Bilateral anterior shoulder dislocations with greater tuberosity fractures are a rare injury in the pediatric population. Early identification and treatment are important for a successful outcome.
Dr. Connor D Burke, Department of Orthopedic Surgery, University of Toledo, 1125 Hospital Dr, Toledo - 43614, OH, United States. E-mail: connor.burke@utoledo.edu
Introduction: Bilateral anterior shoulder dislocation with associated fracture is a rare pediatric injury that may occur secondary to different etiologies. While trauma is often cited as the most common cause, this injury pattern can also seldomly occur following a seizure episode. With anterior shoulder dislocation, timely reduction is of utmost importance to prevent potential complications.
Case Report: We present a case of bilateral anterior shoulder dislocations with greater tuberosity fractures in a 17-year-old male secondary to status epilepticus. Closed reduction of each dislocation followed by surgical fixation was performed. On final follow-up, the patient demonstrated appropriate range of motion with intact strength, motor, and sensory function of both upper extremities.
Conclusion: Our patient had an uncommon presentation of bilateral shoulder fracture-dislocations secondary to atypical etiology. Delayed diagnosis and treatment of a shoulder dislocation may have devastating consequences, especially in the pediatric population. This includes the increased risk of avascular necrosis if not managed appropriately. In this case, we highlight the significance of being vigilant about the potential complications of bilateral shoulder dislocations while patients are admitted and in critical status. This unusual presentation in a pediatric male with status epilepticus illustrates the necessity for prompt recognition and intervention. Healthcare professionals should remain cognizant of this potential presentation to mitigate potential long-term consequences of failed recognition of this pathology.
Keywords: Shoulder, fracture, seizure, pediatric, status epilepticus.
Bilateral anterior shoulder dislocations coupled with greater tuberosity fractures represents a distinctive subset of shoulder injuries that demand careful consideration due to their unique clinical challenges and potential complications. Bilateral anterior shoulder dislocations are rare injuries that occur in an estimated 23.9/100,000 persons/year and associated greater tuberosity fractures occur in a minority of all shoulder dislocations [1,2]. These rare concomitant injuries occur for various reasons, with trauma being the most common association. Seizures account for <5% of all anterior and posterior shoulder dislocations [3]. A variety of complications may occur following a dislocation event, including vascular or neurologic compromise, which makes timely diagnosis and treatment of these injuries critical to prevent potentially irreversible damage. We present the case of a 17-year-old male who sustained bilateral anterior shoulder dislocations with greater tuberosity fractures secondary to status epilepticus. Both shoulders were successfully reduced as evidenced by post-reduction clinical examination and radiographic findings. The successful reduction of both shoulders described here highlights the effectiveness of prompt intervention. The inability to recognize or perform a closed reduction of a dislocated shoulder in a timely manner increases the risk of having unsuccessful subsequent closed reduction attempts [4]. This case enhances the current orthopedic literature by offering valuable insights into the management of this distinct injury pattern, particularly those associated with seizures. It serves as an illustrative example highlighting the potential for favorable outcomes when these injuries are addressed quickly with appropriate care. The information from this case contributes to the broader understanding of effective strategies in handling and diagnosing such situations, which can enhance the ability of healthcare professionals to provide optimal treatment in future circumstances.
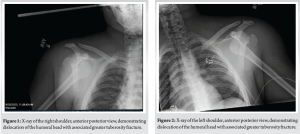
A 17-year-old Caucasian male presented to the emergency department with altered mental status following multiple reported seizure-like episodes at his home. The patient was hemodynamically unstable on presentation and intubated on arrival. Laboratory workup revealed rhabdomyolysis and acute kidney injury. After initial stabilization, careful physical examination was remarkable for subtle prominence in the bilateral deltopectoral regions. He was neurovascularly intact with the exception of decreased sensation in the bilateral axillary nerve distribution. Initial radiographs of the right shoulder revealed anterior dislocation of the humeral head with an avulsion fracture of the humeral greater tuberosity (Fig. 1). Imaging of the left shoulder also revealed an anterior dislocation of the humeral head with an associated greater tuberosity fracture (Fig. 2).
