Less invasive percutaneous retrograde pinning and early post-operative rehabilitation for metacarpal shaft fractures can provide good clinical outcomes, especially for young patients.
Dr. Takahiro Ushijima, Department of Orthopaedic Surgery, Mizoguchi Hospital, Tenjin, Chuo-ku, Fukuoka City, Japan. E-mail: ushishi0908@gmail.com
Introduction: Surgical treatment should be considered for metacarpal fractures that have severe angulation or shortening. Percutaneous pinning is a useful technique in that it is minimally invasive. Insertion of Kirschner wires using retrograde pinning is easier than that using antegrade or transverse pinning. On the other hand, anterograde pinning is also used for metacarpal shaft and neck fractures, but some complications such as perforation of the metacarpal head or laceration of the extensor tendons can occur. The purpose of this study is to evaluate the functional outcomes of simple retrograde pinning.
Materials and Methods: Thirteen patients (15 fingers) with simple metacarpal shaft fractures were enrolled in this prospective study. All patients were treated using percutaneous retrograde pinning following a brachial plexus block. Two intramedullary Kirschner wires were inserted from the metacarpal head to its base. Clinical outcomes included range of motion (ROM), post-operative complications, and evaluation using the Quick Disabilities of the Arm, Shoulder, and Hand score at final follow-up.
Results: ROM in extension/flexion for each joint at the final follow-up was: Metacarpal phalangeal joint 3.1°/87.1°; proximal interphalangeal joint 2.0°/103.3°; and DIP joint 0°/74.1°. The percent total active ROM was 91.9% and the Quick-DASH score was 2.7 out of 100. Pin tract infections occurred in two fingers and were treated with oral antibiotics.
Conclusions: In this study, retrograde Kirschner wire fixation was an acceptable technique for the treatment of displaced metacarpal fractures. This simple technique is suitable, especially for young patients in whom fractures are extraarticular and simple. It can correct deformity less invasively and provide good clinical outcomes.
Keywords: Metacarpal fracture, retrograde, percutaneous pinning.
Various surgical methods for metacarpal shaft fractures have been reported and could provide satisfactory clinical outcomes. Open reduction and internal fixation with a locking plate or lag screws is the usual operative treatment, allowing rigid fixation and early mobilization [1]. However, a conspicuous scar on the dorsal side of the hand and adhesion of the extensor tendon can occur. Percutaneous pinning with Kirschner wires is a less invasive and more versatile technique also common for metacarpal fractures. Anterograde pinning reported by Foucher [2] is used widely for metacarpal shaft and neck fractures, but some complications such as perforation of the metacarpal head or laceration of the extensor tendons can occur [3]. Some studies reported retrograde pinning can lead to a good range of motion (ROM) and clinical outcomes [4-6]. Lord reported retrograde pinning for metacarpal fractures, but joint stiffness occurred because it involving the extensor complex, such as tendons and the sagittal band [4]. We consider that percutaneous retrograde pinning for metacarpal shaft fractures is a simple and easy technique; therefore it can be one of the useful techniques if some tips are taken care. Here, we retrospectively investigated the outcomes of metacarpal shaft fractures treated by retrograde percutaneous pinning.
This research has been approved by the institutional review board of the authors’ affiliated institutions. Informed consent was obtained from all patients. Thirteen patients (15 fingers) with metacarpal shaft fractures who underwent surgery by retrograde percutaneous pinning from 2014 to 2022 were followed for at least 3 months. Clinical evaluations included patient characteristics, as well as type and location of fracture (Table 1). ROM after surgery, post-operative complications, and the Quick Disabilities of the Arm, Shoulder, and Hand (Quick DASH) score were evaluated. Radiological assessment including the dorsal angulation and shortening at the fracture site was performed by X-ray picture at final follow-up. Dorsal angulation was measured with an oblique view for the 4th and 5th finger metacarpal bones and a lateral view for 2nd and 3rd finger metacarpal bones. Shortening displacement was assessed with the same view. The length between the metacarpal base and head was measured and corrected with an adjacent non-injured metacarpal shaft.

Operations were carried out using a brachial plexus block for anesthesia. Percutaneous reduction was performed with point-forceps. Two Kirschner wires (1.2 mm) were inserted with the metacarpal phalangeal (MP) joint in a flexion position from each side of the metacarpal head to avoid damage to the extensor tendon. Intramedullary Kirschner wires were inserted to the base of the metacarpal subchondral bone or beyond the carpometacarpal joint to prevent post-operative shortening dislocation and were cut above the skin. Finger alignment was confirmed by observing finger flexion. Post-operatively, a short arm splint in the intrinsic-plus position was applied for all patients. A knuckle splint was made within 1 week and an active range of finger motion exercises was started as soon as possible under the supervision of a hand therapist (Fig. 1). MP joint contracture and adhesion of extensor tendon could be prevented by early exercise. The Kirschner wires and splint were removed after the bridging callus became mature. A passive ROM was started after the removal of the Kirschner wires. High loading of the affected limb, such as muscle training and sports activity was allowed 3 months after surgery.

