Limb Reconstruction System provides stable fixation and early weight-bearing, making it an effective treatment for infected nonunion of long bones
Dr. Janki Sharan Bhadani, Former Senior Resident, IGIMS Patna, Consultant and DNB Appraiser, Paras HMRI Hospital, Patna, Bihar, India. E-mail: jsbhadani@gmail.com
Introduction: Infected non-union of long bones is a complex orthopedic challenge, leading to prolonged disability and healthcare burden. The limb reconstruction system (LRS) offers advantages over the Ilizarov technique, including early weight-bearing, minimal invasiveness, and improved functional outcomes. This study evaluates the clinical and functional outcomes of infected nonunion treated with LRS.
Materials and Methods: A retrospective study was conducted at a tertiary care center in eastern India from January 2019 to June 2023, including a pandemic-affected period. Thirty patients (18–68 years) with infected nonunion of the femur, tibia, and humerus were included. Data on demographics, infection characteristics, prior surgeries, and hematological parameters were recorded. All patients underwent surgical debridement followed by LRS application. Outcomes were assessed using the Association for the Study and Application of the Method of Ilizarov scoring system.
Results: Of 30 patients, 16 had femoral nonunion, 11 tibial, and 3 humeral. Union was achieved in 83.33% (25 cases), and infection eradication in 93.33% (28 cases). The mean time to union was 9.1 months. Complications included joint stiffness (26.67%), pin tract infection (23.33%), and limb length discrepancy (40%). No amputations were required, and re-fracture rates were low.
Conclusion: LRS is a reliable and effective treatment for infected nonunion, enabling early mobilization and good functional outcomes. It provides a stable alternative to Ilizarov fixation with low complication rates.
Keywords: Infected nonunion, limb reconstruction system, external fixation, bone union, orthopedic infection, Ilizarov technique.
Infected nonunion of long bones is a significant cause of both anatomical and functional disability [1]. It also adds to the economic burden on society and affects the patient’s self-esteem. Despite advancements in management, the prevalence of infected nonunion remains high [2]. Infected nonunion is defined as a failure of bone healing with persistent infection at the fracture site for 6–8 months [1]. Bone infections pose a serious challenge for orthopedic surgeons, requiring treatment strategies aimed at eradicating infection, achieving union, and restoring function [3]. The management of infected nonunion is complex and often requires multiple surgical interventions [4]. Treatment options include thorough debridement with skeletal stabilization, the use of antibiotic-coated nails, antibiotic beads with nailing or plating, vascularized grafts, open cancellous bone grafting, antibiotic-impregnated bioabsorbable bone substitutes, and external fixation using ring or rail fixators [5-10]. The Ilizarov technique is a well-established method for treating infected nonunions, especially in cases with large bone defects or limb length discrepancies [11]. Distraction histogenesis using an Ilizarov external fixator is preferred for nonunions with active or quiescent infection and bone gaps of 4 cm or more [12]. The limb reconstruction system (LRS) provides an alternative approach with several advantages, including less invasiveness, early weight-bearing, reduced infection rates, minimal blood loss, prevention of osteoporosis and muscle atrophy, preservation of limb function, and elimination of the need for bone grafting [13,14]. It also allows deformity correction during healing and provides stable fixation [13,15]. Both Ilizarov and LRS have demonstrated effectiveness and reliability in managing infected nonunions [16]. This retrospective study evaluates the outcomes of infected nonunion of long bones treated with the LRS.
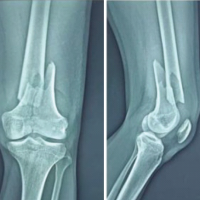
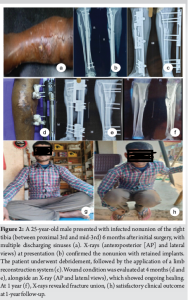
This retrospective study was conducted in the Department of Orthopedics at a tertiary care center in Eastern India after obtaining ethical clearance. The study included patients aged 18–68 years with infected nonunion of the femur, tibia, and humerus, diagnosed clinically, radiologically, and microbiologically between January 2019 and June 2023. A total of 30 cases were managed with the LRS (Fig. 1, 2). Skeletally immature patients (<18 years), those with head injuries, neurological impairments, chronic debilitating conditions, bedridden status, or unwillingness to participate were excluded.

