Prophylactic reconstruction or replacement in cases of impending pathological fractures provides good prognosis while minimizing complications.
Dr. B Mohan Choudhary, Department of Orthopaedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: krishna.nallay@gmail.com
Introduction: Pathological fractures are becoming a very common entity in routine clinical practice due to the widespread prevalence of a wide variety of primary tumors in metropolitan and rural areas. Pathological fractures are often underdiagnosed by surgeons in day-to-day practice. Managing such missed fractures in patients is a nuisance. In this case report, we look into one such patient who came to us with successive serial fractures of multiple long bones.
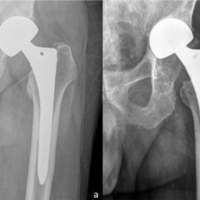
Case Report: A 49-year-old lady presented to us with complaints of right hip with no history of trauma. Plain radiographs were done which revealed a right neck of femur fracture. She underwent right hip bipolar hemiarthroplasty. Forty-five days later she had another trivial injury to her left hip and was diagnosed through radiographs as left neck of femur fracture, for which she underwent left hip bipolar hemiarthroplasty.
Conclusion: A thorough evaluation of bony metastasis is required in the management of pathological fractures or impending fracturesto prevent missing such fractures and early surgical intervention provides good outcome in most cases.
Keywords: Pathological fractures, bipolar hemiarthroplasty, multiple long bones.
Pathological fractures of long bones are one of the common complications caused by a variety of primary tumors. Musculoskeletal system is the third most common site of metastasis after lung and liver respectively. Advanced breast carcinoma, prostate carcinoma, renal carcinoma, and multiple myeloma have shown to have increased incidence of skeletal metastasis. Of those, the tumor that metastasizes to the hip with the greatest frequency is carcinoma of the breast [1-4]. Pathologic lesions in this important weight-bearing zone weaken its ability to sustain load causing pain and impending pathologic fracture [1]. Pathologic fractures rarely heal on their own, since a tumor at the fracture site prevents bone healing. The majority of fractures are successfully managed with surgical intervention. A wide variety of surgical interventions are available to manage pathological fractures. The aim of this case report is to the study the role and outcome of bipolar hemiarthroplasty in the neck of femur fractures secondary to skeletal metastasis.
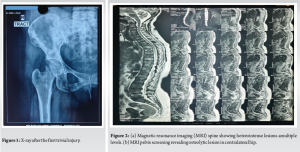
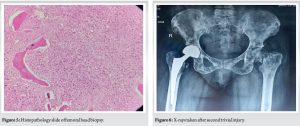
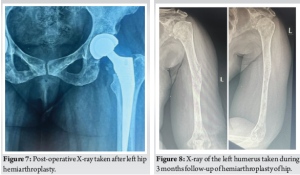
This case report involves a 49-year-old lady who is a biopsy-proven case of triple-negative mammary invasive carcinoma of the left breast and underwent a left mastectomy in 2018. Following which she was on eight cycles of chemotherapy, followed by radiotherapy and hormonal therapy. Two years following mastectomy 1 day while she was on her way for chemotherapy she had a trivial injury to her right hip. She was not able to ambulate post-injury. She came to us with complaints of right hip pain. On examination, she had tenderness over the Scarpa’s triangle and painful hip movements. Endocrinology workup was done which showed reduced serum calcium and elevated serum phosphorous and alkaline phosphatase levels. Radiographs revealed an undisplaced subcapital fracture of the right femoral neck (Fig. 1). Magnetic resonance imaging (MRI) of the spine showed heterointense lesions involving the entire spine in T1/T2 and STIR images (Fig. 2a). MRI also revealed osteolytic lesions in the contralateral neck of femur (Fig. 2b). Positron Emission Tomography scan was suggestive of extensive skeletal metastasis involving the entire axial skeletal system, bilateral humerus, ribs, bilateral scapula, and bilateral proximal femur (Fig. 3a and b). After a thorough review of the literature and assessing all possible options of intervention, the patient underwent right hip bipolar uncemented hemiarthroplasty following an anesthetic workup (Fig. 4). The femoral head was sent for histopathological examination. Intraoperative biopsy revealed fragments of bony trabeculae enclosing suppressed marrow elements and fat infiltrated by a tumor composed of singled-out cells which are eosinophilic in nature with peripherally pushed hyperchromatic nucleus showing atypia and mitosis (Fig. 5). Thus confirming the metastatic spread to the femoral head. Postoperatively, patient was advised strict bed rest and was not allowed to weight bear post-procedure. The patient was regularly followed up 2 weeks, 4 weeks, and 6 weeks post-procedure. Forty-five days post-procedure, subsequently patient had another episode of trivial injury to her left hip. She was worked up again through the same protocols and she diagnosed with a transcervical undisplaced left neck of femur fracture (Fig. 6). Patient again underwent bipolar uncemented hemiarthroplasty in the contralateral hip (Fig. 7). The patient was followed up in regular intervals. There was no periprosthetic joint infection, loosening of femoral stem, periprosthetic fractures or dislocation in the post-operative period. At 3 months, follow-up functional and radiological outcomes were assessed and were satisfactory. However, patient had another trivial injury to her left humerus which revealed undisplaced fracture of humeral shaft (Fig. 8). We did not want to operate her due to increased risk of perioperative cardiac and neurological worsening of patient. Henceforth, she was managed conservatively with custom-made thermoplastic splint. She was again followed up serially and the fracture healed well without any functional compromise (Fig. 9).


