In our case, we present the first case of a revision of an THA leading to oxalate nephropathy due to the use of antibiotics for the management of a post-operative infection.
Dr. Dimitrios Mouselimis, Department of Orthopaedic Surgery, Klinikum Dortmund, Witten/Herdecke University, Beurhausstr. 40, 44137, Dortmund, Germany. E-mail: dimitrios.mouselimis@klinikumdo.de
Introduction: Although one of the most successful orthopedic procedures, total hip arthroplasty (THA) conveys a not negligible risk for complications.
Case Report: A 72-year-old patient after a THA received an operative revision 2 times due to persistent hematoma and early periprothetic infection. Post-operative renal failure requiring hemodialysis has been caused by a histologically confirmed oxalate nephropathy (ON). Post-operative antibiotic treatment altering the gut microbiome has been assumed as the most likely cause of ON. It is the first presented case of ON as a post-operative complication after a hip arthroplasty revising operation.
Conclusion: Acute post-operative renal injury conveys significant danger for the patients. An interdisciplinary approach is needed as many cases require complex diagnostic and therapeutical procedures offered by experts on the field.
Keywords: Total hip arthroplasty, total hip arthroplasty, complication, acute renal failure, oxalate nephropathy.
Total hip arthroplasty (THA) is considered one of the most successful surgical procedures in terms of treatment outcomes on a global scale [1]. The prevalence of THAs is expected to surge in the coming years due to global aging and the enhanced quality of life that it provides through the operation. This anticipated increase is likely to have a proportional impact on the incidence of post-operative complications, consequently necessitating a rise in future revision operative procedures [2]. Among the potential complications of THA, acute renal injury (ARI) conveys significant morbidity and mortality to the patients, while requiring extended hospital stays including in same cases the need for hemodialysis [3], which represents a significant financial burden for public healthcare systems. In general, ARI is responsible for more than 1.5 million deaths worldwide each year [4]. Oxalate nephropathy (ON) is a rare condition causing acute or chronic renal failure. Regarding the ON epidemiology, restricted data are available in the current literature with a prevalence of approximately 1/100 native renal biopsies reported by a Belgian study for the years 2010–2018 [5]. ON is characterized by calcium oxalate crystals deposition in the renal tubules [5,6]. The severity of ON varies between mild renal failure up to severe cases needing hemodialysis [5,6]. The main causes of the disease are primary hyperoxaluria, which is a hereditary autosomal recessive disease [5,6]. We present the first published case of a patient undergoing revision of a THA with a post-operative end stage renal disease requiring hemodialysis due to ON. The patient provided a signed informed consent for the anonymous publication of the case.
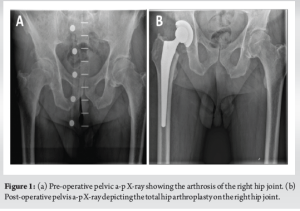
A 72-year-old male patient with severe arthritis of the right hip received a THA (CORAIL™ Stem, PINNACLE™ press-fit cup, PINNACLE™ Marathon-Inlay, CERAMAX™ head) over an anterior lateral approach (baseline date) in our orthopedic department. The pre- and post-operative pelvic anteroposterior radiographic images are presented in Fig. 1a and b, respectively. No intra- and post-operative complications occurred until the discharge to the rehabilitation clinic. Regarding comorbidities, the patient suffered from arterial hypertension and stable coronary artery disease. The standard medication included antihypertensive regimens, specifically valsartan and indapamide, clopidogrel due to allergy against aspirin as an anticoagulant factor after a myocardial infarction 10 years ago and a statin. Subcutaneous dalteparin has been chosen as the antithrombotic therapy rather than rivaroxaban, due to the parallel therapy with clopidogrel.