Patient data, including demographic details, duration and mode of injury, medical history, presence of sinus and pus discharge, number of previous surgeries, tenderness, shortening, deformity, bone defect, and neurovascular status, were recorded. Hematological investigations included hemoglobin, total and differential leukocyte counts, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). Culture samples were collected from discharging sinuses. Radiological assessment involved anteroposterior X-rays, and cases were classified according to Jain AK’s classification for infected nonunion [17]. Surgical intervention consisted of debridement, lavage, and LRS application. The procedure involved implant removal, excision of non-viable soft tissue, fibrosis, and necrotic bone, followed by thorough debridement until cortical bleeding was evident. Intraoperative samples were collected from multiple sites for Gram staining, culture sensitivity, and mycobacterial cultures. The medullary canal was reconstituted, and open reduction of the main fragments was performed. Outcomes were assessed using the Association for the Study and Application of Methods of Ilizarov (ASAMI) scoring system [18,19].
Demographic and clinical data
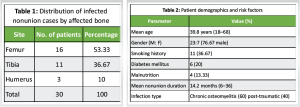
The study included 30 patients with infected nonunion affecting the femur (n = 16, 53.33%), tibia (n = 11, 36.67%), and humerus (n = 3, 10%) (Table 1). The mean age was 39.8 years (range: 18–68 years), with a male predominance (M: F = 23:7, 76.67%). Notable comorbidities included diabetes mellitus (20%), smoking (36.67%), and malnutrition (13.33%). The mean duration of nonunion before treatment was 14.2 months (range: 6–36 months) (Table 2). Chronic osteomyelitis (60%) was the most common infection type, whereas post-traumatic infections accounted for 40% of cases.
Microbiological and hematological findings
The microbiological analysis identified Staphylococcus aureus as the most common pathogen (50%), followed by Pseudomonas aeruginosa (20%) and Klebsiella pneumoniae (10%). Hematological findings showed elevated inflammatory markers preoperatively, with a mean ESR of 47.2 mm/h and CRP of 19.8 mg/L, both of which significantly decreased following treatment.
Treatment details
All patients underwent surgical debridement and stabilization using the LRS. A single-stage procedure was performed in 16 patients (53.33%), while 14 patients (46.67%) required a staged approach due to persistent infection or extensive bone loss. Bone grafting was performed in 18 cases (60%) using autografts, and bone substitutes (calcium phosphate) in 16.67% of cases.
Postoperative rehabilitation protocol
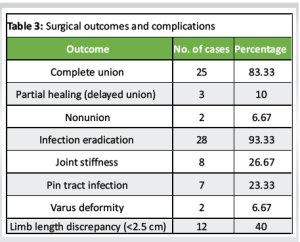
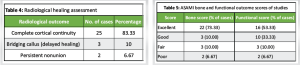
Partial weight-bearing was initiated at 6 weeks postoperatively, while full weight-bearing was achieved at a mean of 9.8 months (range: 7–16 months). Physical therapy focused on range-of-motion exercises and progressive muscle strengthening, beginning in the early postoperative period to minimize stiffness and improve function. Patients were monitored regularly to assess rehabilitation progress and adjust weight-bearing status accordingly. The mean time to frame removal was 8.5 months (range: 6–14 months). The mean time to union was 9.1 months (range: 6–14 months), with complete union achieved in 25 cases (83.33%). A comparative analysis with existing studies revealed no significant difference in union rates (P = 0.42, 95% confidence interval (CI): 75.2–91.5%). Partial weight-bearing was initiated at 6 weeks postoperatively, while full weight-bearing was achieved at a mean of 9.8 months (range: 7–16 months) (Table 3). Radiological assessment revealed cortical continuity in 25 cases (83.33%), delayed healing in 3 cases (10%), and persistent nonunion in 2 cases (6.67%) (Table 4).
