Arthroscopic release of FHL tendon sheath has proven to be a useful and minimally invasive technique to approach Hallux Saltans pathology, enabling fast return to sport and long-lasting results.
Dr. Ainú Verdini Gasti, Orthopaedics and Traumatology Unit, Hôpital Pourtalès, Neuchâtel, Switzerland. E-mail: ainu.verdini@gmail.com
Introduction: Hallux Saltans is an uncommon pathological entity mostly encountered in correlation with physical activities such as ballet dancing or football. It is a stenosing tenosynovitis of the flexor hallucis longus (FHL) tendon, relating to inflammation and fibrous metaplasia of the pulleys. This disorder can cause pain and hinder sport career progression.
Case Report: A 16-year-old female, training to become a professional ballet dancer, presented with a 2-year history of pain and swelling of the right ankle, associated with triggering of the hallux and audible cracking at active extension. After a magnetic resonance imaging (MRI) diagnosis of tenosynovitis of right FHL tendon, the patient was treated operatively by posterior arthroscopic tenolysis of the FHL, which was entrapped by the fibrous tissue of the tendon sheath. During post-operative period, the patient presented an immediate relief from triggering of the hallux. She was able to start dancing again 6 weeks after surgery and her right hallux remained asymptomatic. However, about 8 months after surgery, she presented with the same triggering symptoms on the contralateral side. The pain, blocking, and triggering of her left hallux lead to an MRI investigation and once the diagnosis of tenosynovitis of the FHL was confirmed, an arthroscopic tenolysis was performed again. The treatment relieved the patient immediately. On follow-up, at 5 years after surgery on the right side and 4 years after left one, the patient remained asymptomatic on both sides. She keeps dancing, but stopped the professional career for personal reasons.
Conclusion: The condition known as trigger hallux is a rare yet debilitating pathology. When present, it should be taken seriously, and further radiological investigations should be performed to diagnose any potential tenosynovitis of the FHL. Arthroscopic release of FHL tendon sheath has proven to be a useful and minimally-invasive technique to approach hallux saltans pathology in a semi-professional young ballet dancer, enabling fast return to sport and long lasting results.
Keywords: Hallux saltans, flexor hallucis longus tenosynovitis, arthroscopic tenolysis.
As previously defined in literature, hallux saltans is a phenomenon of thickening and compression of the flexor hallucis longus (FHL) tendon that is mainly seen in young athletes, especially ballet dancers, tennis, and football players [1-5]. In this particular case, stenosing tenosynovitis is leading to pain and a remarkable problem in sporting career prosecution. The stressful repeated joint movement of the foot and ankle causes an inflammation of the FHL tendon that is heading, in association with multiple intra-tendon partial tears, to the formation of nodules and a thickening of the tendon, resulting in trigger hallux problem [6]. Diagnosis is posed by magnetic resonance imaging (MRI) or ultrasonography investigation; dynamic ultrasound may provide a useful evidence of the trapping and triggering mechanism. In our report, we present a case of bilateral hallux saltans in a semi-professional ballet dancer, its endoscopic treatment, and a follow-up of 5 years for the right side and 4 years for the left side.
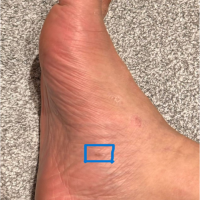
A 16-year-old healthy, non-smoking, female ballerina, heading for a professional career, presented with a 2-year history of pain and joint crepitus concerning her right medial malleolus. The patient described a painful sensation of swelling of the medial retromalleolar region on physical exertion. The pain was relieved at rest. The symptomatology had no traumatic origin and was not associated with instability. Clinical examination revealed no antalgic gait, right ankle and foot range of motion was preserved and symmetric, and there were no neurovascular abnormalities. We did however note a hollow longitudinal arch and a flattened transverse arch, without complains of metatarsalgia or discomfort at the palpation of metatarsal heads. Pathological findings were present during the mobilization of the patient’s hallux. A movement of deep flexion was triggering crepitus, audible, and palpable in the medial malleolus region, followed by a sensation of trapping of the toe (Fig. 1). The extension caused a similar painful cracking (Fig. 2).

Initial plain radiography detected a hollow right foot without others anomalies such as degenerative problems or the presence of os trigonum.
