This case highlights the importance of considering rare bone tumors, such as chondroblastoma, in pediatric patients presenting with persistent joint pain and functional limitations. Early diagnosis through comprehensive imaging is crucial for determining the appropriate treatment approach. En bloc resection with allograft and fixation, though not commonly used in these cases, proved to be an effective strategy for restoring joint morphology and function, emphasizing the need for individualized treatment plans based on tumor extent and location.
Dr. Omar Fernando Rodríguez-Rodríguez, Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE). Regional Hospital Monterrey, Department of Traumatology and Orthopedics, Adolfo López Mateos 122, Col. Burócratas Federales, 64380 Monterrey, N.L.México. E-mail: dr.omarrodriguezro@gmail.com
Introduction: This case is important because it highlights a rare presentation of chondroblastoma, given the tumor’s male predominance and its uncommon occurrence in females. The proximal humerus is one of the less frequently reported sites for chondroblastoma, additionally, the tumor exhibited aneurysmal changes, a known risk factor for recurrence. This case contributes to the orthopedic literature by providing insight into the clinical and imaging features, challenges in diagnosis, and management strategies for this rare tumor.
Case Report: A 12-years-old girl from México, presented with progressive right shoulder pain after a traction injury, clinical examination showed limited abduction and a palpable mass, imaging and pathology tests revealed a lesion in the proximal humerus. Due to the tumor’s extent, en bloc resection with an allograft and fixation was performed, a procedure not commonly used in these patients, to restore morphology and function.
Conclusion: This case underscores the importance of early recognition and a multidisciplinary approach to managing chondroblastoma, especially in atypical presentations, such as in young females. En bloc resection combined with allograft reconstruction provided a favorable clinical outcome, minimizing recurrence risk and preserving joint function. This report contributes to the orthopedic literature by documenting a rare presentation and emphasizing the critical role of individualized surgical strategies and post-operative rehabilitation in achieving optimal outcomes.
Keywords: Chondroblastoma, pediatric tumor, en bloc resection, orthopedic oncology.
Chondroblastoma is a rare, benign bone tumor accounting for approximately 1% of all bone tumors. It primarily affects the epiphysis of long bones, with a predilection for the proximal femur, proximal humerus, and proximal tibia. Most cases occur in adolescents and young adults, with a male predominance. Symptoms typically include localized pain and restricted joint mobility [1]. The following case report describes a pediatric patient diagnosed with a chondroblastoma in the proximal humerus, emphasizing the diagnostic and therapeutic approach.
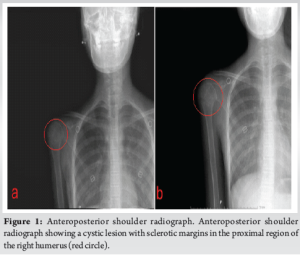
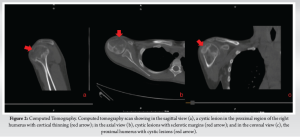
A 12-year-old female from México, presented to the emergency room with sudden onset right shoulder pain following a linear traction injury to her right arm. The pain was initially diffuse, relieved by rest, and exacerbated by movement. After 2 months, the pain intensified and persisted despite rest, prompting the patient to seek further medical attention. Radiographs revealed a lesion in the proximal humerus without signs of a recent fracture. The patient was referred for an outpatient consultation for further evaluation. One month later, a comprehensive physical examination revealed increased volume in the proximal right humerus, accompanied by a palpable, indurated mass. Shoulder abduction was limited to 60°, while both internal and external rotations were preserved. Comparative shoulder radiographs and a computed tomography (CT) scan were ordered for further assessment (Fig. 1 and 2).