Kirschner wires and knuckle splint were removed 26–59 days (mean 36.9 days) after surgery. The patients were followed an average of 118.9 (90–215) days after surgery. ROM in extension/flexion for each joint at final follow-up was: MP joint 3.1° (0–16o) /87.1° 78–98o); proximal interphalangeal (PIP) joint 2.0° (0–10o)/103.3° (90–112o); and distal interphalangeal (DIP) joint 0°/74.1° (60–80o). The percent total active ROM was 91.9% (77.2–100%) and the Quick-DASH score was 2.7 (0–9.1) out of 100. Radiographic bone union was achieved in all patients. Residual dorsal angulation was 3.4° (0–20o). The shortening displacement at the final follow-up was 1.0 mm (0–2.9 mm). Both parameters tend to be large in long oblique or spiral fracture. Pin tract infections occurred in two fingers and were treated with oral antibiotics. Post-operative complications such as non-union and malalignment of the fingers did not occur.
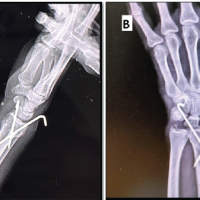
Case 1
An X-ray of a 23-year-old female who had injured her left hand revealed an oblique fracture of the 3rd and 4th metacarpal bones (Fig. 2a). Operation was performed 2 days after injury (Fig. 2b). The Kirschner wires were removed 39 days after surgery. Three months after surgery, an X-ray showed the union of the fracture (Fig. 2c). Dosal angulation was 0.8° for 3rd metacarpal bone and 0.7° for 4th metacarpal bone. Shortening displacement was 0.8 mm for the 3rd metacarpal bone and 0.5 mm for the 4th metacarpal bone. The patient had no pain, and the ROM for each joint of the 3rd metacarpal was: MP joint 0°/86°; PIP joint 0°/112°; DIP joint 0°/80°; and total percent total active motion 94.6%. For the 4th metacarpal, ROM was: MP joint 0°/88°; PIP joint 0°/110°; DIP joint 0°/82°; and percent total active motion 97.2%. The Quick-DASH score was 0.

Case 2
An X-ray of a 20-year-old female who had injured her right hand revealed a transverse fracture of the 5th metacarpal bones (Fig. 3a). Operation was performed 13 days after injury (Fig. 3b). The Kirschner wires were removed 43 days after surgery. Four months after surgery, an X-ray showed the union of the fracture (Fig. 3c). Dosal angulation was 0°, and shortening displacement was 0 mm. The patient had no pain, and the ROM was: MP joint 0°/88°; PIP joint 0°/110°; DIP joint 0°/82°; and total percent total active motion 97.2%. The Quick-DASH score was 2.3.

Case 3
An X-ray of a 20-year-old female who had injured her left hand revealed a long spiral fracture of the 4th metacarpal bones (Fig. 4a). Operation was performed 6 days after injury (Fig. 4b). The Kirschner wires were removed 36 days after surgery. Three months after surgery, an X-ray showed the union of the fracture (Fig. 4c). Dosal angulation was 7°, and shortening displacement was 3.8 mm. The patient had no pain, and the ROM was: MP joint 0°/82°; PIP joint 0°/106°; DIP joint 0°/76°; and total percent total active motion 98.5%. The Quick-DASH score was 0.

Metacarpal fractures are frequently encountered in hand fractures [7]. Most fractures can be treated with closed reduction and cast immobilization, resulting in good function [8]. However, palmar dislocation of >30° and shortening of >5 mm could affect extension and flexion of the fingers [9]. In these cases, surgical treatment is indicated. Many factors are considered in choosing the surgical methods, including the type of fracture, deformity, extent of soft tissue damage, and the patient’s age and sex. Percutaneous pinning for metacarpal shaft fractures is common because it is less invasive and more versatile. Some techniques have been reported to prevent post-operative contracture. The Bouquet method for 5th metacarpal neck fractures reported by Foucher is effective because it can fix the fracture site without MP joint damage [2]. This technique could result in better outcomes than other percutaneous pinning techniques, especially for metacarpal neck fractures [10]. van Bussel et al. also reported that the antegrade intramedullary Kirschner wire fixation technique for metacarpal shaft fractures results in excellent functional outcomes [11]. However, some complications were reported [3] and it is not suitable except for the 5th metacarpal because it is close to the common extensor digitorum. Moon et al reported a transverse technique for metacarpal fractures [12]. This technique has the advantage that the Kirschner wires do not interfere with the extensor complex around the MP joint. However, it is difficult to control rotational displacement because the suitable range of Kirschner wire insertion is narrow. Some studies report retrograde pinning. This technique is useful in that it is easy to insert the Kirschner wires. Kim reported that antegrade intramedullary pinning achieved better outcomes with a better MP joint ROM, grip strength, and DASH score than retrograde pinning 3 months after surgery, but these differences were not observed 6 months after surgery [13]. However, MP joint contracture could occur because the insertion of the wires is close to the extensor tendon and sagittal band. To prevent interference with the extensor mechanism, Han et al. [5] and Lee et al. [6] reported modified retrograde pinning, that Kirschner wires were inserted from the metacarpal head and the proximal end of wires penetrated through the dorsal skin. They indicated good clinical outcomes, although this technique is difficult to lead Kirschner wires to the dorsal side of the metacarpal base. Our study also indicated that a good ROM and DASH score can be achieved using a simple retrograde pinning technique (Table 2). We suggest that the MP joint be flexed during reduction and fixation intraoperatively and during splint fixation post-operatively to prevent contracture of the collateral ligament. Post-operative rehabilitation should be started as soon as possible. Active and passive ROM supervised by a hand therapist will prevent PIP and DIP joint contracture and extensor tendon adhesion. Intraoperatively, Kirschner wires are inserted on both sides of the extensor and passive motion should confirm smooth extensor movement after wire fixation. It is necessary to pay attention in elderly patients because joint contracture tends to occur.

