Distal humerus fractures are challenging to treat due to their complexity, but orthogonal dual plating provides stable fixation, allowing for early mobilization and favorable functional outcomes. Studies show high success rates with minimal complications, making it a reliable option even for complex fractures.
Dr. Setu Kaneria, Department of Orthopaedic Surgery, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pimpri-Chinchwad, Pune - 411018, Maharashtra, India. E-mail: setu.kaneria141@gmail.com
Introduction: The study aimed to evaluate the functional outcomes by treating intra-articular distal humerus fractures using orthogonal plating, with or without olecranon osteotomy. The evaluation criteria included Mayo Elbow Performance score (MEPS), range of motion, and complications arising from surgical management.
Materials and Methods: This is a retrospective study of 34 intra-articular distal humerus fractures (AO classification type C) admitted at our institution for 2 years, 6 months from May 2021 to September 2023, all treated with orthogonal plating. Follow-up was for 1 year period at an interval of 3 months.
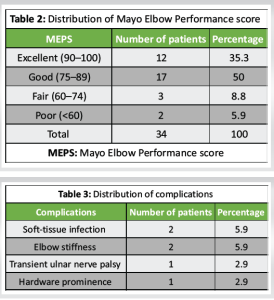
Results: The mean age of the study group was 42.2 ± 14.83 years, ranging from 22 to 76. The mean MEPS was 82.06 ± 10.66. According to MEPS, the outcome was excellent to good in 29 (85.3%) cases, fair in 3 (8.8%), and poor in 2 (5.9%) individuals. Complications such as superficial infection, soft-tissue infection, transient ulnar nerve neuropathy, and elbow stiffness were observed in six out of 34 patients (17.65%), and the mean flexion range was 117.2.
Conclusion: This study demonstrates that orthogonal plating for intra-articular distal humerus fractures provides satisfactory functional outcomes. The surgical approach was effective in restoring elbow function with acceptable complication rates. The decision to perform olecranon osteotomy was based on intraoperative visualization needs, and outcomes were comparable between patients with and without osteotomy. No significant differences were observed in functional recovery between right- and left-sided fractures or between male and female patients. Therefore, we conclude that orthogonal plating represents a reliable treatment option regardless of age, gender, or the specific type of intra-articular distal humerus fracture.
Keywords: Orthogonal plate fixation, olecranon osteotomy, mayo elbow performance score, intra-articular fracture, distal humerus fractures.
Intra-articular distal humerus fractures are one of the most challenging injuries to manage due to the complex anatomy of the elbow, comminution, and poor bone quality in elderly individuals, which makes orthogonal plating difficult. These fractures account for 0.5% of all fractures and exhibit a bimodal distribution [1]. In young individuals, high-velocity trauma, such as road traffic accidents and side-swipe injuries are common causes, whereas osteoporotic bone and simple falls are predominant in elderly individuals [2]. Sound articular reduction is crucial for restoring a fully functional range of motion (ROM) at the elbow joint and preventing painful arthritis. Open reduction and internal fixation is the preferred method for accurate intra-articular correction. Dual plating, whether orthogonal or parallel configurations, provides extremely rigid fixation. There is ongoing debate regarding the optimal plate position, with previous studies not demonstrating clinical superiority of orthogonal over parallel plating in complex intra-articular distal humerus fractures [3]. The study aimed to evaluate the functional outcomes of intra-articular distal humerus fracture fixation using orthogonal plating, assessing post-operative recovery, complications, and the effectiveness of surgical intervention in restoring elbow function using the Mayo Elbow Performance score (MEPS) to measure a ROM and assess complications associated with surgical management.
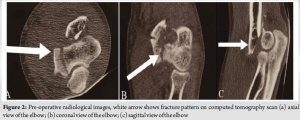
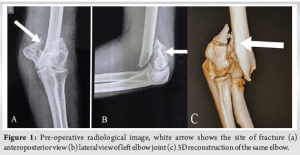
This retrospective study included 34 patients with intra-articular distal humerus fractures (AO classification type C) treated at our institution over 2 years and 6 months, from May 2021 to September 2023, and data was retrieved from institution medical records. All fractures were managed using orthogonal plating, and follow-up continued for 1 year at 3-month intervals. Inclusion criteria include intra-articular distal humerus fracture (AO type 13C1, 13C2, and 13C3) and patients aged more than 20 years old. However, exclusion criteria included pathological fractures, fractures with open wounds, and patients unfit for surgery. Before surgery, all patients underwent clinical and radiological evaluations to assess for associated injuries. A local examination was performed to exclude open wounds and assess neurovascular status. X-rays (anteroposterior and lateral views) and computed tomography scans of the affected elbow were obtained for deformity assessment, joint reconstruction evaluation, and pre-operative planning (Fig. 1 and 2).
