Not all dorsal hand cysts are benign as rarely an extra-axial chordoma may lurk within.
Dr. Neha Singh, Room no. 3047, 3rd floor, Department of Pathology, ESIC Medical College and Hospital, Sanath Nagar, Hyderabad, India E-mail: drneha_6@rediffmail.com
Introduction: Conventional chordoma is a malignant osseous neoplasm that usually arises from the axial skeleton. It recapitulates a phenotype of embryonic notochord, usually occurring in the 5th–7th decades of life. Very rarely, chordomas can arise in the extra-axial skeleton, more so in the extra-axial soft tissues. We present one such case of Extra-axial soft tissue chordoma in the dorsum of the hand in an adult patient, with a short review of the literature.
Case Report: A 48-year-old male patient presented with a longstanding swelling on the dorsum of the left hand, persisting for 5 years. Clinico-radiological assessment suggested differential diagnoses of a ganglion cyst or a chondroid lesion. A fine needle aspiration was performed, which was documented as a giant cell-rich soft tissue neoplasm. Subsequent excision biopsy showed histopathological features characterized by numerous multivacuolated, bubbly cytoplasmic physaliferous cells within a myxohyaline matrix, indicative of a neoplastic process. Immunohistochemistry revealed positivity for brachyury, which confirmed the diagnosis of an extra-axial soft tissue chordoma.
Conclusion: Extra-axial soft tissue chordomas are extremely rare malignant osseous neoplasms that can mimic a variety of other lesions, need a strong clinical suspicion, and keen morphological cum immunohistochemical examination for diagnosis. Given their similar imaging characteristics and overlapping histological features, making an accurate diagnosis is crucial, as treatment plans vary significantly.
Keywords: Chordoma, Extra-Axial Soft Tissue Chordoma, Notochord, Brachyury, Physaliferous.
Conventional chordoma is a malignant osseous neoplasm that usually arises from the axial skeleton, having a propensity toward embryonic notochordal differentiation [1]. It usually occurs in the 5th–7th decades of life. Axially, it can involve the bones of the spine, the base of skull, and sacrococcygeal region Very rarely chordomas can arise in the extra-axial skeleton, more so in the extraskeletal soft tissues. As per the literature, only 28 cases of Extra-axial Chordomas are reported as of 2018 [2]. When presenting in an extra-axial site, assessment of brachyury expression by immunohistochemical (IHC) examination proves to be of immense value in confirmation. Additional molecular evaluations are necessary for further exploring into the pathogenesis of extra-axial Chordomas (EAC). We present one such case of Extra-axial soft tissue chordoma in the dorsum of the hand in an adult patient, with a short review of the literature.
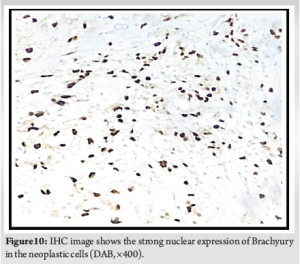
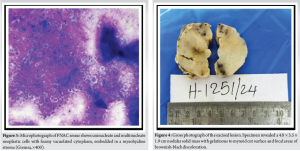
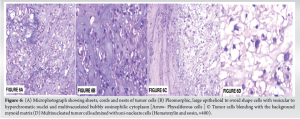
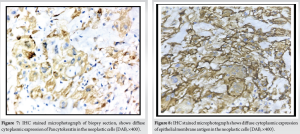
A 48-year-old male patient presented to the orthopedic clinic with swelling in the dorsum of the left hand since 5 years. The swelling was insidious in onset and gradually progressive. There was no history of trauma, constitutional symptoms, recent weight loss, or loss of appetite. No local rise of temperature or pain was noted in association with the lesion. On physical examination, a lobulated 5 × 4 cm sized swelling with well-defined margins was noted in the dorsum of the left hand (Fig. 1). The lesion spanned from the 3rd to 5th metacarpal region and had a smooth surface with soft to cystic consistency. The skin over the lesion was pinchable. The swelling was mobile in the horizontal direction, but not in the vertical direction. The swelling became prominent with the extension of fingers. On radiological examination of the left hand, there were soft tissue shadows seen in the dorsum, with a scalloping effect and cortical erosion noted in the distal end of the 3rd metacarpal bone (Fig. 2). Background mature skeleton was unremarkable. With clinical differentials of Ganglion cyst versus chondroid lesion, the patient was referred for a fine needle aspiration cytology (FNAC) procedure. FNAC showed abundant cellular material comprising of giant cells admixed with myxoid stromal elements in addition to the presence of multivacuolated cells, hence a report of “Giant cell rich soft tissue neoplasm” was rendered (Fig. 3). Since the margins of the tumor were well-demarcated, and FNAC exhibited a benign morphology, excision biopsy was performed and the specimen was sent to histopathological examination. Specimen post-formalin fixation revealed a 4.8 × 3.5 × 1.9 cm nodular solid mass with gelatinous to the myxoid surface (Fig. 4). Externally, the lesion was bosselated with lobulations noted on the cut surface. Solid areas were yellow to grey-tan in color with tiny cystic spaces embedded in it. Focal brown-black hemorrhagic areas possibly from the previous FNAC site were noted admixed with mucinous areas on gross evaluation. On microscopy, the sections studied showed a well-encapsulated neoplasm composed of lobules of tumor tissue separated by fibrous strands in a myxohyaline