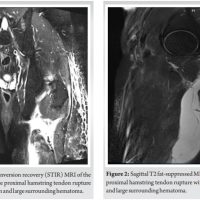
The following MRI showed a thickening of right FHL tendon extending to the portion located distally to the posterior talar process, associated with a tenosynovitis of its entire length and a partial tear of 25% of its thickness (Fig. 3 and 4). 
Due to the troublesome symptoms and their impact on patient’s sportive activity, the surgical indication was confirmed and written informed consent was obtained. The day of the surgery, the patient was placed in prone position and a spinal anesthesia was provided as well as a classic disinfection and a prophylactic administration of 1.5 g of Cefuroxime. The right leg was exsanguinated and a tourniquet was adjusted to 280 mmHg. Two posterior portals were established, at the medial and lateral side of right Achille’s tendon, the tibial nerve and the FHL tendon were localized and protected during the whole surgery. Tibiotalar and subtalar joint preparation was performed by shaver. An important fibrous thickening of the FHL tendon could be endoscopically observed (Fig. 5). The tendon was found to be intact at its proximal part. On testing the right tendon’s mobility, it was found that the prominence could not move proximally to the retinaculum without an active contraction of FHL. The fibrous thickening around the tendon was then released by shaver (Fig. 6). The FHL could finally slide freely and no stenosis or triggering was found at further tendon motion (Fig. 7). Following the operation, free mobilization was encouraged from day 1, avoiding right hallux efforts, and sport could be resumed 6 weeks later, and 12 weeks for “en pointe” position.

At the first follow-up, 5 weeks after surgery, the patient complained only of a minimal stiffness of her right ankle. The trapping sensation had disappeared, and she had no more cracking. The right hallux and ankle mobility were normal on physical examination, and there were no triggering phenomena. At 8-month follow-up, the patient had returned to dancing as before the intervention, and the triggering problem of her right hallux had resolved, as well as the pain. However, the patient began to present the same triggering symptoms on the contralateral side. After a clinical examination and the radiological investigations of her left foot, the diagnosis of stenosing tenosynovitis of left FHL tendon was confirmed and the surgical indication to perform an arthroscopic release of the trapped tendon on the left side was clear. The same surgical procedure of her contralateral foot was discussed with the patient, and written informed consent was obtained. The day of the intervention, the same positioning of the patient and surgical techniques as the first operation was adopted. During the arthroscopic procedure on the left side, a fibrous thickening around the tendon, similar to the first procedure was visualized (Fig. 8). It was released by shaver (Fig. 9) and the FHL could finally slide freely (Fig. 10). No stenosis or triggering was found at further tendon motion.

After the surgery, free mobilization was again encouraged from day 1, avoiding right hallux efforts and sport for 6 weeks. At present, 5 years from right and 4 years from left FHL surgery, the patient remains asymptomatic on both sides; she is still dancing, despite stopping her semi-professional career for other personal reasons.
Hallux Saltans condition is known to be mainly caused by a fibrous thickening of the pulley structure at the level of sustentaculum tali, heading to an entrapment of FHL tendon. Locking of the tendon may also be caused by compression due to bone structures, such as os Trigonum and sesamoids [7]. Despite literature describing cases of entrapment of the FHL tendon in non-athletic patients, without any apparent predisposing factors [8], classical ballet dancers seem to be most at risk of developing this pathology, due to the stressful dancing position on the tips of the toes “en pointe” that may lead to inflammation, in certain cases, to a stenosing tenosynovitis of FHL and the associated fibrous thickening [9]. To provide context for our case, we reviewed similar reports in the literature. The table below (Table 1) lists relevant case reports of bilateral Hallux Saltans published in the last 10 years, offering references to other works that have explored this condition in various patient populations. This helps to frame our case within the broader body of research on Hallux Saltans.

The advantages of arthroscopic surgery include a good direct and dynamic visualization of FHL lesions, the minimal invasiveness of the surgical intervention, and the dynamic pathology of the lesion can be easily understood and assessed. It is furthermore possible to examine and treat other intra-articular and peri-articular structures better with this method than in open surgery [10].