Diagnostic Assessment
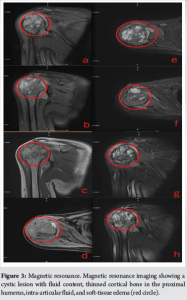
Four months after the initial evaluation, a CT scan revealed a multilobulated, expansile tumor in the humeral head, measuring 5 × 3 cm, with cortical thinning and internal sclerotic septa (Fig. 2). A clinical suspicion of a tumor was raised, prompting the scheduling of an incisional biopsy along with a metastatic bone survey to rule out systemic involvement. The biopsy confirmed the diagnosis of a chondroblastoma in the proximal humerus. In addition, magnetic resonance imaging (MRI) showed a heterogeneous cystic lesion to the humeral head, measuring 4.5 × 4.1 × 5.1 cm. The lesion exhibited thin septations, fluid-fluid levels, and cortical thinning (Fig. 3).
Therapeutic Intervention
Surgical intervention was performed 10 months following the initial evaluation. The patient was positioned in a beach-chair posture, and a 12 cm incision was made using a deltopectoral approach. The lesion was resected en bloc. An allograft was prepared and secured with a five-hole anatomical distal tibia plate and screws. Intraoperative radiographs confirmed the correct placement of the graft. Soft-tissue reconstruction included tendon repair and capsular plication (Fig. 4). The procedure was completed without complications, and the resected specimen was sent for histopathological analysis.
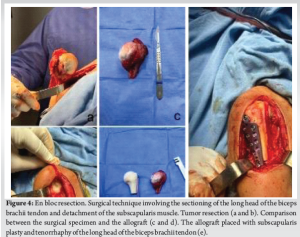
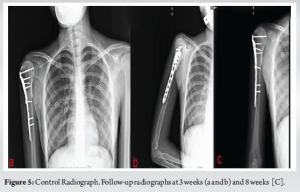
The patient was discharged with instructions for daily wound care, suture removal in 15 days, and immobilization until further medical guidance. At the first post-operative follow-up, 1 month later, the patient was asymptomatic, with a well-healed surgical wound and no signs of infection. Shoulder abduction was limited to 40°, with reduced muscle strength and restricted internal and external rotation. Histopathological analysis confirmed the diagnosis of chondroblastoma with aneurysmal changes. Currently, at the 6-month follow-up, the patient remained asymptomatic, with a healed surgical site. However, joint mobility and strength were still limited to 60°, and the patient continue with physical rehabilitation (Fig. 5).
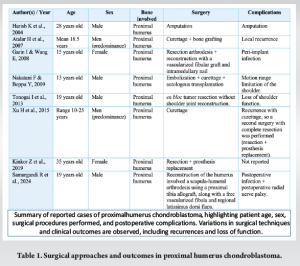
Chondroblastoma is a rare, benign tumor primarily affecting the epiphyseal regions of long bones, is a slow-growing tumor that rarely involves soft tissues or causes cortical destruction [2]. The average age of onset is 12.5 years, with a higher incidence in males. Pain is typically the first presenting symptom. The most common location is the epiphysis of long bones (68%), with the proximal humerus being the third most frequent site. On average, there is a 6.5-month delay between symptom onset and diagnosis. Complete curettage is generally recommended as the treatment of choice to minimize recurrence risk [3]. The case presented aligns with the literature, except for the fact that the patient was female. Given available resources, an allograft and distal tibia plate were utilized to provide the optimal treatment outcome for the patient. This case was managed in a tertiary-level hospital in México. This clinical presentation includes localized pain and, in some cases, functional impairment. Imagining plays a critical role in diagnosis, typically can appear as a lytic lesion with well-defined margins, varying in size from 1 to 4 cm, the involvement of soft-tissues causing bone edema and joint effusion is characteristic. In the proximal humerus, chondroblastoma may present with poorly defined borders, which can resemble a malignant lesion. Between 46 and 59.4% of patients may present with calcifications detected on imaging studies. The imaging differential diagnosis includes chondrosarcoma, osteomyelitis, and giant cell tumor. Histopathological confirmation is essential [4,5]. It is crucial to establish a comprehensive treatment plan, as insufficient curettage is a known risk factor for the recurrence of chondroblastoma. Treatment typically involves curettage and bone grafting using curettage, the recurrence rate ranges from 