This case highlights the critical need for specialized pediatric orthopedic care, advanced intraoperative imaging in resource limited settings, and continuous parent education to improve outcomes and quality of life for children with bilateral radial club hand.
Dr. Oluwatosin Gabriel Afolabi, Department of Surgery, Federal Teaching Hospital Ido-Ekiti, Ekiti State, Nigeria. E-mail: otosinafolabi@gmail.com
Introduction: Radial aplasia is a rare congenital anomaly of the upper limbs, more common in females, affecting between one in 30,000 and one in 100,000 live births, and primarily impacting structures on the radial side of the forearm. While there have been numerous articles on bilateral radial aplasia and its management, this case is particularly significant as it represents the index case for our hospital. It is the first report to highlight how limited resources can lead to unfavorable outcomes in the management of this condition. In addition, it aims to stimulate the interest of the global orthopedics community to develop interventions or modify current treatment options that can be successfully implemented in low-resource settings to improve outcomes, especially the functionality of the limbs. By documenting this case, we aim to shed light on the challenges faced in resource-limited settings and advocate for increased investment in training pediatric orthopedic specialist to enhance the quality of life for affected children.
Case Report: A 1-year-old boy of African descent presented with bilateral radial club hand. The patient exhibited characteristics of classical radial club hand, with complete absence of the radius and thumbs bilaterally, resulting in the nonexistence of the radio-carpal and radio-ulna joints. The forearm and ulna were shorter, with the ulna’s diaphysis curved toward the radius. No hematological abnormalities were noted, and the case was non-syndromic with no identifiable risk factors. The patient underwent serial manipulation and casting for 17 months to achieve sufficient soft tissue stretching and passive correction of the deformity before the centralization procedure.
Conclusion: This case underscores the urgent need for improved access to specialized pediatric orthopedic care, advanced intraoperative imaging tools, and comprehensive, continuous parent education on realistic treatment expectations for patients with bilateral radial club hand. Addressing these limitations can enhance long-term outcomes and quality of life for children with this condition. This case report is of particular interest to both current and intending pediatric orthopedic specialists and highlights the broader clinical impact of resource limitations on treatment outcomes. In addition, it significantly advances our knowledge of the challenges faced in managing severe congenital anomalies in resource-limited settings.
Keywords: Bilateral radial aplasia, radial club hand, congenital anomaly.
Radial aplasia or radial club hand is a congenital absence of the radius, a rare congenital anomaly of the upper limbs and this account for about 10% of the all congenital abnormalities [1]. It is more commoner in females with affecting between 1:30,000 and 1:100,000 live births [2, 3]. Although rare, it is the most common anomaly of longitudinal formation in the embryological classification of congenital deformities of the upper limbs by the International Federation of Societies for Surgery of the Hand [4]. Being a disorder of the preaxial border of the upper limb, it can affect any structures (bones, muscles, tendons, ligaments, and neurovascular bundles) on the radial side of the forearm. It may occur in isolation, but frequently associated with other syndromes fanconi anemia, TAR, Lewis, Nager, Roberts, VACTERL, Holt-Oram, RAPADILINO, OKIHIRO among others [3, 5]. There are different classifications of radial club hand but the most common is the system described by Bayne and Klug [6]. Type I is characterized by a short distal radius (the distal growth plate is present). Type II involves a hypoplastic radius where it is smaller and thinner than the ulna, and no growth plate is present. Type III shows a partial absence of the radius (a small proximal segment of the radius remains, ulna is hypertrophied and angled radially). Type IV involves a total absence of the radius. This is the most common and severest form [6]. Early prenatal exposure to antiepileptic drugs (valproic acid and phenobarbital), thalidomide, and aminopterin has been associated with radial aplasia [7]. Treatment options range conservative to surgical intervention depending on the severity of the condition from. Although this should begin from the time of birth irrespective of the type of deformity [8]. Management of congenital bilateral radial aplasia comes with numerous challenges, especially in a low-resource setting with limited facilities and technical know-how. This is a case of bilateral radial club hand in a boy, managed in a resource-limited setting, resulting in unfavorable outcomes. This highlights the urgent need for improved pediatric orthopedic care and innovative interventions for low-resource environments. This retrospective case report is based on a comprehensive review of the patient’s medical records from December 1st, 2022 to May 30th, 2024. Data extraction was performed using a standardized data collection form, including information on prenatal history, physical examination findings, imaging studies, treatment details, and follow-up information. The extracted data were analyzed to identify key challenges, treatment outcomes, and the impact of limited resources on the patient’s development and quality of life.