Routine investigations, including complete blood count, liver and renal function tests, viral screening, chest X-ray, and echocardiography, were conducted for all patients. An above-elbow plaster of Paris slab with bandaging was applied to provide temporary support until fracture fixation. Surgery was scheduled after obtaining written and informed consent and after subsidence of swelling.
Surgical technique
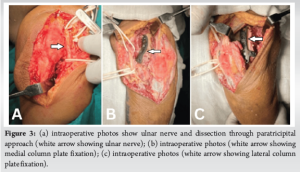
All patients underwent general anesthesia following pre-anesthetic evaluations. The surgical approach, in most cases, involved an olecranon osteotomy followed by a paratricipital approach. Patients were positioned in the lateral decubitus position on a radiolucent table with a bolster under the arm and a pneumatic tourniquet placed around the upper arm. A 15 cm posterior midline incision was made over the elbow, curving laterally or medially to avoid direct incision over the olecranon tip. After superficial and deep dissection, the ulnar nerve was identified and carefully mobilized to prevent damage. Olecranon osteotomy was performed in a chevron pattern with the distal apex sawed off, allowing exposure of the intra-articular surface of the distal humerus. In cases utilizing the paratricipital approach, two windows were created by separating the triceps from the medial and lateral intermuscular septum to expose the medial and lateral columns of the distal humerus. Fracture fragments were identified and reduced using reduction forceps, and provisional fixation was achieved with multiple Kirschner wires. Orthogonal plate fixation involves the placement of an anatomically pre-contoured 3.5 mm reconstruction plate over the medial column of the distal humerus and a lateral plate over the posterior aspect of the lateral column (Fig. 3). Each plate was secured with three screws proximally and three screws distally. Plates varied in length and ended at different levels. After securing the plates, the olecranon was fixed with tension band wiring, followed by anterior transposition of the ulnar nerve.
The average duration of surgery was approximately 148 min. The tourniquet was released after 1 h and 30 min and was not reinflated once deflated. Two different surgeons performed surgeries at a single center. Patients were given an above-elbow plaster of Paris slab and instructed to elevate the arm to reduce swelling postoperatively.
Rehabilitation protocol
Passive ROM exercises for the elbow, including flexion, extension, pronation, and supination, were initiated within 1 week postoperatively. Active movements were allowed to begin after 2 weeks. All patients were provided with an above-elbow plaster of Paris slab after surgery to support and protect the elbow during the initial recovery period.
Follow-up protocol
Most patients were followed up initially at 6 weeks postoperatively and subsequently at 3-month intervals up to 1 year. During each follow-up visit, all patients underwent both radiological and clinical assessments. The clinical evaluation included using the MEPS to assess functional outcomes.
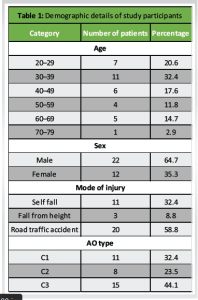
The mean age of the study group was 42.2 ± 14.83 years, ranging from 22 to 76 (Table 1). Of the 34 patients, 11 (32.4%) were in their 3rd decade, and 6 (17.6%) were in their 6th and 7th decades. Males were more frequently affected 22 (64.7%) than females (Table 1). The right side was predominantly affected 19 (55.9%). Overall, road traffic accidents totaled 20 (58.8%) and were the most common mode of injury. Road traffic accidents were predominant among young individuals, whereas self-falls were more common among elderly patients. All patients had complete articular (intra-articular) distal humerus fractures classified as AO type C. The most common subtype was AO type C3, followed by AO type C1 and C2 (Table 1). The mean surgical duration was 148.82 ± 26.63 min, ranging from 110 to 200 min. The study group was successfully followed for an average period of 14.29 ± 3.13 months, ranging from 9 to 18 months.