ASAMI bone and functional scores
The bone score assessment showed that 22 cases (73.33%) had excellent outcomes, 3 cases (10%) had good results, 3 cases (10%) had fair results, and 2 cases (6.67%) had poor outcomes. The functional score evaluation indicated that 16 cases (53.33%) achieved excellent functional outcomes, 10 cases (33.33%) had good results, 3 cases (10%) had fair results, and 2 cases (6.67%) had poor results (Table 5). Notably, patients with better bone healing demonstrated significantly improved functional outcomes (P < 0.05, r = 0.71), suggesting a strong correlation between radiological healing and functional recovery.
Complications and follow-up
The mean follow-up duration was 18 months (range: 12–30 months). Infection eradication was achieved in 28 cases (93.33%), i.e., infection eradication rates (P = 0.38, 95% CI: 85.6–97.8%). Two cases (6.67%) required additional intervention. Late complications included joint stiffness in 26.67% of cases, pin tract infections in 23.33%, and limb length discrepancies in 40%, most of which were <2.5 cm and managed with shoe modifications. Varus deformity was observed in 6.67% of cases, and hardware loosening occurred in 3.33%. Notably, no amputations were required.
The management of infected nonunion remains a significant challenge in orthopedic surgery, requiring a meticulous approach to eradicate infection, restore bone integrity, and optimize functional outcomes [20]. Our study, which utilized the LRS for the treatment of infected nonunions, demonstrated encouraging results in terms of union rates, infection control, and functional recovery [21,22]. When compared with previous similar studies, our findings align well with existing literature while also highlighting some unique trends. The treatment of nonunion in long bones using distraction osteogenesis has been well-documented in the literature, with both Ilizarov and monorail fixators LRS demonstrating comparable functional outcomes [21,22]. Arfee et al., found no significant difference in clinical or radiographic outcomes between Ilizarov and LRS fixators for infected tibial nonunion [23]. However, their study noted better patient acceptance with LRS due to its relative ease of use.
Demographics and clinical profile
The demographic distribution of our study showed a predominance of femoral (53.33%) and tibial (36.67%) involvement, which is consistent with reports by Seenappa et al. and Rohilla et al., where tibial involvement was predominant [22,24]. Our mean patient age (39.8 years) was similar to that reported by Chen et al. and Gupta et al., reinforcing the notion that infected nonunions predominantly affect young to middle-aged adults, often in the productive workforce [25,26]. The male predominance (76.67%) observed in our cohort is consistent across multiple studies, including those by Yin et al. and Zhang et al., which also reported higher male representation (92/18 and 31/10, respectively) [27,28]. Our study also highlighted important comorbidities, including diabetes mellitus (20%), smoking (36.67%), and malnutrition (13.33%), which have been recognized as contributing factors to delayed healing and recurrent infections. These risk factors were not consistently reported in previous studies, indicating an area for further exploration in future research [29,30].
Infection control and microbiological outcomes
The primary goal in managing infected nonunion is eradicating infection before attempting definitive reconstruction. In our study, S. aureus was the most common pathogen (50%), followed by P. aeruginosa (20%) and K. pneumoniae (10%). These findings are consistent with global microbiological trends, as S. aureus has been the most frequently isolated organism in similar studies [31]. Infection eradication was achieved in 93.33% of cases, which compares favorably to previous reports where eradication rates ranged from 85% to 90% [22,32].