stroma (Fig. 5). The tumor cells were arranged in sheets, cords, and nests, were pleomorphic showing large epithelioid to ovoid shapes with vesicular to hyperchromatic nuclei and multivacuolated bubbly eosinophilic cytoplasm, resembling like physaliferous cells notably seen with chordoma (Fig. 6a-d). At places, the cell borders were indistinct and seem to be blending with the background myxohyaline matrix. No evidence of bony trabeculae or osteoid was noted in the lesion. There was intratumoral heterogeneity observed with solid, myxoid, microcystic, and hemorrhagic areas in varying proportions. With these findings on H&E staining, a primary provisional diagnosis of EAC was rendered on morphology with a note to perform IHC analysis for brachyury to consider EAC. In addition, a panel of IHC markers performed to rule out differential diagnoses, namely, soft tissue Myoepithelioma and other chondroid soft tissue lesions as well. The results of the IHC profile (Fig. 7 and 8) revealed that the neoplastic cells were positive for Pan-Cytokeratin (PCK) and Epithelial Membrane Antigen (EMA), S100, Ki-67 while negative for p63 and Glial Fibrillary Acidic Protein (GFAP) (Fig. 9a-d). There was a strong nuclear positivity for brachyury highlighting the neoplastic physaliferous cells (Fig. 10). Thus, a final diagnosis of Extra-axial soft tissue chordoma on the dorsum of the left hand was rendered. Post-operative as well as follow-up periods were uneventful as of now.


Conventional chordoma by definition is a malignant osseous neoplasm that usually arises from the axial skeleton and that recapitulates a phenotype of embryonic notochord [1]. The incidence of chordoma is 0.08 cases per 1,00,000 person years and has a male predilection [1]. Although all age groups are affected, predominantly it occurs in the 5th–7th decades of life. Axially it can involve bones from the base of the skull to the coccyx with preferential order of occurrence as mobile spine (32.8%), skull-based (32%), and in the sacrococcygeal region (29.2%). As per the recent World Health Organization [WHO] publication [1], only a very small number of extra-axial cum extra-skeletal chordomas are reported. Radiologically, chordoma is usually visualized as a lytic destructive lesion that grows slowly and expands the bone forming a large mass. In the present study, there was no evidence of bony expansion noted; rather, the lesion was predominantly noted in the soft tissue plane. On Magnetic Resonance Imaging (MRI), chordoma appears as a lobulated and septated heterogenous mass, showing enhancement after gadolinium administration [1]. Histopathologically, conventional chordomas are composed of large epithelioid cells with clear to light vacuolated cytoplasm, which are separated into lobules by fibrous septa. The bubbly cytoplasm of the neoplastic cells is the reason why they are referred to as physaliferous cells [1]. Architecturally, these cells are arranged as cords and nests embedded in an abundant extracellular matrix. The neoplasm is known for its morphological heterogeneity within the tumor, such as areas with high nuclear grade alternating with areas of minimal nuclear atypia. Variants of Chordoma are also noted, such as chondroid chordoma, de-differentiated chordoma, and poorly differentiated chordoma. Chondroid chordomas have large areas of matrix mimicking hyaline cartilaginous tumors, while de-differentiated chordomas have a biphasic appearance characterized by a conventional chordoma along with a high-grade sarcoma in the same lesion. Poorly differentiated chordomas usually arise in the axial skeleton and are characterized by loss of SMARCB1 expression [1]. In a study by Righi et al., who documented 6 cases of EACs, the authors mention the rarity of the tumor as only 28 cases had been reported in the literature as of 2018 [2]. In addition, the authors comment that EAC cases are underdiagnosed and often misdiagnosed as Extraskel et al. chondrosarcoma or myoepithelioma [2]. A study by Suzuki et al. reports a case of EAC of the wrist in an 87-year-old man which was having similar appearance as the present study, with positivity for Cytokeratin 19 and Brachyury [3]. The author says that EAC is the same entity called Parachordoma (Chordoma periphericum) as originally proposed by Laskowski and Dabska [3]. In various studies, EACs were also reported in locations, such as proximal tibia, wrist, hand, and gingiva [4-9]. A study by Huang et al. describes how a Renal cell carcinoma (RCC) in a 74-year-old male patient, suspected to be metastasized in the proximal tibia, was actually found to be masquerading an EAC [4]. Further, IHC with Brachyury confirmed that it was EAC and not metastatic RCC. There are studies that underpin the use of Brachyury by IHC to help distinguish EAC from myoepithelioma, myxoid soft tissue tumors, and mixed tumors [10, 11]. Molecular analyses throw insight upon the recurrent loss of Chromosome 22 and SMARCB1 deletion in EACs. While conventional EACs show a simple genome with loss of Chromosome 22 or heterozygous deletion of SMARCB1, poorly differentiated types show multiple chromosome losses and homozygous deletion of SMARCB1 [12, 13].
