Pigmented villonodular synovitis is a rare condition; surgeons should be aware of the possible intraligamentous presence and should suspect it during arthroscopy if the anterior cruciate ligament is swollen and not normal on probing.
Dr. Hesham Mohamed Gawish, Department of Orthopedic Surgery and Traumatology, Faculty of Medicine, Kafr El Sheikh University, Kafr El-Sheikh, Egypt. E-mail: hichamgawish@gmail.com
Introduction: Pigmented villonodular synovitis arising from cruciate ligaments is a very rare condition. Arthroscopic management of these lesions is the treatment of choice. Probing of the anterior cruciate ligament (ACL) is very crucial due to the possibility of intraligamentous invasion of this lesion.
Case Report: A 40-year-old male patient had anterior knee pain and effusion without giving way. There was no history of trauma before the presentation. In his last attack of locking, he had knee effusion for the 1st time. His magnetic resonance imaging scan revealed partial ACL injury along with intercondylar notch soft-tissue mass, i.e., nodular synovitis. The lesion was seen between the ACL and lateral femoral condyle during arthroscopy. The rest of the lesion was inside the substance of the ACL. After the complete removal of the lesion, ACL reconstruction was done. Microscopic examination revealed a localized pigmented villonodular synovitis.
Conclusion: Specific signs and symptoms for pigmented villonodular synovitis are lacking. Surgeons should have a very high suspicion of intra-articular localization for this type of lesion. Preparation of ligamentous reconstruction is recommended in case of complete ligamentous invasion by the tumor.
Keywords: Pigmented villonodular synovitis, anterior cruciate ligament, arthroscopic synovectomy.
Pigmented villonodular synovitis (PVNS) or the tenosynovial giant-cell tumor (GCT) inside the knee joint is a rare condition. It is reported to present either in a diffuse form or nodular form (GCT) [1]. This tumor arises from the synovial sheath of the fibrous tissue surrounding the joints, tendon sheaths, mucosal bursas, ligaments, and tendons. The tenosynovial GCT has four clinicopathological variants: The localized type, the diffuse extra-articular, the diffuse intra-articular, and the malignant. The localized type of tenosynovial GCT is defined as a circumscribed lesion that is microscopically not infiltrating into the fat of skeletal muscles [2]. The GCT of the tendon sheath is morphologically identical to the localized PVNS, whose most common location is the knee. It typically occurs between the ages of 30 and 50 [3]. Kim et al. [4] first reported a case of a localized and intra-articular type of tenosynovial GCT of the knee attached to the synovium on the anterior horn of the medial meniscus in 1995. Otsuka et al., [5] in 1996, first reported a case of intra-articular tenosynovial GCT arising from the anterior cruciate ligament (ACL). It was also reported to arise from the posterior cruciate ligament (PCL) [6].
In this case, we report a rare presentation of intra-ligamentous PVNS inside the ACL substance that was not seen on the initial knee arthroscopic examination with simultaneous ACL reconstruction.
Case presentation of a male patient with ACL PVNS
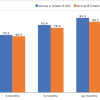
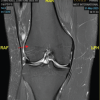
A 40-year-old male patient, medically free, presented with left knee pain for 9 months. The pain was predominantly an anterior knee pain without giving way. However, there were frequent attacks of locking. He works as an accountant. His favorite sport is football on a weekly basis. There was no history of trauma before the presentation. In his last attack of locking, he had knee effusion for the 1st time. On clinical examination, there was moderate knee effusion, full extension, and flexion up to 140°. Lachman test, anterior drawer test, Pivot-Shift test, McMurray, and Apley test were negative. Routine laboratory investigations were normal. Anteroposterior and lateral radiographs were normal (Fig. 1), and the patient underwent a magnetic resonance imaging (MRI) scan of his left knee. On the MRI examination, there was thickening of the ACL with intact attachment along with some knee effusion (Fig. 2). The patient underwent conservative therapy for 6 months in the form of aggressive physical therapy, core strengthening, daily activities modifications, and medical treatment. Thereafter, a new MRI scan was done, which revealed partial ACL injury along with intercondylar notch soft tissue mass, i.e., nodular synovitis (Fig. 3).

