A rare presentation of pediatric iliac crest avulsion with associated meralgia paresthetica.
Dr. Dylan Smith, Department of Orthopaedic Surgery, Penn State Health, 500 University Drive, Hershey, Pennsylvania. E-mail: dsmith48@pennstatehealth.psu.edu
Introduction: This case report details an unusual presentation of an iliac crest (IC) avulsion fracture in a 15-year-old male, complicated by meralgia paresthetica (MP), despite no involvement of the anterior superior iliac spine (ASIS). IC avulsion fractures are rare, occurring in only 6.7% of pelvic avulsion fractures (PAF). They are rarely associated with MP, which typically correlates with ASIS injuries due to the proximity of the lateral femoral cutaneous nerve (LFCN).
Case Report: This case suggests a potential anatomical variation where the LFCN may traverse posteriorly to the IC, explaining the MP without ASIS involvement. The patient fully recovered with conservative treatment within 1 month, indicating that the MP symptoms likely resulted from localized inflammation rather than direct nerve injury.
Conclusion: This case highlights the need for awareness of rare anatomical variations and their impact on clinical presentation, reinforcing the importance of a thorough physical examination. Prompt diagnosis is crucial, and while conservative management is effective for minimally displaced fractures, ongoing debates exist regarding surgical intervention criteria. Future research should focus on refining treatment guidelines for pediatric PAF and exploring anatomical variations to understand better and manage atypical symptoms.
Keywords: Meralgia paresthetica, pediatric pelvic avulsion, lateral femoral cutaneous nerve.
Apophyseal avulsion fractures of the pelvis typically occur during a sudden, forceful muscle contraction [1]. In these instances, the force exerted during contraction is translated through musculotendinous units to the apophysis in which they attach and, consequently, separate the apophysis from the rest of the bone. This occurs most frequently in young athletes, as their apophyseal growth plates are still cartilaginous and thus more susceptible to damage from mechanical forces compared to skeletally mature athletes [2]. While pelvic avulsion fractures (PAF) can also result from blunt trauma – such as in the case to be presented – this is far less common. The most prevalent activities associated with PAF are running and kicking, thus making soccer the most frequently associated sport (38.1%) [3]. Further epidemiologic data reveals that males between the ages of 14 and 15 years old are at the greatest risk of experiencing a PAF [3-5]. Moreover, the anterior inferior iliac spine (AIIS), anterior superior iliac spine (ASIS), and ischial tuberosity (IT) are the most common fracture sites [3,5]. In contrast, the iliac crest (IC) and the superior corner of the pubic symphysis are among the rarest locations for a PAF [4,5]. Each zone has muscle originations that, when forcefully contracted, can cause a pelvic avulsion fracture at that site. The rectus femoris originates at the AIIS, and the sartorius originates at the ASIS, the hamstring muscles at the IT, the rectus abdominis muscle at the pubic symphysis, and the abdominal muscles at the IC. Patients who have experienced a PAF commonly report hearing a “crack” at the time of injury, followed by sudden pain [6]. Clinical examination typically reveals localized tenderness, swelling, and limited range of motion [7,8]. Depending on the location of the fracture, additional site-specific findings can be seen; numerous reported cases of ASIS avulsion fractures have presented with pain and/or paresthesia on the anterolateral aspect of the thigh [9-12]. This condition is better known as meralgia paresthetica (MP), a neuropathy due to entrapment of the lateral femoral cutaneous nerve (LFCN) [9]. In the setting of PAFs, this condition is usually specific to the ASIS due to its close proximity to the LFCN and is hardly ever seen in the case of IC avulsion fractures [10]. Treatment includes conservative treatment for 4–6 weeks for most patients with avoidance of high-impact activities. Depending on the source, surgical intervention is recommended based on location and displacement of 15 mm or greater [5,12,13]. The purpose of this case report is to discuss a PAF at a rare location, the IC, that uncharacteristically presented with MP in the absence of ASIS involvement.