Surgical approach and bone defect management
Our study employed both single-stage (53.33%) and staged (46.67%) approaches, with bone grafting performed in 60% of cases. The mean bone defect size in our cohort was 6.5 cm, similar to that reported by Chen et al. (6.5 cm) and Gupta et al. (6.4 cm) [25,26]. The use of LRS for bone transport was a key factor in achieving favorable outcomes, as demonstrated in prior studies, where mean bone defects ranged from 5.06 cm (Seenappa et al., 2013) to 10.1 cm (Zhang et al., 2017) [22,28]. Bone transport using LRS remains a gold-standard technique for managing segmental defects, as shown in multiple studies. Our findings align with the work of Rohilla et al., who reported a mean defect size of 5.78 cm and a union rate of 79% using LRS, closely mirroring our union rate of 83.33% [24].
Union rates and functional outcomes
The overall union rate in our study was 83.33%, consistent with the reported range of 80–85% in previous studies using LRS. Seenappa et al. reported a 27-month mean follow-up and a union rate of 66%, whereas our study had a mean follow-up of 18 months, with union achieved within 9.1 months on average [22]. Studies with higher mean bone defect sizes, such as Zhang et al., which reported a mean defect size of 10.1 cm, showed lower union rates due to the increased complexity of reconstruction [28]. The functional outcomes in our cohort were assessed using the ASAMI score, revealing 73.33% excellent and 10% good outcomes, while Seenappa et al. achieved excellent outcomes on 49%, while good outcomes on 50%, Hashmi et al. achieved 42% excellent, and 50% good outcome [22,33]. Lu et al. reported a mean follow-up of 57 months with a functional success rate of 50%, which is slightly lower than our findings [32]. The direct correlation between bone healing and functional improvement (P < 0.05, r = 0.71) in our study underscores the importance of achieving solid union to ensure optimal patient mobility and quality of life.
Complications and challenges
The most common complications encountered in our study were joint stiffness (26.67%), pin tract infections (23.33%), and limb length discrepancies (40%). These complications were similarly reported in previous studies, such as Yin et al., where pin tract infections were noted in 20% of cases, and Gupta et al., who documented limb length discrepancies in 38% of patients [26,27]. Maheshwari et al. reported pin tract infection as the most common complication, followed by joint stiffness and deformities [21]. Our findings similarly indicate joint stiffness (26.67%) and pin tract infections (23.33%) as major complications, while limb length discrepancy was observed in 40% of cases, mostly manageable with shoe modifications. The higher rate of pin tract infections in our study may be attributed to prolonged frame duration, averaging 8.5 months. However, no amputations were required, reinforcing the efficacy of LRS in limb salvage procedures. With an 18-month follow-up, this study provides a reliable assessment of long-term outcomes. Its findings are consistent with previous research, strengthening their credibility. In addition, identifying key complications and their management enhances its relevance to clinical practice. This study does not include a comparison with other treatment modalities like the Ilizarov fixator, limiting its comparative value. The small sample size restricts the generalizability of the findings, and functional outcomes were assessed qualitatively rather than with standardized scoring systems. Future research should focus on a randomized controlled trial comparing Ilizarov and LRS fixators in terms of infection control, healing time, and patient-reported outcomes. The use of standardized assessment tools, such as the ASAMI criteria, would improve the evaluation of functional recovery. In addition, long-term follow-up is needed to assess the durability of limb function and complication rates over time.
The LRS is an effective option for managing long bone nonunions, achieving high union rates and infection eradication. However, challenges such as comorbidities, large bone defects, and postoperative complications necessitate an individualized treatment approach. Our findings highlight the importance of early weight-bearing progression and structured rehabilitation in optimizing functional recovery. Future research should focus on refining fixation techniques, minimizing complications, and developing standardized rehabilitation protocols to improve long-term patient outcomes.
The LRS is a reliable option for managing infected nonunion of long bones, offering stable fixation and early weight-bearing. It helps control infection, promotes bone healing, and avoids the need for extensive bone grafting. Proper patient selection and adherence to post-treatment protocols are crucial for optimal outcomes.