There were some limitations in this study. First, this study was a case series with small numbers and short follow-up periods. More operative cases and follow-ups of more than 1 year are needed to conclude that retrograde pinning has an advantage on antegrade pinning. Second, our report was not a comparative study with other operative techniques. Because of the variety of operative techniques, study designs, and outcome measures, comparison with other studies is limited.
Retrograde pinning could be one of the useful operative techniques for metacarpal shaft fractures if some tips, such as Kirschner wires insertion and post-operative rehabilitation are taken care. This straightforward technique is most successfully performed on those young patients in whom fractures are extraarticular and simple, especially transverse fractures, which are subject to easy reduction and stable fixation.
Although retrograde pinning is a simple and easy operative technique for metacarpal shaft fractures, it may result in MP joint contracture post-operatively. However, we consider that the complication could be prevented by inserting Kirschner wires from the appropriate site to avoid direct damage to the extensor tendon. Moreover, post-operative rehabilitation should be started as soon as possible with wearing a knuckle splint.
References
- 1.Başar H, Başar B, Başçı O, Topkar OM, Erol B, Tetik C. Comparison of treatment of oblique and spiral metacarpal and phalangeal fractures with mini plate plus screw or screw only. Arch Orthop Trauma Surg 2015;135:499-504. [Google Scholar | PubMed]
- 2.Foucher G. “Bouquet” osteosynthesis in metacarpal neck fractures: A series of 66 patients. J Hand Surg Am 1995;20:S86-90. [Google Scholar | PubMed]
- 3.Akinleye SD, Garofolo-Gonzalez G, Culbertson MD, Choueka J. Iatrogenic injuries in percutaneous pinning techniques for fifth metacarpal neck fractures. Hand (N Y) 2019;14:386-92. [Google Scholar | PubMed]
- 4.Lord RE. Intramedullary fixation of metacarpal fractures. J Am Med Assoc 1957;164:1746-9. [Google Scholar | PubMed]
- 5.Han SH, Rhee SY, Lee SC, Han SC, Cha YS. Percutaneous retrograde intramedullary single wire fixation for metacarpal shaft fracture of the little finger. Eur J Orthop Surg Traumatol 2013;23:883-7. [Google Scholar | PubMed]
- 6.Lee SK, Kim KJ, Choy WS. Modified retrograde percutaneous intramedullary multiple Kirschner wire fixation for treatment of unstable displaced metacarpal neck and shaft fractures. Eur J Orthop Surg Traumatol 2013;25:535-43. [Google Scholar | PubMed]
- 7.Hove LM. Fractures of the hand. Distribution and relative incidence. Scand J Plast Reconstr Hand Surg 1993;27:317-9. [Google Scholar | PubMed]
- 8.Tavassoli J, Ruland RT, Hogan CJ, Cannon DL. Three cast techniques for the treatment of extra-articular metacarpal fractures. Comparison of short-term outcomes and final fracture alignments. J Bone Joint Surg Am 2005;87:2196-201. [Google Scholar | PubMed]
- 9.Low CK, Wong HC, Low YP, Wong HP. A cadaver study of the effects of dorsal angulation and shortening of the metacarpal shaft on the extension and flexion force ratios of the index and little fingers. J Hand Surg Br 1995;20:609-13. [Google Scholar | PubMed]
- 10.Yammine K, Harvey A. Antegrade intramedullary nailing for fifth metacarpal neck fractures: A systematic review and meta-analysis. Eur J Orthop Surg Traumatol 2014;24:273-8. [Google Scholar | PubMed]
- 11.Van Bussel EM, Houwert RM, Kootstra TJ, van Heiji M, Van der Velde D, Wittich P, et al. Antegrade intramedullary Kirschner-wire fixation of displaced metacarpal shaft fractures. Eur J Emerg Surg 2019;45:65-71. [Google Scholar | PubMed]
- 12.Moon SH, Kim HS, Jung SN, Kwon H. The efficacy of transverse fixation and early exercise in the treatment of fourth metacarpal bone fractures. Arch Plast Surg 2016;43:189-96. [Google Scholar | PubMed]
- 13.Kim JK, Kim DJ. Antegrade intramedullary pinning versus retrograde intramedullary pinning for displaced fifth metacarpal neck fractures. Clin Orthop Relat Res 2015;473:1747-54. [Google Scholar | PubMed]