Pre-axial polydactyly of the foot, a rare congenital condition often linked to genetic syndromes, can significantly impair mobility but can be effectively managed through surgical excision, as demonstrated in a case improving gait and quality of life in a 5-year-old patient.
Dr. Mohan Choudhary, Department of Orthopaedics, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: varunkumarvk3510@gmail.com
Introduction: Polydactyly of the foot, particularly pre-axial polydactyly, is a rare congenital malformation that can occur alongside various congenital anomalies and syndromes. Classification of polydactyly, such as Venn-Watson’s system, aids in understanding the complexity and variability of this congenital condition.
Case Report: This case report details the presentation and surgical intervention of a 5-year-old boy with pre-axial polydactyly characterized by an accessory toe on the right foot, which had hindered his ability to walk properly since birth and his journey through surgical excision for a better stand in life.
Conclusion: Pre-axial polydactyly of the foot is a rare congenital anomaly that can significantly affect mobility and quality of life. Early diagnosis, aided by a detailed clinical evaluation and radiographic imaging, is crucial for appropriate management.
Keywords: Polydactyly, supernumerary, preaxial
Polydactyly of the foot is a congenital malformation which can be classified as pre-axial, post-axial, and central depending on the anatomical location from which the toe emerges [1]. When the anomaly is bilateral, genetic origin must be considered [2,3]. Of this type central is the rarest and post-axial is the most common presentation [4]. Although hand and foot polydactyly in newborns are pretty common, pre-axial polydactyly of the foot is rare [5,6]. Hence, the knowledge about the presentation of pre-axial polydactyly of the foot is important, because they may even be associated with other congenital anomalies including syndactyly and atrial septum defects [7]. Other syndromes which are associated with polydactyly are craniosynostosis or corpus callosum agenesis. Precise surgical technique is important, thereby minimizing the potential need for revision surgery [8]. As there are so little presentations, many clinicians are not familiar with these malformations and associated syndromes, thereby making it harder to diagnose [9,10].
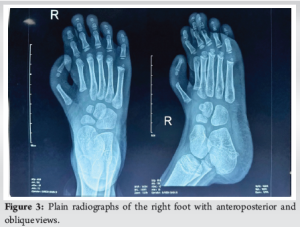
This case report involves a 5-year-old healthy toddler, who has achieved appropriate developmental milestones, which was brought by his worried mother about his right foot deformity and his difficulty to walk properly. The above-mentioned deformity was prevalent since his birth which hindered him to wear normal footwear. Patient had no significant birth history. Patient’s mother gives history of similar deformity over paternal family. Head to toe examination as concluded with no further evidence suggesting other congenital disorder. On examining the right foot of the patient, an accessory toe of size 5 × 2 cm emerged over the medial aspect of the mid-foot (Fig. 1). Skin over the toe appeared to be normal along with a fully developed nail. Minimal flexion was noted over the metatarsophalangeal joint. Plain radiographs of the patient’s right foot showed a metatarsal along with a phalange in the accessory toe (Fig. 2 and 3). Plain radiographs of the contralateral foot were not obtained as the clinical examination of contralateral foot showed no evidence of rudimentary toes. All routine baseline hematological parameters were found to be within normal limits. Pros, cons, and complications for the surgery were explained to the patient’s attendants and proper consent for the surgery was obtained. Patient underwent excision of the supernumerary toe of right foot. Patient was positioned in supine under general anesthesia. A racquet-shaped incision was made encircling the toe with the tail of the incision pointing posteriorly (Fig. 4). Skin was incised deeply. Once the skin was incised, two tendons – flexor hallucis longus and extensor hallucis longus (Fig. 5) was visualized posteriorly and anteriorly over the phalange which was elevated subperiosteally and retracted.


Once the tendons were retracted that a neurovascular bundle supplying the toe (a digital artery, vein, and nerve) was visualized, (Fig. 6) which was cauterized and excised. The metatarsal was separated from surrounding tissues near the pre-axial border of the right foot. En bloc removal of the supernumerary toe was hence performed, and the skin and soft tissue was closed in layers (Fig 7 and 8). Post-operative check plain radiograph was obtained (Fig. 9). Postoperatively, the patient was advised to walk after suture removal. The patient was followed postoperatively 3 months. The patient did not develop any corn or calluses over the affected foot due to uneven balancing. He also had no complaints of tripping while walking, gait abnormalities and rejoiced about his chance to wear normal footwear.