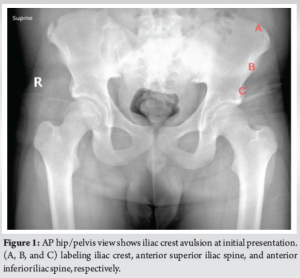
A 15-year-old male presented to the clinic with his mother for evaluation of a right IC avulsion that occurred 1 week prior. The patient initially presented to the emergency department and was diagnosed with a single AP hip/pelvis bilateral radiograph (Fig. 1). The AP pelvic view demonstrated an acute 2–3 mm displaced avulsion fracture of the right anterior IC. The patient was at football practice when a teammate’s helmet collided with his right pelvic area. He felt an immediate “pop” and felt pain. The emergency department recommended pediatric orthopedic follow-up, gave him crutches, and instructed him not to bear weight. The patient endorsed pain in his right hip area for a few days after the injury that had since subsided and intermittent numbness in his right anterolateral thigh. The patient’s examination resulted in mild point tenderness over the fracture site and an antalgic gait. There was also numbness on palpation on the anterolateral thigh, consistent with LFCN distribution. There was no obvious deformity, normal range of motion of lower extremities without pain, and no pain with abdominal or oblique crunches. No further radiologic studies were obtained this visit. The patient and his mother were instructed to bear weight as tolerated, avoid high-impact activities, use crutches as needed, and return to the clinic in 4–6 weeks for a repeat examination and AP hip/pelvis radiograph. At the 1-month follow-up, the patient reported no pain or numbness. His examination was normal, with resolution point tenderness and numbness. There was also no pain with crunches. The AP hip/pelvis radiograph showed a healing avulsion fracture of the right anterior IC (Fig. 2). The patient was told to resume all activities as tolerated with no plan to follow up unless needed.
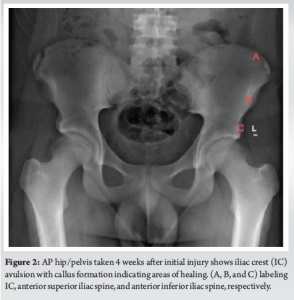
This case report presents a rare instance of an IC avulsion fracture in a 15-year-old male, which was further complicated by the presentation of MP despite no involvement of the ASIS. The patient achieved a full recovery with conservative treatment within 1 month of the initial injury. Among PAF, IC involvement is seen in only 6.7% of cases and rarely presents with MP [5]. Typically, MP is associated with ASIS avulsion fractures due to the LFCN traversing near this pelvic landmark [14]. However, the exact etiology of MP in the context of an IC avulsion fracture is challenging to determine without visualization of the nerve. Literature suggests that a small percentage of the population (approximately 4%) has an anatomical variant in which the LFCN traverses across the IC posterior to the ASIS [14]. This anatomical anomaly may explain the MP experienced by this patient in the absence of ASIS involvement. The resolution of symptoms with conservative treatment suggests that nerve entrapment was likely secondary to local inflammatory processes rather than direct mechanical forces on the nerve by the avulsed apophysis. However, as previously stated, the etiology cannot be definitively determined without visualization of the nerve relative to the fracture. Prompt and accurate diagnosis of PAFs is crucial for appropriate management. While most PAFs, including those with minimal displacement, respond well to conservative management, there is ongoing debate regarding the indications for surgical intervention. Current guidelines are not definitive, but surgical fixation is generally considered for avulsion fractures with significant displacement (over 15 mm) due to the higher risk of non-union [5,13,15]. This case, with only a 2–3 mm displacement, appropriately followed a conservative approach, leading to a successful outcome. The rarity of IC avulsion fractures, especially those presenting with MP, underscores the importance of thorough clinical evaluation and consideration of less common anatomical variations. Clinicians should maintain a high index of suspicion for nerve involvement, even in atypical presentations. Conservative management remains the cornerstone of treatment for minimally displaced avulsion fractures, but careful monitoring for complications such as heterotrophic ossification, loss of strength, and excessive callus formation is essential [16]. Further studies are necessary to establish more precise guidelines for the management of PAFs in pediatric patients. This includes determining the optimal thresholds for surgical intervention and better understanding the long-term outcomes of conservative versus surgical treatments. In addition, further research into the anatomical variations of the LFCN could provide valuable insights into the mechanisms behind atypical presentations of MP, which may further guide treatment protocols.
This case highlights a rare presentation of an IC avulsion fracture with associated MP, successfully managed with conservative treatment. It emphasizes the need for awareness of anatomical variations and careful clinical assessment in managing PAFs. Ongoing research is essential to solidify treatment guidelines and improve outcomes for young athletes experiencing these injuries.