References
- 1.Nicholson JA, Makaram N, Simpson A, Keating JF. Fracture nonunion in long bones: A literature review of risk factors and surgical management. Injury 2021;52(Suppl 2): S3-11. [Google Scholar | PubMed]
- 2.Flores MJ, Brown KE, O’Marr JM, Adejuyigbe B, Rodarte P, Gomez-Alvarado F, et al. The economic impact of infection and/or nonunion on long-bone shaft fractures: A systematic review. OTA Int 2024;7: e337. [Google Scholar | PubMed]
- 3.Qin L, Yang S, Zhao C, Yang J, Li F, Xu Z, et al. Prospects and challenges for the application of tissue engineering technologies in the treatment of bone infections. Bone Res 2024; 12:28. [Google Scholar | PubMed]
- 4.Kanakaris NK, Tosounidis TH, Giannoudis PV. Surgical management of infected non-unions: An update. Injury 2015;46(Suppl 5): S25-32. [Google Scholar | PubMed]
- 5.Ismat A, Walter N, Baertl S, Mika J, Lang S, Kerschbaum M, et al. Antibiotic cement coating in orthopedic surgery: A systematic review of reported clinical techniques. J Orthop Traumatol 2021; 22:56. [Google Scholar | PubMed]
- 6.Wang L, Lu S, Luo W, Wang G, Zhu Z, Liu Y, et al. Efficacy comparison of antibiotic bone cement-coated implants and external fixations for treating infected bone defects. Int Orthop 2023; 47:1171-9. [Google Scholar | PubMed]
- 7.Chaudhary MM. Infected nonunion of tibia. Indian J Orthop 2017; 51:256-68. [Google Scholar | PubMed]
- 8.Ueng SW, Wei FC, Shih CH. Management of femoral diaphyseal infected nonunion with antibiotic beads local therapy, external skeletal fixation, and staged bone grafting. J Trauma 1999; 46:97-103. [Google Scholar | PubMed]
- 9.Agashe VM, Bhadani JS, Maini L. Beyond hardware: The orthoplastic approach to managing infected nonunions. Indian J Orthop 2024; 58:1777-81. [Google Scholar | PubMed]
- 10.Shyam AK, Sancheti PK, Patel SK, Rocha S, Pradhan C, Patil A. Use of antibiotic cement-impregnated intramedullary nail in treatment of infected non-union of long bones. Indian J Orthop 2009; 43:396-402. [Google Scholar | PubMed]
- 11.Li J, Li M, Wang W, Li B, Liu L. Evolution and development of Ilizarov technique in the treatment of infected long bone nonunion with or without bone defects. Orthop Surg 2022; 14:824-30. [Google Scholar | PubMed]
- 12.Murray JH, Fitch RD. Distraction histiogenesis: Principles and indications. J Am Acad Orthop Surg 1996; 4:317-27. [Google Scholar | PubMed]
- 13.Sharma B, Kumar Shakunt R, Patel J, Pal CP. Outcome of limb reconstruction system in tibial infected non-union and open tibial diaphysial fracture with bone loss. J Clin Orthop Trauma 2021; 15:136-8. [Google Scholar | PubMed]
- 14.Chahar HS, Gupta M, Kumar V, Yadav R, Patel J, Pal CP. Prospective evaluation of role of limb reconstruction system (Rail External Fixator) in open fractures and infected non-union of femur. J Orthop Case Rep 2021; 11:5-11. [Google Scholar | PubMed]
- 15.Bisaccia M, Rinonapoli G, Meccariello L, Caraffa A, Cukierman B, Iborra JR. The challenges of monoaxial bone transport in orthopedics and traumatology. Ortop Traumatol Rehabil 2017; 19:373-8. [Google Scholar | PubMed]
- 16.Saleh AK, Yusof NM, Attallah AA, Elshal EA, Khames AA, Ibrahim MN, et al. Ilizarov external fixator versus orthofix LRS in management of femoral osteomyelitis: A propensity scores matched analysis. Indian J Orthop 2024; 58:1272-7. [Google Scholar | PubMed]
- 17.Jain AK, Sinha S. Infected nonunion of the long bones. Clin Orthop Relat Res 2005; 431:57-65. [Google Scholar | PubMed]