8 to 30%. Contributing factors include patient age, the presence of an aneurysmal cystic component, anatomical location, and inadequate surgical technique [7]. However, en bloc resection is recommended for larger or more aggressive lesions. In this case, en bloc resection was selected due to the tumor’s extent, and the histopathological report revealed aneurysmal changes, which are considered a risk factor for recurrence [8]. Treatment with allografts provides good outcomes. After 1 year, patients are asymptomatic, show no radiographic evidence of recurrence, and the allograft is found to be well-integrated [9]. Physical rehabilitation remains crucial for restoring joint function and strength postoperatively. Although the tumor is radiosensitive, it is not recommended as a first-line treatment due to the favorable outcomes achievable through surgery. Radiotherapy is recommended only when surgical intervention is not possible [10]. En bloc resection is a relevant strategy due to the lower recurrence rate compared to others such as curettage or other techniques in patients with proximal humeral chondroblastoma, unlike other locations where, for example, curettage can be a good option with minimal risk of recurrence or complications [11-16]. Other technique that has been used in addition to curettage is the arthroplasty of the shoulder using a vascularized fibula graft that it is used when there is a massive defect of the proximal humerus, however, both curettage and fibula grafting present complications (Table 1). Xu H et.al. describe a report of 126 patients with chondroblastoma, only 11 patients had it in the proximal humerus. Of the 126, 6 patients had recurrence, of these, 5 had chondroblastoma in the humerus, this was because they were first treated with curettage, later they had a complete resection and 0% recurrence was seen, however, most used a prosthesis after the resection, and none reported a reconstruction of the adjacent muscles and the glenohumeral joint [14].
This case is relevant due to the reconstruction of the muscular tissues, allowing the patient a functionality as close to normal as possible, while other cases where the invasion of chondroblastoma does not allow the reconstruction of the muscular tissue, preventing the return to normal daily activity. However, it is essential to mention that in reports where muscle tissue reconstruction was not performed it is generally not due to a lack of material or surgical skill. In most of these cases, the chondroblastoma caused extensive damage, making tissue reconstruction unfeasible [13-18]. The glenohumeral joint, along with its muscular envelope, plays a crucial role in overall body functionality. The muscles involved are essential for a dynamic movement, providing stability and coordination. Therefore, reconstructing the joint as close to normal as possible is fundamental to restoring function and facilitating the patient’s reintegration into daily life.
This case highlights the importance of a multidisciplinary approach in diagnosing and managing chondroblastoma. Early recognition, appropriate imaging, and timely surgical intervention are pivotal in achieving favorable outcomes in pediatric patients with this rare tumor. With this patient, a low risk of recurrence is expected, along with a functional range of motion and no need for further surgical interventions.
Chondroblastoma, though rare, should be considered in the differential diagnosis of adolescents presenting with persistent joint pain and limited mobility, particularly when involving the epiphyseal regions of long bones. Timely diagnosis through imaging and histopathological confirmation is crucial to guide appropriate management. En bloc resection combined with allograft reconstruction is an effective surgical strategy for larger or aggressive lesions, minimizing recurrence risk and preserving joint function. A multidisciplinary approach, including early rehabilitation, is essential to optimize functional recovery and long-term outcomes in pediatric patients.