This case highlights the need for awareness of rare anatomical variations and their impact on clinical presentation, reinforcing the importance of a thorough physical examination. Prompt diagnosis is crucial, and while conservative management is effective for minimally displaced fractures, ongoing debates exist regarding surgical intervention criteria.
References
- 1.Kocher MS, Tucker R. Pediatric athlete hip disorders. Clin Sports Med 2006;25:241-53. [Google Scholar | PubMed]
- 2.Metzmaker JN, Pappas AM. Avulsion fractures of the pelvis. Am J Sports Med 1985;13:349-58. [Google Scholar | PubMed]
- 3.Ferraro SL, Batty M, Heyworth BE, Cook DL, Miller PE, Novais EN. Acute pelvic and hip apophyseal avulsion fractures in adolescents: A summary of 719 cases. J Pediatr Orthop 2023;43:204-10. [Google Scholar | PubMed]
- 4.Schuett DJ, Bomar JD, Pennock AT. Pelvic apophyseal avulsion fractures: A retrospective review of 228 cases. J Pediatr Orthop 2015;35:617-23. [Google Scholar | PubMed]
- 5.Eberbach H, Hohloch L, Feucht MJ, Konstantinidis L, Südkamp NP, Zwingmann J. Operative versus conservative treatment of apophyseal avulsion fractures of the pelvis in the adolescents: A systematical review with meta-analysis of clinical outcome and return to sports. BMC Musculoskelet Disord 2017;18:162. [Google Scholar | PubMed]
- 6.Şahin E, Durgut F, Tuğrul Aİ. Nonunion of anterior inferior iliac spine avulsion fracture. Jt Dis Relat Surg Case Rep 2022;1:55-8. [Google Scholar | PubMed]
- 7.Boyce SH, Quigley MA. Simultaneous bilateral avulsion fractures of the anterior superior iliac spines in an adolescent sprinter. BMJ Case Rep 2009;2009:bcr0520091827. [Google Scholar | PubMed]
- 8.Gidwani S, Bircher MD. Avulsion injuries of the hamstring origin - a series of 12 patients and management algorithm. Ann R Coll Surg Engl 2007;89:394-9. [Google Scholar | PubMed]
- 9.Buch KA, Campbell J. Acute onset meralgia paraesthetica after fracture of the anterior superior iliac spine. Injury 1993;24:569-70. [Google Scholar | PubMed]
- 10.Thanikachalam M, Petros JG, O’Donnell S. Avulsion fracture of the anterior superior iliac spine presenting as acute-onset meralgia paresthetica. Ann Emerg Med 1995;26:515-7. [Google Scholar | PubMed]
- 11.Hayashi S, Nishiyama T, Fujishiro T, Kanzaki N, Kurosaka M. Avulsion-fracture of the anterior superior iliac spine with meralgia paresthetica: A case report. J Orthop Surg (Hong Kong) 2011;19:384-5. [Google Scholar | PubMed]
- 12.Hsu CY, Wu CM, Lin SW, Cheng KL. Anterior superior iliac spine avulsion fracture presenting as meralgia paraesthetica in an adolescent sprinter. J Rehabil Med 2014;46:188-90. [Google Scholar | PubMed]
- 13.Di Maria F, Testa G, Sammartino F, Sorrentino M, Petrantoni V, Pavone V. Treatment of avulsion fractures of the pelvis in adolescent athletes: A scoping literature review. Front Pediatr 2022;10:947463. [Google Scholar | PubMed]
- 14.Cheatham SW, Kolber MJ, Salamh PA. Meralgia paresthetica: A review of the literature. Int J Sports Phys Ther 2013;8:883-93. [Google Scholar | PubMed]
- 15.Filippo C, Alessandro N, Cristina G, Margherita M, Francesco P, Francesco C. Apophyseal avulsion fractures of the pelvis. A review. Acta Biomed 2018;89:470-6. [Google Scholar | PubMed]
- 16.Kautzner J, Trc T, Havlas V. Comparison of conservative against surgical treatment of anterior-superior iliac spine avulsion fractures in children and adolescents. Int Orthop 2014;38:1495-8. [Google Scholar | PubMed]