The proximal femur is a common location for bone metastases and pathologic or impending fractures are frequently observed due to the biomechanical characteristics of this site[5,6]. The most common causes for pathological femur fractures are osteoporosis, osteomalacia, and malignancy [7]. Malignancy with extensive skeletal metastasis warrants a need for prophylactic surgical intervention which is evaluated through Mirels criteria. In the setting of a pathological or impending fracture, current treatment options include endoprosthetic replacement, or intramedullary or extramedullary fracture fixation [3]. Osteosynthesis is preferred in patients with a small focal lesion in the trochanteric or peritrochanteric fracture without the involvement of the acetabulum and femoral head and neck. In the case of proximal femoral fractures, osteosynthesis may provide unyielding results. Patients are also at a higher risk of implant failure and revision surgery rate is higher in these patients. Therefore, a joint replacement surgery is preferred in such cases. There’s a debate whether hemiarthroplasty or total hip arthroplasty is preferred in such a scenario. Total hip arthroplasty is preferred in most young patients with metastatic fractures due to lesser complication and revision rates [8]. However, in this scenario, which chose to go ahead with an uncemented bipolar hemiarthroplasty considering her socioeconomic demands and her life expectancy. Among all subtypes of breast carcinoma triple-negative breast carcinoma has the worst prognosis [9,10]. Most patients with triple-negative breast carcinoma with extensive metastasis have a life expectancy of <5 years. An uncemented bipolar prosthesis has an average expectancy of 10 years. A hemiarthroplasty yields acceptable results in patients with extensive skeletal metastasis with a low rate of revision surgeries [2]. The common issues observed following a hemiarthroplasty are aseptic loosening and acetabular wear. Patients often complain of residual thigh and hip pain. To overcome this a total hip replacement is performed. A cemented total hip replacement is performed in such instances due to the need for post-operative radiotherapy. Dislocation is a common reported complications following endoprosthetic replacement of the proximal femur in the setting of a pathological fractures.[9] Custom made prosthesis is preferred in extensive femoral involvement, failed modular replacement or in patients with greater life expectancy. The common complications observed in such implants are instability and rate of dislocation postoperatively. The other issue is the cost of the implants and availability.
Proximal femoral metastatic involvement is a marker of advanced disease with reduced prognosis and is related to tumor and warrants a prophylactic replacement [5]. Replacement for this patient population is a palliative procedure with the primary goals to provide pain relief and enable ambulation, while limiting complications.
Bipolar modular uncemented hemiarthroplasty produces excellent results in patients with malignancy and extensive skeletal metastasis provided early surgical intervention is made.
References
- 1.Khattak MJ, Ashraf U, Nawaz Z, Noordin S, Umer M. Surgical management of metastatic lesions of proximal femur and the hip. Ann Med Surg (Lond) 2018;36:90-5. [Google Scholar | PubMed]
- 2.Houdek MT, Wyles CC, Labott JR, Rose PS, Taunton MJ, Sim FH. Durability of hemiarthroplasty for pathologic proximal femur fractures. J Arthroplasty 2017;32:3607-10. [Google Scholar | PubMed]
- 3.Angelini A, Trovarelli G, Berizzi A, Pala E, Breda A, Maraldi M, et al. Treatment of pathologic fractures of the proximal femur. Injury 2018;49(Suppl 3):S77-83. [Google Scholar | PubMed]
- 4.Murray JA, Parrish FF. Surgical management of secondary neoplastic fractures about the hip. Orthop Clin North Am 1974;5:887-901. [Google Scholar | PubMed]
- 5.Putnam DS, Philipp TC, Lam PW, Gundle KR. Treatment modalities for pathologic fractures of the proximal femur pertrochanteric region: A systematic review and meta-analysis of reoperation rates. J Arthroplasty 2018;33:3354-61. [Google Scholar | PubMed]
- 6.Jacofsky DJ, Haidukewych GJ. Management of pathologic fractures of the proximal femur: State of the art. J Orthop Trauma 2004;18:459-69. [Google Scholar | PubMed]
- 7.Sakale H, Yadav SK, Kar BK, Kowshik S, Agrawal AC, Ranjan R. Pathological fractures of bilateral neck of femur in geriatric population: Our experience and review of literature. J Orthop Case Rep 2022;12:1-4. [Google Scholar | PubMed]
- 8.Tepper SC, Lee L, Kasson LB, Herbst LR, Vijayakumar G, Colman MW, et al. Hip arthroplasty outcomes in patients with metastatic bone disease. Orthop Rev (Pavia) 2024;16:94568. [Google Scholar | PubMed]
- 9.Menendez LR, Ahlmann ER, Kermani C, Gotha H. Endoprosthetic reconstruction for neoplasms of the proximal femur. Clin Orthop Relat Res 2006;450:46-51. [Google Scholar | PubMed]
- 10.Wang C, Chen Z, Zhou Y, Huang W, Zhu H, Mao F, et al. T1a triple negative breast cancer has the worst prognosis among all the small tumor (<1 cm) of TNBC and HER2-rich subtypes. Gland Surg 2021;10:943-52. [Google Scholar | PubMed]