References
- 1.Sailhan F, Chotel F, Parot R. Chondroblastoma of bone in a pediatric population. J Bone Joint Surg Am 2009;91:2159-68. [Google Scholar | PubMed]
- 2.Atalar H, Basarir K, Yildiz Y, Erekul S, Saglik Y. Management of chondroblastoma: Retrospective review of 28 patients. J Orthop Sci 2007;12:334-40. [Google Scholar | PubMed]
- 3.Huang C, Li XM, Fu G, Yang Z. Chondroblastoma in the children treated with intralesional curettage and bone grafting: Outcomes and risk factors for local recurrence. Orthop Surg 2021;13:2102-10. [Google Scholar | PubMed]
- 4.Blancas C, Llauger J, Palmer J, Valverde S, Bagué S. Manifestaciones radiológicas del condroblastoma. Radiologia 2008;50:416-23. [Google Scholar | PubMed]
- 5.Crim JR, Gold RH, Mirra JM, Eckardt J. Case report 748: Chondroblastoma of the femur with an aneurysmal bone cyst. Skeletal Radiol 1992;21:403-5. [Google Scholar | PubMed]
- 6.Garin IE, Wang EH. Chondroblastoma. J Orthop Surg (Hong Kong) 2008;16:84-7. [Google Scholar | PubMed]
- 7.Unni KK, Inwards CY. Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases. 6th ed. Philadelphia: : Lippincott Williams & Wilkins; 2010 ???. [Google Scholar | PubMed]
- 8.Xu H, Nugent D, Monforte HL, Binitie OT, Ding Y, Letson GD, et al. Chondroblastoma of bone in the extremities: A multicenter retrospective study. J Bone Joint Surg Am 2015;97:925-31. [Google Scholar | PubMed]
- 9.Fitzgerald J, Broehm C, Chafey D, Treme G. Chondroblastoma of the knee treated with resection and osteochondral allograft reconstruction. Case Rep Orthop 2014;2014:543959. [Google Scholar | PubMed]
- 10.Dahlin DC, Ivins JC. Benign chondroblastoma. A study of 125 cases. Cancer 1972;30:401-13. [Google Scholar | PubMed]
- 11.Garin IE, Wang EH. Chondroblastoma. J Orthop Surg (Hong Kong). 2008;16(1):84–87. doi:10.1177/230949900801600119. [Google Scholar | PubMed | CrossRef]
- 12.Harish K, Janaki MG, Alva NK. "Primary" aggressive chondroblastoma of the humerus: a case report. BMC Musculoskelet Disord. 2004;5:9. doi:10.1186/1471-2474-5-9. [Google Scholar | PubMed | CrossRef]
- 13.Atalar H, Basarir K, Yildiz Y, Erekul S, Saglik Y. Management of chondroblastoma: retrospective review of 28 patients. J Orthop Sci. 2007;12(4):334–340. doi:10.1007/s00776-007-1141-2. [Google Scholar | PubMed | CrossRef]
- 14.Xu H, Ding Y, Niu X, et al. Chondroblastoma of bone in the extremities: a multicenter retrospective study. J Bone Joint Surg Am. 2014;96(12):925–931. doi:10.2106/JBJS.N.00992. [Google Scholar | PubMed | CrossRef]
- 15.Nakatani F, Beppu Y. A case of locally advanced chondroblastoma in the proximal humerus. Jpn J Clin Oncol. 2009;39(1):70. doi:10.1093/jjco/hyn149. [Google Scholar | PubMed | CrossRef]
- 16.Tonogai I, Takahashi M, Manabe H, et al. A massive chondroblastoma in the proximal humerus simulating malignant bone tumors. Case Rep Orthop. 2013;2013:673576. doi:10.1155/2013/673576. [Google Scholar | PubMed | CrossRef]
- 17.Samargandi R, Bernard M, Miquelestorena-Standley E, Le Nail LR. Efficacy of denosumab treatment for lung metastasis secondary to proximal humerus chondroblastoma. Saudi Med J. 2024;45(6):633–638. doi:10.15537/smj.2024.45.6.20230720. [Google Scholar | PubMed | CrossRef]
- 18.Zdeněk K, Petr G, Zuzana Š, Zuzana V, Zdeněk M. Chondroblastoma-like primary malignant giant cell tumor of the humerus: a case report. Cesk Patol. 2019;55(1):42–47. [Google Scholar | PubMed]