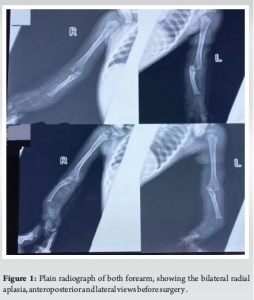
A 10-day-old male neonate was brought to the orthopedics outpatient department by his mother due to an abnormality in both hands noticed at birth. The baby’s 37-year-old mother, who is married in a non-consanguineous setting, registered at 16 weeks gestational age at a primary health center where she received antenatal care. There was no history of maternal illness, ingestion of alcohol or smoking, or exposure to radiation before or during the pregnancy during pregnancy. Throughout the pregnancy, the mother received routine hematinics (ferrous sulfate and folate), tetanus prophylaxis, and intermittent preventive treatment for malaria in normal doses. In addition, she underwent five obstetric ultrasounds at 24, 28, 32, 36, and 38 weeks, respectively, at a primary health-care center, during which the anomaly was not discovered. No history of similar anomalies in paternal or maternal families. Delivery was through caesarean sections due to a breech presentation and a previous history of early fetal demise due to prolonged labor. No similar findings were noticed in the previous child after birth. The child cried immediately after birth with an APGAR score was 51, 95. Baby passed meconium and urine within the first 36 h of life. On physical examination, the patient was a normal-looking neonate, pink, and active, with obvious bilateral anomaly of both needles and no rashes. His birth weight was 2.9 kg. There was bilateral shortening of the forearms with varus deviation of the hands and hyper-mobility of the wrist joints. The thumbs were absent bilaterally. There was no clinical evidence of congenital heart disease and kidneys were not ballotable. Other systems were examined and found normal. Radiography of the forearm showed a bilateral absence of the radii. Ulna bones were bowed and their distal ends deviated to the radial side (Fig. 1). The metacarpals and phalanges were normal.
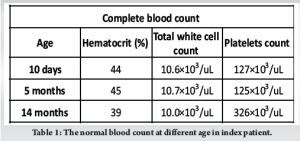
A complete blood count was carried out 3 times throughout the clinic visit and found normal (Table 1). Bone one marrow biopsy done on the 90th day of life of showed normal study.
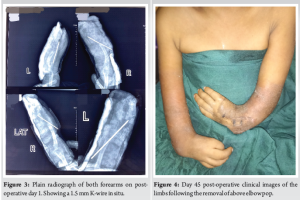
The child underwent a 60-week conservative treatment plan, which included stretching, serial manipulations, and above-elbow casting with Plaster of Paris every 2 weeks to prepare the soft tissues for surgical correction. The operative procedure took place when the child was 18 months old and involved a 4 cm incision on the back of the hand along the ulnar border under tourniquet. Significant ulna deviation was performed to correct the anomaly in the forearm and wrist. A 1.5 mm size Kirchner wire (K-wire) was used to centralize the ulna. This procedure was then repeated on the other side without intraoperative imaging. Both forearms were immobilized with above-elbow casts. A post-operative radiograph was taken the day after the surgery (Fig. 2). There were some complications such as the K-wire going through the palm the create a puncture wound, spontaneous removal of the pins in the weeks following the surgery, leading to the discontinuation of all interventions by the parent at the time of writing this report Fig. 3.
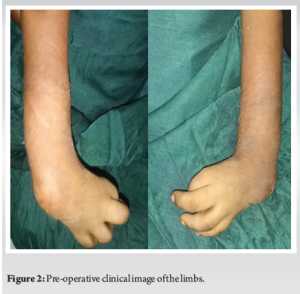
In this case, the patient exhibits characteristics of classical radial club hand. The radius and thumbs are completely absent bilaterally, resulting in the non-existence of the radio-carpal and radio-ulna joints, which affects flexion-pronation movement. The forearm and ulna are shorter, with the ulna’s diaphysis curved toward the radius. No hematological abnormalities were noted. The case is non-syndromic with no identifiable risk factors, fitting into the class IV Bayne and Klug, the most common and severe form. Treatment options range from conservative methods, like orthoses and stretching exercises from birth, to surgical correction, depending on severity. For Bayne type I and II, conservative care may suffice, while surgery is typically recommended for Bayne type III and IV [1]. Main surgical procedures include centralization and radialization of the carpus. Centralization centers the carpus on the ulna, while radialization places the radial portion of the carpus on the ulna to increase leverage and prevent recurrence. Gradual correction using the Ilizarov method is also described for Bayne Type III or IV [9]. Our patient underwent serial manipulation and casting for 17 months to achieve sufficient soft tissue stretching and passive correction of the deformity as a prerequisite for successful surgery before the centralization procedure and immobilization from the axilla to the palm with plaster of Paris at 18 months of age. Most successful cases of the centralization procedure have been reported with the use of intraoperative fluoroscopic imaging to confirm the location and alignment of the pins [1,9,10]. In addition, some authors have suggested the use of two K-wire (one from the carpus to the metacarpal bone and another inversely inserted) for increased stability [9,10]. However, in this case, intraoperative imaging