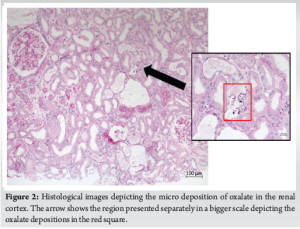
Sixteen days after the surgery and while being in the rehabilitation phase during a rotational movement, the patient reported an unusual “click” in his operated hip. Subsequently, a hematoma developed under the surgical wound, urgently leading the patient to our emergency department. At this moment, he has been receiving an anticoagulant therapy with subcutaneous dalteparin and per. os. clopidogrel 75 mg. The decision for the replacement of the mobile joint components combined with obtaining samples for microbiological examination was directly made. At this point, clopidogrel has been received since more than 7 days (Figure Timeline). Postoperatively, it was discontinued. Intraoperatively occurred no complications. Intravenous ampicillin/sulbactam was administered directly postoperatively due to intraoperative signs of infection. Postoperatively, blood has been transfused due to a hemoglobin of 6.4 g/dL. The intraoperative tissue samples sent to microbiological tests that revealed a Staphylococcus capitis infection, and the antibiotic therapy was switched to intravenous flucloxacillin with the dose adapted to the renal function. Fourteen days after the revision of THA and 1 month after the initial operation, a new revision of the THA was performed due to persistent hematoma and wound secretions. Intraoperatively, 2 g of vancomycin powder were locally applied to the joint and subcutaneous tissues. The mobile parts were replaced again. Only one of the 6 microbiological intraoperatively collected samples was positive for S. capitis according to the antibiogram and, therefore, evaluated as contaminated. The antibiotic therapy with flucloxacillin has been continued for another 2 weeks after the last operation and has been afterward switched to an oral antibiotic therapy with levofloxacin and rifampicin for 10 weeks after the last operation. Another blood transfusion until discharge has been conducted. Clopidogrel could be continued after the uneventful wound healing. After the second revision of the THA, a significant increase of serum creatinine was detected. A nephrological consultation has been requested. The patient suffered an ARI with a maximum serum creatinine level of 8.22 mg/dL. Hemodialysis was initiated 5 days after the last operation. A nephrological differential diagnostic has been performed by our nephrologists. Urine and blood tests were taken. Our patient had a proteinuria up to 500 mg/g rooting from the tubules underlined by the elevated alpha-1-microglobulin. No hematuria was detected, but the urine cultures revealed a urine tract infection with Proteus mirabilis and Escherichia coli, which were adequately handled with the antibiotic therapy received for the periprosthetic infection. Autoimmune tests excluded potential diseases including collagenosis, systemic lupus erythematosus, antineutrophil cytoplasmic antibody angiitis, or rheumatoid arthritis. The only elevated factor was the soluble interleukin 2 receptor (1100 U/mL, normal range: 158–623 U/mL) with normal angiotensin converting enzyme levels. A hanta virus infection was also serologically excluded, as well as a monoclonal gammopathy and diabetes mellitus as the HbA1c was 4.1%. Twenty days after the first operative revision of the THA, a biopsy was needed to identify the reason of ARI. The results showed a severe potentially partially reversible tubular injury in the renal cortex with microdeposition of oxalate (Fig. 2). There were no signs of acute necrotizing extracapillary glomerulonephritis and tubulointerstitial nephritis. To establish the diagnosis of ON, a double separate 24-h urine sample for oxalate measurement was gathered. Both tests revealed an oxalate/creatinine concentration of 30.8 mg/dL, which was slightly above the upper normal limit according to our labor’s normal range (5.9–28.6 mg/dL). The diagnosis of ON was established. After 58 days of intermittent dialysis, the renal function was restored, enabling the discontinuation of dialysis. The last creatinine value was 0.99 mg/dL, measured 116 days after the first session and 58 days after weaning from dialysis. A summary of the case is presented in the timeline in Fig. 3.