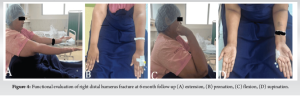
The average time for bone union was 14.94 ± 3.27 weeks, ranging from 10 to 22 weeks. No cases of non-union were observed in this study group. Serial X-rays were performed during the follow-up period to monitor signs of the union. The mean range of flexion was 117.2° (Fig. 4). The mean MEPS was 82.058 ± 10.66. According to MEPS, outcomes were excellent to good in 29 (85.3%) of cases, fair in 3 (8.8%), and poor in 2 (5.9%) of individuals (Table 2). No significant differences were noted in functional recovery between patients with and without olecranon osteotomy, between right- and left-sided fractures, and between male and female patients.
Distal humerus fractures are typically comminuted and intra-articular, directly impacting elbow mobility. Managing these fractures is challenging due to the complex anatomy of the elbow and the limited subchondral bone [4]. Successful restoration of elbow function hinges on three key factors: Exposure during surgery, fracture fixation, and post-operative rehabilitation [5]. Optimal exposure is crucial and can be achieved through a posterior approach with olecranon osteotomy or a paratricipital approach. Anatomical reduction and the use of column-specific plates are essential for achieving favorable outcomes. After reduction, provisional fixation with K-wires and bone clamps is performed, and maintaining or recreating the olecranon fossa is critical. Dual plating offers stability and precise reduction and facilitates early elbow mobilization. Two methods of dual plating include orthogonal and parallel orientations. In orthogonal plating, one plate is applied over the medial column and another over the posterior aspect of the lateral column. Despite ongoing debates about the best treatment for distal humerus fractures, double plating fixation has been shown to yield favorable clinical outcomes, even in cases of complex intra-articular fractures [6]. The osteotomized olecranon is fixed with tension band wiring to provide sufficient stability to the elbow. Studies have reported positive outcomes with orthogonal plating for AO type C distal humerus fractures. For instance, Huang et al. achieved good to excellent results in 100% of cases treated with perpendicular plating [7]. Aslam and Willett reported a 70% good to excellent functional outcomes rate with a mean flexion arc of 112° [8]. Gofton et al. found that patients treated with orthogonal plating had a flexion arc of 122° with a 17° loss of flexion torque, and 93% were satisfied with their functional outcomes [9]. Jacobson et al. highlighted the preference for orthogonal plating due to reduced stiffness in the sagittal plane [10]. In our study, males were more affected than females (M:F = 1.8:1), and the mean MEPS was 82, with good to excellent results reported in 29 (85.3%) cases. The mean flexion-extension arc was 117.2°, and all patients showed radiological evidence of fracture union within 14.9 weeks. Orthogonal plating provided stable and rigid fixation with satisfactory functional outcomes. However, Sanchez-Sotelo et al. in the Mayo Clinic introduced a principle-based parallel-plate technique and showed that the mean flexion-extension arc was 99° and the mean MEPS was 85 points [11]. Athwal et al. studied 37 patients with type C distal humeral fractures treated by the bicolumn parallel plating system and found that the mean arc of elbow flexion-extension motion was 97°, and the mean MEPS was 82 points [12]. Some previous studies have shown a 48% post-operative complication rate in AO type C distal humerus fracture [13,14]. The main complications are transient ulnar nerve palsy, hypertrophic ossification, and superficial and deep infection. The most common complication is transient ulnar nerve palsy followed by hypertrophic ossification. The incidence rate of heterotrophic ossification widely varies in the literature from 4% to 49% [14,15]. In our study, the complication rate was 6 (17.5%), with superficial and soft tissue infections in 5.9% (2 cases) and transient ulnar nerve palsy in 2.9% (one case), resolved within 2 months postoperatively as shown in Fig. 5 and Table 3. There were no incidents of heterotrophic ossification. Limitations of our retrospective study include a small sample size and a relatively short follow-up period. Despite these limitations, our study demonstrates satisfactory functional outcomes and a low complication rate with orthogonal plating in intra-articular distal humerus fractures.