The condition known as trigger hallux is a rare yet debilitating pathology. When present, it should be taken seriously, and further radiological investigations should be performed to diagnose any associated tenosynovitis of the FHL. Good results with a relatively minimally invasive technique may be obtained with endoscopic treatment of hallux saltans. Mobility can be re-acquired soon and high-level sport resumption can be expected within months. Arthroscopic technique however requires careful handling because of the proximity between the tibial nerve and the FHL tendon. The risk-benefit ratio, including the classical surgical risks as like as infection, cicatrisation problems, and pain, should always be considered.
The pathology of trigger hallux due to a tenosynovitis of the FHL, it can be treated through arthroscopic tenolysis, yielding satisfactory and long lasting results.
References
- 1.Lereim P. Trigger toe in classical-ballet dancers. Arch Orthop Trauma Surg (1978) 1985;104:325-6. [Google Scholar | PubMed]
- 2.Theodore GH, Kolettis GJ, Micheli LJ. Tenosynovitis of the flexor hallucis longus in a long-distance runner. Med Sci Sports Exerc 1996;28:277-9. [Google Scholar | PubMed]
- 3.Cooper ME, Wolin PM. Os trigonum syndrome with flexor hallucis longus tenosynovitis in a professional football referee. Med Sci Sports Exerc 1999;31:S493-6. [Google Scholar | PubMed]
- 4.Moorman CT 3rd, Monto RR, Bassett FH 3rd. So-called trigger ankle due to an aberrant flexor hallucis longus muscle in a tennis player. A case report. J Bone Joint Surg Am 1992;74:294-5. [Google Scholar | PubMed]
- 5.Hamilton WG. Posterior ankle pain in dancers. Clin Sports Med 2008;27:263-77. [Google Scholar | PubMed]
- 6.Kolettis GJ, Micheli LJ, Klein JD. Release of the flexor hallucis longus tendon in ballet dancers. J Bone Joint Surg Am 1996;78:1386-90. [Google Scholar | PubMed]
- 7.Tokgöz MA, Kanatlı U, Vural A, Ataoğlu MB, Yapar A, Ergişi Y. Endoscopic treatment of bilateral hallux saltans in an ordinary woman. Eklem Hastalik Cerrahisi 2019;30:322-4. [Google Scholar | PubMed]
- 8.Chinzei N, Kanzaki N, Nagai K, Haneda M, Yamamoto T, Kuroda R. Posterior ankle arthroscopy for flexor hallucis longus entrapment: A case report. J Orthop Case Rep 2021;11:70-4. [Google Scholar | PubMed]
- 9.Tudisco C, Puddu G. Stenosing tenosynovitis of the flexor hallucis longus tendon in a classical ballet dancer. A case report. Am J Sports Med 1984;12:403-4. [Google Scholar | PubMed]
- 10.Zwiers R, Wiegerinck JI, Murawski CD, Smyth NA, Kennedy JG, Van Dijk CN. Surgical treatment for posterior ankle impingement. Arthroscopy 2013;29:1263-70. [Google Scholar | PubMed]
- 11.Rohan, Sundarapandian R, Pillai A. A rare case of hallux saltans treated using ultrasound-guided intralesional steroid injection: A case report. J Orthop Case Rep 2024;14:52-5. [Google Scholar | PubMed]
- 12.Schindler M, Reinhard J, Grifka J, Leiss F, Schwarz T. Hallux saltans - seltene diagnose, oft übersehen [Hallux saltans-rare diagnosis, often overlooked]. Orthopadie (Heidelb) 2022;51:939-42. [Google Scholar | PubMed]
- 13.Barchi EI, Swensen S, Dimant OE, McKay TE, Rose DJ. Flexor hallucis longus tenolysis and tenosynovectomy in dancers. J Foot Ankle Surg 2022;61:84-7. [Google Scholar | PubMed]
- 14.Wentzell M. Conservative management of a chronic recurrent flexor hallucis longus stenosing tenosynovitis in a pre-professional ballet dancer: A case report. J Can Chiropr Assoc 2018;62:111-6. [Google Scholar | PubMed]
- 15.Martinez-Salazar EL, Vicentini JR, Johnson AH, Torriani M. Hallux Saltans due to stenosing tenosynovitis of flexor hallucis longus: Dynamic sonography and arthroscopic findings. Skeletal Radiol 2018;47:747-50. [Google Scholar | PubMed]