Hematoma is a potential post-operative complication after a THA [7]. Perioperative anticoagulation is a significant risk factor for hematoma development for patients receiving a THA [7]. Rivaroxaban 10 mg has been suggested since longer as an antithrombotic therapy in patients receiving native THA [8]. The decision for anticoagulation in our case has been intriguing as no data exist regarding the coadministration of rivaroxaban 10 mg and clopidogrel 75 mg. The allergy of our patient against aspirin rendered difficult the decision for the right antithrombotic therapy after the native THA. Rivaroxaban 10 mg spitted into two daily doses as a monotherapy failed against aspirin according to the COMPASS study, one of the largest including patients with stable angina [9]. Therefore, our team has chosen the dual therapy with clopidogrel and subcutaneous dalteparin. At the end, it has been adequately achieved to handle the complication with a replacement of the mobile parts of the joint and the patient retained full mobility of his hip joint. The infection with S. capitis has also been treated without any persistence of infectious or clinical markers. However, the renal injury was the most serious complication that our team was confronted with in our case and the most important one due to its extent for the patients’ health. ARI is a recognized complication after operative procedures and has to be carefully taken into consideration. The most common causes of ARI are dehydration or intraoperative blood loss [10]. In these cases, a timely blood transfusion or volume substitution may reverse the initial elevation of serum creatinine. However, persistently elevated renal markers should trigger a further investigation. In these cases, an interdisciplinary medical approach is indicated. As in our case, the colleagues of our nephrology department have overtaken the further diagnostical and therapeutical management. ON has been diagnosed. Of high interest is the approach which led to the diagnosis. Initially, common etiologies of ARI were excluded, and no potential diagnosis has been identified until a renal biopsy was performed. We assume that the intake of antibiotics changed the gut microbiome subsequently leading to overproduction and deposition of oxalate molecules in the renal cortex. It is a rare complication that may occur in patients receiving long-term antibiotics [5]. According to our knowledge and research of the literature, there is no similar case of ON after an antibiotic post-operative management of a periprothetic infection that has been published. The most common complications after a THA revising operation are bleeding, thromboembolic events, periprothetic fractures, injury of nerves, and vasculature, while renal failure may also occur and conveys a bad prognosis. A holistic handling of each patient is the cornerstone of good clinical practice. Focusing only on the field of expertise may lead to overseeing some life-threatening complications and should be omitted.
In our case, we timely activated an interdisciplinary team approach for a case of postoperative ARI after a revision of a THA, while receiving antibiotic treatment. The diagnose of ON was set but a reduction of the elevated renal markers has not been timely achieved due to the nature of the disease. However, the patient has been under hemodialysis until the renal function was restored. As implied by the histological results, there were no signs of permanent injury and the weaning from dialysis was achieved approximately 2 months after the first session.
Post-operative ARI may lead to persistent renal failure requiring an interdisciplinary approach to improve the patient’s prognosis.
References
- 1.Petis S, Howard JL, Lanting BL, Vasarhelyi EM. Surgical approach in primary total hip arthroplasty: Anatomy, technique and clinical outcomes. Can J Surg 2015;58:128-39. [Google Scholar | PubMed]
- 2.Abdel MP, Watts CD, Houdek MT, Lewallen DG, Berry DJ. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties. A 40-year experience. Bone Joint J 2016;98-B:461-7. [Google Scholar | PubMed]
- 3.Thongprayoon C, Kaewput W, Thamcharoen N, Bathini T, Watthanasuntorn K, Salim SA, et al. Acute kidney injury in patients undergoing total hip arthroplasty: A systematic review and meta-analysis. J Clin Med 2019;8:66. [Google Scholar | PubMed]
- 4.Mehta RL, Burdmann EA, Cerdá J, Feehally J, Finkelstein F, García-García G, et al. Recognition and management of acute kidney injury in the International Society of Nephrology 0by25 global snapshot: A multinational cross-sectional study. Lancet 2016;387:2017-25. [Google Scholar | PubMed]
- 5.Buysschaert B, Aydin S, Morelle J, Gillion V, Jadoul M, Demoulin N. Etiologies, clinical features, and outcome of oxalate nephropathy. Kidney Int Rep 2020;5:1503-9. [Google Scholar | PubMed]
- 6.Rosenstock JL, Joab TM, DeVita MV, Yang Y, Sharma PD, Bijol V. Oxalate nephropathy: A review. Clin Kidney J 2022;15:194-204. [Google Scholar | PubMed]
- 7.Mortazavi SM, Hansen P, Zmistowski B, Kane PW, Restrepo C, Parvizi J. Hematoma following primary total hip arthroplasty: A grave complication. J Arthroplasty 2013;28:498-503. [Google Scholar | PubMed]
- 8.Liu J, Zhao J, Yan Y, Su J. Effectiveness and safety of rivaroxaban for the prevention of thrombosis following total hip or knee replacement. Medicine (Baltimore) 2019;98:e14539. [Google Scholar | PubMed]
- 9.Eikelboom JW, Connolly SJ, Bosch J, Dagenais GR, Hart RG, Shestakovska O, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med 2017;377:1319-30. [Google Scholar | PubMed]
- 10.Bihorac A, Yavas S, Subbiah S, Hobson CE, Schold JD, Gabrielli A, et al. Long-term risk of mortality and acute kidney injury during hospitalization after major surgery. Ann Surg 2009;249:851-8. [Google Scholar | PubMed]