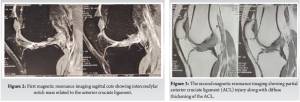
Due to the persistence of his symptoms, an arthroscopic excision of the lesion was decided with a biopsy taken for histopathological examination. In the arthroscopic examination, the menisci, PCL, and articular cartilage were normal. A round mass with a reddish-brown color was located just beside the ACL impinging between the ACL and lateral femoral condyle (Fig. 4). This lesion was excised with the use of basket forceps and the motorized shaver blade 5.5 mm (Fig. 5).
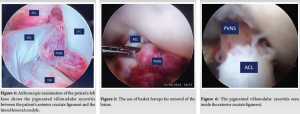
On probing the ACL, it was swollen and not normal. When the probe was used to invaginate between ACL fibers, the rest of the lesion appeared to be inside the substance of ACL. A motorized shaver was used to debride the ACL fibers and the lesion was surprisingly invading the whole substance of the ACL from the inside (Fig. 6-8).
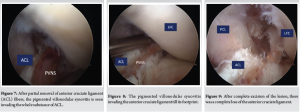
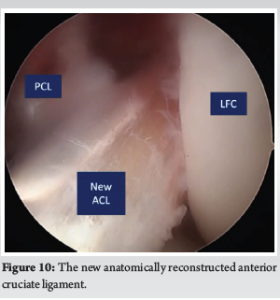
After the complete removal of the lesion, the ACL was completely lost (Fig. 9). The semitendinosus tendon was harvested for proper ligament reconstruction. The ACL reconstruction was done and fixed in the original footprint of the native ACL (Fig. 10). The patient was then subjected to an ACL rehabilitation program.
Microscopic examination reported a localized PVNS with the presence of multinucleated giant cells and plenty of mononuclear cells with low-grade cellular multiplication. The patient became asymptomatic without pain or loss of extension and returned to his work after 3 months postoperatively. There was no recurrence of either pain or swelling. The patient was followed up for 15 months with no recurrence of symptoms. He regained his sports activities 12 months post-surgery.
The intra-articular PVNS is a rare knee condition. Intraligamentous presentation inside the substance of the ligament is even more extraordinary. The case described here presented a unique, rare form of nodular localized PVNS. We strongly recommend arthroscopic management of these lesions with adequate probing of ligament substance if doubtful-looking cruciate ligaments, along with MRI film reporting a diffuse thickening of the ligament [7]. The etiology of GCT of the tendon sheath or nodular PVNS remains unclear. Many factors have been proposed as possible causes for this condition, including inflammation, trauma, toxin, allergy, clonal chromosomal abnormalities, and overuse [8]. There is a scarcity of specific clinical features for the localized PVNS of the knee, and thus, a thorough clinical examination is prudent, along with high clinical suspicion. Patients present signs of mechanical derangement of the knee. One of the most helpful and, at the same time, non-invasive is the MRI scan. A finding that should raise the suspicion of such a tumor and place it in the differential diagnosis is a hypointense lesion in T1-weighted MRI sequences which obscure the cruciate ligaments, and in T2-weighted MRI sequences that the lesion is hyperintense. MRI diagnosis must be confirmed by histopathological examination. The tumor typically presents as a slowly growing, painless mass of size between 1 and 4 cm [9]. These lesions tend to recur even after complete excision. The recurrence rate is reported to be more than 20%. Therefore, close patient monitoring and follow-up are advisable. Arthroscopic excision has been reported as a safe, minimally invasive, and effective procedure for the treatment of these tumors [10]. Some authors reported the occurrence of a diffuse form with ACL rupture. Chen et al. [11] reported that PVNS may arise with joint instability. They recommended early and reliable stabilization of the joint as this may significantly prevent PVNS and ensure a better clinical outcome. Rajani et al. [12] reported the occurrence of diffuse PVNS after ACLR which resulted in graft failure. However, most papers reported nodular PVNS with either intact or ruptured ACL [13]. Some of them reported second stage of excision and then reconstruction. In our case, we did it in the first stage because we believe that the nodular form has less chance to recur than the diffuse form. Other authors also reported arthroscopic excision of GCT at the femoral attachment of ACL with simultaneous ACL reconstruction [14,15].
PVNS of the knee is a rather rare intra-articular disease. Arthroscopic excision is the treatment of choice. During arthroscopy, it is advisable to probe the ACL. Intraligamentous invasion of the tumor should be suspected. Surgeons should be prepared for this possibility and the need for ACL reconstruction either simultaneously or in another session.