Pre-axial polydactyly of the foot is a rare malformation and often clinicians are unfamiliar with associated malformations and syndromes [1]. They are a common presentation in genetic syndromes but most importantly occur in autosomal dominant inheritance with variable expression [2,3]. Venn-Watson classified [4] polydactyly into pre-axial and post-axial types. Class 1 involves distal duplication with a normal metatarsal. Class 2 features a block metatarsal. Class 3 presents a Y-shaped metatarsal. Class 4 has a T-shaped metatarsal. Class 5 exhibits a normal metatarsal shaft with a widened head. Class 6 involves complete duplication, including the metatarsal. It may be combined with syndactyly. The mainstay surgical treatment of an accessory toe is amputation. General surgical guidelines [5] include (1) preservation of digit with best axial alignment, (2) resection of projecting and symptomatic toe, (3) rebalancing of soft tissues, and (4) provide adequate soft-tissue cover. Tendency to develop axial deviations of first metatarsophalangeal joint is high [6,7]. Genetic study helps in establishing different phenotypes associated [8]. Pre-operative radiographs should be obtained to detect any extra metatarsal articulating with the digits. Surgery should be delayed until skeletal ossification has occurred in the affected ray so that accurate anatomic assessment in surgery is possible [9]. The use of plain radiographs in polydactyl is therefore essential for both diagnosis and surgical approach [10].
Pre-axial polydactyly of the foot is a rare congenital anomaly that can significantly impact mobility and quality of life. Early diagnosis, aided by a detailed clinical evaluation and radiographic imaging, is crucial for appropriate management. Surgical excision of the accessory toe, as demonstrated in this case, is an effective treatment that can restore normal gait and functionality while allowing patients to resume daily activities without limitations. Increased awareness among healthcare providers about this condition and its management can lead to better outcomes for affected individuals.
Early recognition and surgical management of pre-axial polydactyly of the foot are crucial for restoring normal functionality and improving the quality of life. Pre-operative imaging and meticulous surgical planning ensure optimal outcomes, highlighting the importance of awareness and expertise in managing this rare congenital anomaly.
References
- 1.Burger EB, Baas M, Hovius SE, Hoogeboom AJ, Van Nieuwenhoven CA. Preaxial polydactyly of the foot. Acta Orthop 2017;89:113-8. [Google Scholar | PubMed]
- 2.Rampal V, Giuliano F. Forefoot malformations, deformities and other congenital defects in children. Orthop Traumatol Surg Res 2020;106:S115-23. [Google Scholar | PubMed]
- 3.Malik S. Polydactyly: Phenotypes, genetics and classification. Clin Genet 2013;85:203-12. [Google Scholar | PubMed]
- 4.Venn-Watson EA. Problems in polydactyly of the foot. Orthop Clin North Am 1976;7:909-27. [Google Scholar | PubMed]
- 5.Belthur MV, Linton JL, Barnes DA. The spectrum of preaxial polydactyly of the foot. J Pediatr Orthop 2011;31:435-47. [Google Scholar | PubMed]
- 6.Turra S, Gigante C, Bisinella G. Polydactyly of the foot. J Pediatr Orthop B 2007;16:216-20. . [Google Scholar | PubMed]
- 7.Phelps DA, Grogan DP. Polydactyly of the foot. J Pediatr Orthop 1985;5:446-51. [Google Scholar | PubMed]
- 8.Rogers BH, Schmieg SL, Pehnke ME, Shah AS. Evaluation and management of preaxial polydactyly. Curr Rev Musculoskelet Med 2020;13:545-51. [Google Scholar | PubMed]
- 9.Jalili A. Preaxial polydactyly of foot, report of a rare case. Shafa Ortho J 2014;1:e24623. [Google Scholar | PubMed]
- 10.Russo A, Patanè V, Viglione V, Pinto A, Cristiano M, Comune R, et al. Preaxial polydactyly of the foot in an adult patient diagnosed by X-ray after a trauma. Radiol Case Rep 2023;18:1376-9 [Google Scholar | PubMed]