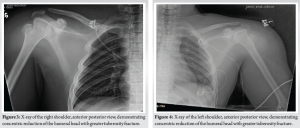
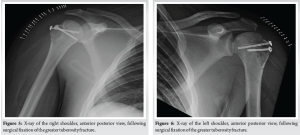
The patient underwent urgent closed reduction of each fracture-dislocation using a traction-countertraction technique. Follow-up imaging revealed appropriate reduction of both dislocations (Fig. 3 and 4). The patient was placed into bilateral slings following successful reduction. Operative stabilization of the patient’s bilateral greater tuberosity fractures was performed following medical optimization. Fracture fixation was achieved with a cannulated screw and suture anchor construct. Both shoulders demonstrated restoration of glenohumeral joint alignment on intraoperative films (Fig. 5 and 6). At the first clinic visit following surgical intervention, the patient was found to have persistent diminished sensation in the bilateral axillary nerve distribution with mild deltoid atrophy. Of note, he was without any further seizure episodes at that time. The patient maintained close follow-up with neurology who continued him on oral valproate regimen for seizure prevention. On further follow-up, he was noted to have modest improvement in sensation in the right and left axillary nerve distribution. Electromyography and nerve conduction studies (EMG/NCS) studies were performed 2 months postoperatively which revealed bilateral axillary nerve palsies. The patient was subsequently started on an intensive physical therapy regimen. Repeat EMG/NCS studies were performed 4 months postoperatively, which were reassuring for ongoing nerve recovery. The patient was last seen in the orthopedic clinic 1 year following surgical intervention. At that time, he was noted to have significant improvement in deltoid strength bilaterally with preserved shoulder range of motion. He was continuing to make progress in physical therapy, and his pain was controlled. There was no evidence of shoulder instability at the final follow-up. The patient had returned to all activities, and he was allowed to follow-up as needed. No further seizure episodes were reported at last follow-up with the Neurology team, which was 1 year from the patient’s initial seizure episode.
Shoulder dislocations can lead to various complications if not treated promptly and appropriately [5]. Anterior dislocation secondary to seizures is an uncommon presentation when compared to posterior dislocation [6], and only a small subset of patients with bilateral anterior shoulder dislocations present with an associated greater tuberosity fracture [7]. As performed in this patient, management of shoulder dislocations includes early reduction and immobilization to minimize complications. Once reduced, surgical treatment may be warranted depending on fracture pattern characteristics and patient factors [8]. Operative fixation remains indicated in this setting of 1st-time anterior shoulder dislocation, but the method of stabilization remains controversial [9,10]. Screw fixation over percutaneous pinning was the stabilization of choice to promote appropriate bone growth and alignment in the setting of shoulder dislocation with combined greater tuberosity fractures, but evidence on management remains limited [11]. Patients who experience shoulder dislocations have a higher risk of recurrent shoulder dislocations and long-term complications [12]. Chronic instability and repeated dislocations can accelerate arthritic changes of the joint surfaces leading to pain, stiffness, and decreased shoulder function over time [13]. In addition, following a shoulder dislocation, the adjacent neurovasculature can be stretched or compressed. If not addressed, this can result in permanent nerve damage or vascular injury and avascular necrosis [5,6,13]. Prolonged dislocation can cause significant damage to the surrounding soft tissues, including ligaments, tendons, and muscles. This can result in increased pain, swelling, and potential compartment syndrome of the upper extremity if not treated in a timely manner [14,15]. Following stabilization of this injury in the setting of status epilepticus, further medication management may be needed to prevent injury recurrence. Intravenous (IV) benzodiazepines, specifically lorazepam, are used as first-line anti-epileptics in the emergent setting of seizure control, and if refractory, a continuous infusion of IV benzodiazepines should be administered [16]. In the workup of identifying the etiology of status epilepticus, it is ideal to administer up to two doses of IV lorazepam within 1 h followed by a non-benzodiazepine, but further administration of anti-seizure medications is not indicated following resolution [17]. It is important to note that the management of these injuries can vary depending on patient-specific factors such as the type of dislocation and the extent of injury. These factors include the patient’s overall health status, pre-existing medical conditions or prior dislocations, age, and anatomical variations. In addition, aspects like the patient’s ability to comply with rehabilitation exercises or overall activity level can impact prognosis. The atypical presentation and distinctive radiographic findings in this patient warrant additional exploration into the early identification and management strategies for bilateral anterior shoulder dislocations in pediatric patients who are in critical status. Considering the significant repercussions associated with delaying reduction of bilateral shoulder dislocations, healthcare workers must maintain a high index of suspicion for this potential injury pattern in the critically ill and intubated patient when the physical examination warrants further workup. 2nd, about control of epilepsy. Because it is very important to obtain stabilization after operation and prevention for recurrence.
The current literature on bilateral anterior shoulder fracture-dislocations in a pediatric patient is scarce. Imaging and appropriate reduction is essential to improve patient outcomes and prevent potentially irreversible complications such as avascular necrosis and neurologic compromise. Treatment involves reduction of the dislocation, managing pain and inflammation, and initiating rehabilitation exercises to strengthen the shoulder and prevent future dislocations. In some cases, surgical intervention may be necessary to address severe injuries, including complicated fractures or recurrent dislocations. This case holds significance due to the rarity of bilateral pediatric shoulder dislocations, which might not be immediately considered by healthcare providers, especially when a patient is intubated or unresponsive and in critical status. Therefore, clinical suspicion of potential shoulder dislocation must be maintained while gathering a thorough patient history and performing a detailed physical examination in initial management of these injuries, especially in pediatric cases. The effects of delayed treatment are more severe in the pediatric patient, where salvage treatment options such as arthroplasty should be avoided if possible. Our case raises awareness about this potential diagnosis and the prompt treatment required to ensure an optimal outcome. Members of the healthcare team must maintain a high clinical suspicion of this injury pattern, especially in the intubated pediatric patient where a physical examination may be limited secondary to their clinical status.