Accurate reduction and rigid internal fixation with early mobilization are crucial goals for achieving favorable functional outcomes in intra-articular distal humerus fractures. Orthogonal plating using anatomical locking pre-contoured plates effectively addresses both objectives. Our retrospective study achieved good to excellent functional outcomes in approximately the majority of cases, even in patients with highly comminuted fractures and osteoporosis, with minimal complications. Therefore, we conclude that orthogonal plating is a reliable treatment option regardless of age, sex, or the specific intra-articular distal humerus fracture type.
Orthogonal dual plating is a reliable surgical technique for treating intra-articular distal humerus fractures, providing stable fixation and enabling early mobilization. This method achieves favorable functional outcomes, with good to excellent results in approximately 85% of cases, even for complex or comminuted fractures. Complication rates are minimal, making it an effective treatment choice across diverse patient demographics, including those with osteoporosis.
References
- 1.Rose SH, Melton LJ, Morrey BF, Ilstrup DM, Riggs BL. Epidemiologic features of humeral fractures. Clin Orthop Relat Res 1982;168:24-30. [Google Scholar]
- 2.Robinson CM, Hill RM, Jacobs N, Dall G, Court-Brown CM. Adult distal humeral metaphyseal fractures: Epidemiology and results of treatment. J Orthop Trauma 2003;17:38-47. [Google Scholar]
- 3.Yu X, Xie L, Wang J, Chen C, Zhang C, Zheng W. Orthogonal plating method versus parallel plating method in the treatment of distal humerus fracture: A systematic review and meta-analysis. Int J Surg 2019;69:49-60. [Google Scholar]
- 4.Lee SK, Kim KJ, Park KH, Choy WS. A comparison between orthogonal and parallel plating methods for distal humerus fractures: A prospective randomized trial. Eur J Orthop Surg Traumatol 2014;24:1123-31. [Google Scholar]
- 5.Vashistha D, Naik S, Nandi S, Kulkarni S. Clinical outcome of treatment of intra-articular distal humerus fracture with open reduction and internal fixation by orthogonal locking plate: A prospective study. Int J Res Orthop 2020;6:471-6. [Google Scholar]
- 6.Gupta R, Khanchandani P. Intercondylar fractures of the distal humerus in adults: A critical analysis of 55 cases. Injury 2002;33:511-5. [Google Scholar]
- 7.Huang YM, Chen CY, Lin KC, Tarng YW, Liao CY, Chang WN. Functional outcomes following fixation of a marginal distal radius fracture with two commonly used volar locking plates: A retrospective cohort study. BMC Musculoskelet Disord 2022;23:18. [Google Scholar]
- 8.Aslam N, Willett K. Functional outcome following internal fixation of intraarticular fractures of the distal humerus (AO type C). Acta Orthop Belg 2004;70:118-22. [Google Scholar]
- 9.Gofton WT, MacDermid JC, Patterson SD, Faber KJ, King GJ. Functional outcome of AO type C distal humeral fractures. J Hand Surg Am 2003;28:294-308. [Google Scholar]
- 10.Jacobson SR, Glisson RR, Urbaniak JR. Comparison of distal humerus fracture fixation: A biomechanical study. J South Orthop Assoc 1997;6:241-9. [Google Scholar]
- 11.Sanchez-Sotelo J, Torchia ME, OʼDriscoll SW. Complex distal humeral fractures: Internal fixation with a principle-based parallel-plate technique. J Bone Joint Surg Am 2007;89:961-9. [Google Scholar]
- 12.Athwal GS, Hoxie SC, Rispoli DM, Steinmann SP. Precontoured parallel plate fixation of AO/OTA type C distal humerus fractures. J Orthop Trauma 2009;23:575-80. [Google Scholar]
- 13.Södergård J, Sandelin J, Böstman O. Postoperative complications of distal humeral fractures. 27/96 Adults followed up for 6 (2-10) years. Acta Orthop Scand 1992;63:85-9. [Google Scholar]
- 14.Pajarinen J, Björkenheim JM. Operative treatment of type C intercondylar fractures of the distal humerus: Results after a mean follow-up of 2 years in a series of 18 patients. J Shoulder Elbow Surg 2002;11:48-52. [Google Scholar]
- 15.Kundel K, Braun W, Wieberneit J, Rüter A. Intraarticular distal humerus fractures. Factors affecting functional outcome. Clin Orthop Relat Res 1996;332:200-8. [Google Scholar]