EACs are very rare and attempting to think of EACs in a non-axial site as a differential is predominantly based on histomorphology by appreciating the physaliferous cells, while the use of brachyury helps in confirmation. Extensive molecular studies are required in the future to know the genomic profile of these extremely rare EACs.
Long-standing large lesions with soft to cystic consistency in the dorsum of the hand may not always be ganglion cysts. Even though these lesions are well-demarcated and well-circumscribed, the possibility of a malignant extra axial chordoma can be considered as the least possible differential along with other chondroid neoplasms. Although chordoma is known for its painful presentation on clinical examination, this patient had no pain surprisingly.
References
- 1.Tirabosco R, O’Donnell PG, Yamaguchi T. Notochordal tumors/Conventional chordoma. In: WHO Classification of Tumors Editorial Board. Soft Tissue and Bone Tumors. WHO Classification of Tumors Series. 5th ed., Vol. 3. Lyon, France: International Agency for Research on Cancer; 2020. Available from https://tumorclassification.iarc.who.int/chapters/33 [Last accessed on 2024 Oct 10]. [Google Scholar]
- 2.Righi A, Sbaraglia M, Gambarotti M, Cocchi S, Drago G, Casadei R, et al. Extra-axial chordoma: A clinicopathologic analysis of six cases. Virchows Arch 2018;472:1015-20. [Google Scholar]
- 3.Suzuki H, Yamashiro K, Takeda H, Nojima T, Usui M. Extra-axial soft tissue chordoma of wrist. Pathol Res Pract 2011;207:327-31. [Google Scholar]
- 4.Huang J, Bhojwani N, Oakley FD, Jordanov MI. Proximal tibial extra-axial chordoma masquerading as renal cell carcinoma metastasis. Skeletal Radiol 2017;46:1567-73. [Google Scholar]
- 5.Neumann J, Gersing AS, Barth TF, Boxberg M, Woertler K. Intra-articular extra-axial chordoma of the wrist: A case report with review of the current literature. Skeletal Radiol 2019;48:2015-20. [Google Scholar]
- 6.Bitzer A, McCarthy EF, Morris CD. Extra-axial chordoma of the hand. J Hand Surg Am 2017;42:933.e1-5. [Google Scholar]
- 7.Ueda T, Kubota K, Shiroma N, Maeda S, Furuie H, Taruya T, et al. Extra-axial chordoma of the gingiva. Auris Nasus Larynx 2020;47:299-304. [Google Scholar]
- 8.DiFrancesco LM, Davanzo Castillo CA, Temple WJ. Extra-axial chordoma. Arch Pathol Lab Med 2006;130:1871-4. [Google Scholar]
- 9.Tsukamoto S, Vanel D, Righi A, Donati DM, Errani C. Parosteal extra-axial chordoma of the second metacarpal bone: A case report with literature review. Skeletal Radiol 2018;47:579-85. [Google Scholar]
- 10.Tirabosco R, Mangham DC, Rosenberg AE, Vujovic S, Bousdras K, Pizzolitto S, et al. Brachyury expression in extra-axial skeletal and soft tissue chordomas: A marker that distinguishes chordoma from mixed tumor/myoepithelioma/parachordoma in soft tissue. Am J Surg Pathol 2008;32:572-80. [Google Scholar]
- 11.Nibu Y, José-Edwards DS, Di Gregorio A. From notochord formation to hereditary chordoma: The many roles of Brachyury. Biomed Res Int 2013;2013:826435. [Google Scholar]
- 12.Klubíčková N, Michal M, Kinkor Z, Soukup J, Ryška A, Brtková J, et al. Poorly differentiated extra-axial extraskeletal chordoma diagnosed by methylation profiling: Case report and analysis of brachyury expression in SWI/SNF-deficient tumors. Virchows Arch 2024;484:621-7. [Google Scholar]
- 13.Wen X, Cimera R, Aryeequaye R, Abhinta M, Athanasian E, Healey J, et al. Recurrent loss of chromosome 22 and SMARCB1 deletion in extra-axial chordoma: A clinicopathological and molecular analysis. Genes Chromosomes Cancer 2021;60:796-807. [Google Scholar]