This paper discusses a rare case of bilateral anterior shoulder dislocations with associated greater tuberosity fractures in a 17-year-old male following status epilepticus. Our patient presented with altered mental status, rhabdomyolysis, and acute kidney injury, requiring intubation due to hemodynamic instability. Despite this, his injuries were promptly identified and treated successfully. This case emphasizes the importance of prompt diagnosis and treatment to prevent potentially devastating complications. The unusual presentation described herein warrants further investigation into the management of such cases. A lower threshold to obtain imaging in an unresponsive or critically ill patient may be warranted when history and physical examination are suggestive of potential pathology. This will ultimately allow for appropriate treatment to be delivered with an improvement in patient outcomes and prevention of long-term complications.
References
- 1.Pushpakumara J, Sivathiran S, Roshan L, Gunatilake S. Bilateral posterior fracture-dislocation of the shoulders following epileptic seizures: A case report and review of the literature. BMC Res Notes 2015;8:704. [Google Scholar | PubMed]
- 2.Dao KT, Veedu HKP, Ly B, Zalmay N, Hariprasad R, Eagan M, Ussef N. Two cases of anterior shoulder dislocation and fracture secondary to generalized tonic-clonic seizure. Case Rep Orthop 2024;2024:6652622. [Google Scholar | PubMed]
- 3.Betz ME, Traub SJ. Bilateral posterior shoulder dislocations following seizure. Intern Emerg Med 2007;2:63-5. [Google Scholar | PubMed]
- 4.Meena S, Saini P, Singh V, Kumar R, Trikha V. Bilateral anterior shoulder dislocation. J Nat Sci Biol Med 2013;4:499-501. [Google Scholar | PubMed]
- 5.Ballesteros R, Benavente P, Bonsfills N, Chacón M, García-Lázaro FJ. Bilateral anterior dislocation of the shoulder: Review of seventy cases and proposal of a new etiological-mechanical classification. J Emerg Med 2013;44:269-79. [Google Scholar | PubMed]
- 6.Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl 2009;91:2-7. [Google Scholar | PubMed]
- 7.Siu YC, Lui TH. Bilateral anterior shoulder dislocation. Arch Trauma Res 2014;3:e18178. [Google Scholar | PubMed]
- 8.Schumacher KM, Moravec A, Jonas ME, Tayag DL, Choi JY. Bilateral posterior shoulder fracture dislocations from seizures due to hyponatremia: A case report. JSES Rev Rep Tech 2022;3:94-100. [Google Scholar | PubMed]
- 9.Godin J, Sekiya JK. Systematic review of rehabilitation versus operative stabilization for the treatment of first-time anterior shoulder dislocations. Sports Health 2010;2:156-65. [Google Scholar | PubMed]
- 10.Nazzal EM, Herman ZJ, Engler ID, Dalton JF, Freehill MT, Lin A. First-time traumatic anterior shoulder dislocation: Current concepts. J ISAKOS 2023;8:101-7. [Google Scholar | PubMed]
- 11.Mansi Z, Abdelkader T, Islem C, Wajdi C, Ali H, Wael G. Bilateral combined fracture of the greater tuberosity with anterior internal shoulder dislocation. Int J Surg Case Rep 2024;121:109914. [Google Scholar | PubMed]
- 12.Stanislavsky A, Sofiane Z, Ranchod A, et al. Anterior Shoulder Dislocation. Available from: https://radiopaedia.org [Last accessed on 2023 Aug 13]. [Google Scholar | PubMed]
- 13.Hernigou P, Hernigou J, Scarlat M. Shoulder osteonecrosis: Pathogenesis, causes, clinical evaluation, imaging, and classification. Orthop Surg 2020;12:1340-9. [Google Scholar | PubMed]
- 14.Benabbouha A, Benyass Y, Sallahi H, Margad O. An exceptional challenging case: Anterior shoulder dislocation with ipsilateral humeral shaft fracture complicated with an upper extremity compartment syndrome. Int J Surg Case Rep 2023;106:108237. [Google Scholar | PubMed]
- 15.Yen CY, Yeh WL, Tu YK. Inferior dislocation of the glenohumeral joint combined with the compartment syndrome of the upper arm: Case report. Changgeng Yi Xue Za Zhi 1998;21:358-61. [Google Scholar | PubMed]
- 16.16. Kim D, Kim JM, Cho YW, Yang KI, Kim DW, Lee ST, et al. Antiepileptic drug therapy for status epilepticus. J Clin Neurol 2021;17:11-9. [Google Scholar | PubMed]
- 17.Kienitz R, Kay L, Beuchat I, Gelhard S, von Brauchitsch S, Mann C, et al. Benzodiazepines in the management of seizures and status epilepticus: A review of routes of delivery, pharmacokinetics, efficacy, and tolerability. CNS Drugs 2022;36:951-75. [Google Scholar | PubMed]