was not available, and the procedure was performed without intraoperative imaging using a single K-wire. Post-operative plain X-rays of both upper limbs were taken on the 1st day, unlike other cases where intraoperative imaging was used [1,10]. The rest of the post-operative period was quite eventful, with several complications. On the 5th day after surgery, the K-wire in the right hand had completely dislodged spontaneously, while the wire in the left hand had migrated through the entire palm, creating a 0.5 cm puncture wound in the web space between the fourth and fifth digits by the 14th day post-operation. These complications were likely due to poor bone penetration on the right and excessive penetration on the left, resulting from the lack of imaging to confirm the position of the K-wires intraoperatively. This necessitated the manual removal of the K-wire on the 15th post-operative day, compared to the standard practice of removal between 6 and 12 weeks [1,9,10]. The patient then continued with serial manipulation, casting, and regular wound dressing, with a plan to repeat of the K-wire fixation in the future. Unfortunately, 8 weeks after surgery, the parents presented to the clinic for a follow-up and requested the removal of the cast, expressing their desire to discontinue any further conservative or surgical interventions. The reasons highlighted by the parents included the failure of the initial procedure, lack of improvement in hand function, significant cost of care with no positive outcomes, and inadequate information and counseling about the condition. From a health-care perspective, the lack of imaging facilities at the managing center and lack of pediatric orthopedic expertise significantly contributed to this unfavorable outcome. At the time of this report, the child is unable to use both upper limbs for routine activities expected at their developmental milestones. Consequently, their quality of life is significantly affected, and they may be dependent on others for the rest of their life (Fig. 4).
This case report advocate for the urgent need for improved access to specialized pediatric orthopedic care, advanced intraoperative imaging tools, and comprehensive, continuous parent education on realistic treatment expectations for patients with bilateral radial club hand in ensuring successful outcomes for centralization procedures in low-resource settings. Addressing these limitations can enhance long-term outcomes and quality of life for children with this condition.
This case report of bilateral radial club hand in a resource-limited setting highlights the critical impact of inadequate medical resources and expertise on treatment outcomes. It is valuable for clinicians and policymakers alike, as it stresses the importance of resource allocation and innovative solutions to enhance the quality of life and functional outcomes for children with rare congenital anomalies. It emphasizes the need for the global orthopedics community to develop and implement effective interventions tailored for low-resource environments and crates an awareness of the challenges faced in such settings.
References
- 1.Chung MS. Congenital differences of the upper extremity: Classification and treatment principles. Clin Orthop Surg 2011;3:172-7. [Google Scholar]
- 2.Vergult S, Hoogeboom AJ, Bijlsma EK, Sante T, Klopocki E, De Wilde B, et al. Complex genetics of radial ray deficiencies: Screening of a cohort of 54 patients. Genet Med 2013;15:195-202. [Google Scholar]
- 3.D’Arcangelo M, Gupta A, Schecker LR. Radial club hand. In: Gupta A, Ray SP, Schecker LR, editors. The Growing Hand. Diagnosis and Management of the Upper Extremity in Children. London: Mosby; 2000. p. 147-68. [Google Scholar]
- 4.De Smet L, IFSSH. International federation for societies for surgery of the hand JSSH. Japanese Society for Surgery of the Hand. Classification for congenital anomalies of the hand: The IFSSH classification and the JSSH modification. Genet Couns 2002;13:331-8. [Google Scholar]
- 5.Goldfarb CA, Wall L, Manske PR. Radial longitudinal deficiency: The incidence of associated medical and musculoskeletal conditions. J Hand Surg Am 2006;31:1176-82. [Google Scholar]
- 6.Bayne LG, Klug MS. Long-term review of the surgical treatment of radial deficiencies. J Hand Surg Am 1987;12:169-79. [Google Scholar]
- 7.Rodríguez-Pinilla E, Arroyo I, Fondevilla J, García MJ, Martínez-Frías ML. Prenatal exposure to valproic acid during pregnancy and limb deficiencies: A case-control study. Am J Med Genet 2000;90:376-81. [Google Scholar]
- 8.Manske PR, Goldfarb CA. Congenital failure of formation of the upper limb. Hand Clin 2009;25:157-70. [Google Scholar]
- 9.Matsuno T, Ishida O, Sunagawa T, Suzuki O, Ikuta Y, Ochi M. Radius lengthening for the treatment of Bayne and Klug type II and type III radial longitudinal deficiency. J Hand Surg Am 2006;31:822-9. [Google Scholar]
- 10.Konadu-Yeboah D, Konadu P, Yifieyeh Abiboye C, Ampem-Darkwa, Schumacher Z. Bilateral radial club hands at the komfo anokye teaching hospital, Kumasi, Ghana: A case report. J Prev Med Care 2019;3:10-6. [Google Scholar]