For surgeons, pigmented villonodular synovitis should always be in mind when dealing with painful knee effusions. Preparation of ACL reconstruction should be considered when dealing with this lesion due to the possibility of intra-ligamentous invasion of this tumor.
References
- 1.De Ponti A, Sansone V, Malcherè M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy 2003;19:602-7. [Google Scholar | PubMed]
- 2.Agarwala S, Agrawal P, Moonot P, Sobti A. A rare case of giant cell tumour arising from anterior cruciate ligament: Its diagnosis and management. J Clin Orthop Trauma 2015;6:140-3. [Google Scholar | PubMed]
- 3.Dines JS, DeBerardino TM, Wells JL, Dodson CC, Shindle M, DiCarlo EF, et al. Long-term follow-up of surgically treated localized pigmented villonodular synovitis of the knee. Arthroscopy 2007;23:930-7. [Google Scholar | PubMed]
- 4.Kim SJ, Choi NH, Lee SC. Tenosynovial giant-cell tumor in the knee joint. Arthroscopy 1995;11:213-5. [Google Scholar | PubMed]
- 5.Otsuka Y, Mizuta H, Nakamura E, Kudo S, Inoue S, Takagi K. Tenosynovial giant-cell tumor arising from the anterior cruciate ligament of the knee. Arthroscopy 1996;12:496-9. [Google Scholar | PubMed]
- 6.Camillieri G, Di Sanzo V, Ferretti M, Calderaro C, Calvisi V. Intra-articular tenosynovial giant cell tumor arising from the posterior cruciate ligament. Orthopedics 2012;35:e1116-8. [Google Scholar | PubMed]
- 7.Kramer D, Frassica FJ, Frassica DA, Cosgarea AJ. Pigmented villonodular synovitis of the knee: Diagnosis and treatment. J Knee Surg 2009;22:243-54. [Google Scholar | PubMed]
- 8.Spahn G, Bousseljot F, Schulz HJ, Bauer T. Arthroscopic resection of an extra-articular tenosynovial giant cell tumor from the ankle region. Arthroscopy 2003;19:E8-11. [Google Scholar | PubMed]
- 9.Bojanic I, Ivkovic A, Dotlic S, Ivkovic M, Manojlovic S. Localized pigmented villonodular synovitis of the knee: Diagnostic challenge and arthroscopic treatment: A report of three cases. Knee Surg Sports Traumatol Arthrosc 2001;9:350-4. [Google Scholar | PubMed]
- 10.Loriaut P, Djian P, Boyer T, Bonvarlet JP, Delin C, Makridis KG. Arthroscopic treatment of localized pigmented villonodular synovitis of the knee. Knee Surg Sports Traumatol Arthrosc 2012;20:1550-3. [Google Scholar | PubMed]
- 11.Chen X, Li P, Zhang W, Yin X, Ma Q, Wang K. Higher incidence of diffuse pigmented villonodular synovitis in patients with ruptured cruciate ligament: A case report. Int J Surg Case Rep 2022;100:107720. [Google Scholar | PubMed]
- 12.Rajani R, Ogden L, Matthews CJ, Gibbs CP. Diffuse pigmented villonodular synovitis as a rare cause of graft failure following anterior cruciate ligament reconstruction. Orthopedics 2018;41:e142-4. [Google Scholar | PubMed]
- 13.Galli M, Ciriello V, Menghi A, Perisano C, Maccauro G, Marzetti E. Localized pigmented villonodular synovitis and the anterior cruciate ligament of the knee: An exceptional presentation of a rare disease with neoplastic and inflammatory features. Int J Immunopathol Pharmacol 2012;25:1131-6. [Google Scholar | PubMed]
- 14.Shreekanth KS, Ganiger MH, Didwaniya S, Aravind M. Arthroscopic excision of giant cell tumour at femoral attachment of anterior cruciate ligament and simultaneous anterior cruciate ligament reconstruction: A case report. Int J Res Orthop 2024;10:1091-4. [Google Scholar | PubMed]
- 15.Flevas DA, Karagiannis AA, Patsea ED, Kontogeorgakos VA, Chouliaras VT. Arthroscopic removal of tenosynovial giant-cell tumors of the cruciate ligaments. Presentation of two cases. J Orthop Case Rep 2021;11:23-7. [Google Scholar | PubMed]