid granuloma, necrosis, or malignancy in the collected specimen. Postoperatively, the affected limb was immobilized in an above elbow plaster of Paris slab for 2 weeks and thereafter encouraged elbow and wrist movements. Subsequent X-rays taken at 3 months and 6 months showed consolidation of fracture and incorporation of fibular graft with no recurrence of the lesion. At 2-year follow-up the fracture has completely healed and the patient had full range of movements in the adjacent joints (Fig. 5).
XO is a specific form of chronic inflammatory disease histologically characterized by collection of foamy macrophages along with polymorphonuclear leukocytes, activated plasma cells, and lymphocytes of polyclonal origin, in a mosaic-like pattern [1]. Exact pathogenesis is unknown; however, defective lipid transport, immunological disorders, low-virulent infections, reactions to specific infectious agents, and lymphatic obstruction have been proposed as putative mechanisms [5]. With respect to the origin of foam cells, it was considered that the vast majority of foam cells were derived from monocytes/macrophages because they were invariably positive for KP1, HAM56, CD11b, and CD68. Delayed type hypersensitivity reaction of cell-mediated immunity may be implicated in the pathogenesis of XO [6]. In the skeletal system, it usually affects long bones. It has a male predominance with male-to-female ratio of 6:1 [7]. Radiologically it often presents as a mass-like lesion extending into adjacent structures [3] and so radiological features have little role in pointing to a diagnosis. Definitive diagnosis can only be made by histopathological examination. Microscopically, the differential diagnosis for XO is LCH, ECD, and lipid storage disorders [2, 8]. LCH usually has preponderance in younger age group and shows Birbeck granules on histological examination. Erdhiem-Chester disease radiologically shows osteosclerosis in almost all cases and histologically shows foamy histiocytes and fibrosis without neutrophilic infiltrations [9]. Infiltrative storage disorder can be differentiated from XO by clinical history, cardiac involvement, and histologically, foamy macrophages of the bone marrow with no signs of inflammation [10]. Xanthogranulomatous inflammation on histology shows characteristic multinucleate giant cells interspersed with lipid-laden macrophages, which impart the characteristic yellow macroscopic appearance. Only a few cases of XO in bone have been reported in the literature. Among these, the earliest two cases were reported by Cozzutto which were in the first rib and the epiphysis of the tibia [1]. Vankalakunti et al. in 2007 reported a case of XO of ulna mimicking neoplasm which was curetted and cancellous iliac crest graft was interposed followed by bridge plating and showed good clinical outcome [2]. Kamat et al. in 2011 reported a case of XO presenting as swelling in the right tibia. They done curettage of the lesion and histopathologically confirmed the diagnosis. An association between bacterial infection and xanthogranulomatous inflammation has existed in several organs, such as the kidneys, and in the gastrointestinal system, but such an association of the two is yet to be determined for bone [1, 6, 11]. In our case, the culture was sterile and the definitive diagnosis was confirmed by a histopathological study [12].
Xanthogranulomatous inflammation is a specific form of chronic inflammatory disease histologically characterized by the collection of foamy macrophages along with polymorphonuclear leukocytes, activated plasma cells, and lymphocytes of polyclonal origin, in a mosaic-like pattern. Bone is a rare site of occurrence of the disease. Clinical examination and radiology have little role in diagnosis of the condition. Definitive diagnosis is achieved by histopathological examination. In the present case, microscopic examination revealed bony trabeculae with normal marrow elements and dense sheets of foamy histiocytes and a few histiocytic giant cells along with focal dense neutrophilic infiltrate. Furthermore, seen were chronic inflammatory infiltrate against fibrinous background seen. There was no evidence of epithelioid granuloma, necrosis, or malignancy in the collected specimen thus confirming the diagnosis of XO.
XO must be kept in mind as a differential diagnosis in an elderly patient with a lytic lesion presenting with a pathological fracture. Plane radiology plays little role in the diagnosis of the condition. Histopathology confirms the diagnosis. Excision of the lesion along with rigid fixation and interpositional fibular graft gives excellent long-term outcome.
References
- 1.Cozzutto C. Xanthogranulomatous osteomyelitis. Arch Pathol Lab Med 1984;108:973-6. [Google Scholar]
- 2.Vankalakunti M, Saikia UN, Mathew M, Kang M. Xanthogranulomatous osteomyelitis of ulna mimicking neoplasm. World J Surg Oncol 2007;5:46. [Google Scholar]
- 3.Unni KK, McLeod RA, Dahlin DC. Conditions that simulate primary neoplasms of bone. Pathol Annu 1980;15:91-131. [Google Scholar]
- 4.Lee SH, Lee YH, Park H, Cho YJ, Song HT, Yang WI, et al. A case report of xanthogranulomatous osteomyelitis of the distal ulna mimicking a malignant neoplasm. Am J Case Rep 2013;14:304-7. [Google Scholar]
- 5.Antonakopoulos GN, Chapple CR, Newman J, Crocker J, Tudway DC, O’Brien JM, et al. Xanthogranulomatous pyelonephritis. A reappraisal and immunohistochemical study. Arch Pathol Lab Med 1988;112:275-81. [Google Scholar]
- 6.Nakashiro H, Haraoka S, Fujiwara K, Harada S, Hisatsugu T, Watanabe T. Xanthogranulomatous cholecystis. Cell composition and a possible pathogenetic role of cell-mediated immunity. Pathol Res Pract 1995;191:1078-86. [Google Scholar]
- 7.Nalini G. Xanthogranulomatous osteomyelitis: A case report. Med J 2014;1:45-7. [Google Scholar]
- 8.Rathi M, Khattri J, Budania SK, Singh J, Awasthi S, Verma S. Xanthogranulomatous osteomyelitis. Arch Med Health Sci 2014;2:228-30. [Google Scholar]
- 9.Yun EJ, Yeh BM, Yabes AP, Coakley FV, Kane CJ. Erdheim-chester disease: Case report and review of associated urological, radiological and histological features. J Urol 2003;169:1470-1. [Google Scholar]
- 10.Ferreira CR, Gahl WA. Lysosomal storage diseases. Transl Sci Rare Dis 2017;25:1-71. [Google Scholar]
- 11.Machiz S, Gordon J, Block N, Politano VA. Salmonella typhosa urinary tract infection and xanthogranulomatous pyelonephritis. Case report and review of literature. J Fla Med Assoc 1974;61:703-5. [Google Scholar]
- 12.Kamat G, Gramapurohit V, Myageri A, Shettar C. Xanthogranulomatous osteomyelitis presenting as swelling in right tibia. Case Rep Pathol 2011;2011:257458. [Google Scholar]