- 18.Testa G, Vescio A, Aloj DC, Costa D, Papotto G, Gurrieri L, et al. Treatment of infected tibial non-unions with Ilizarov technique: A case series. J Clin Med 2020; 9:1352. [Google Scholar | PubMed]
- 19.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res 1990; 250:81-104. [Google Scholar | PubMed]
- 20.Mukhopadhaya J, Bhadani JS, Maini L. Managing nonunion in orthopedic surgery. Indian J Orthop 2024; 58:1677-9. [Google Scholar | PubMed]
- 21.Maheshwari V, Raja BS, Bahadur B, Regmi A, Dhingra M, Gowda AK. Outcome analysis of Ilizarov and monorail fixators in the treatment of nonunion of long bones: A systematic review and proportion meta-analysis. J Clin Orthop Trauma 2023; 40:102170. [Google Scholar | PubMed]
- 22.Seenappa HK, Shukla MK, Narasimhaiah M. Management of complex long bone nonunions using limb reconstruction system. Indian J Orthop 2013; 47:602-7. [Google Scholar | PubMed]
- 23.Arfee S, Malik AT, Nehru A, Ali U, Arfee A, Arfee AA. Clinicoradiological comparison of outcomes of LRS fixator and Ilizarov in infected nonunion of tibia based on bone gap quantification: Original research. J Pharm Bioallied Sci 2022;14: S295-7. [Google Scholar | PubMed]
- 24.Rohilla R, Wadhwani J, Devgan A, Singh R, Khanna M. Prospective randomised comparison of ring versus rail fixator in infected gap nonunion of tibia treated with distraction osteogenesis. Bone Joint J 2016;98-B:1399-405. [Google Scholar | PubMed]
- 25.Chen X, Zhang W, Yu Z, Wang Y, Zhang S, Song T. Application of bone transport with unilateral external fixator combined with locked plate internal fixation in treatment of infected tibial nonunion. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2019; 33:328-31. [Google Scholar | PubMed]
- 26.Gupta S, Malhotra A, Mittal N, Garg SK, Jindal R, Kansay R. The management of infected nonunion of tibia with a segmental defect using simultaneous fixation with a monorail fixator and a locked plate. Bone Joint J 2018;100-B:1094-9. [Google Scholar | PubMed]
- 27.Yin P, Zhang Q, Mao Z, Li T, Zhang L, Tang P. The treatment of infected tibial nonunion by bone transport using the Ilizarov external fixator and a systematic review of infected tibial nonunion treated by Ilizarov methods. Acta Orthop Belg 2014; 80:426-35. [Google Scholar | PubMed]
- 28.Zhang Q, Zhang W, Zhang Z, Zhang L, Chen H, Hao M, et al. Femoral nonunion with segmental bone defect treated by distraction osteogenesis with monolateral external fixation. J Orthop Surg Res 2017; 12:183. [Google Scholar | PubMed]
- 29.Shibuya N, Humphers JM, Fluhman BL, Jupiter DC. Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J Foot Ankle Surg 2013; 52:207-11. [Google Scholar | PubMed]
- 30.Nunna RS, Ostrov PB, Ansari D, Dettori JR, Godolias P, Elias E, et al. The risk of nonunion in smokers revisited: A systematic review and meta-analysis. Global Spine J 2022; 12:526-39. [Google Scholar | PubMed]
- 31.Ganta A, Tong Y, Boadi BI, Konda SR, Egol KA. Microbiome of infected fracture nonunion: Does it affect outcomes? J Orthop Sci 2024; 29:1270-3. [Google Scholar | PubMed]
- 32.Lu V, Zhang J, Zhou A, Krkovic M. Management of post-traumatic femoral defects with a monorail external fixator over an intramedullary nail. Eur J Orthop Surg Traumatol 2022; 32:1119-26. [Google Scholar | PubMed]
- 33.Hashmi MA, Ali A, Saleh M. Management of non-unions with mono-lateral external fixation. Injury 2001;32(Suppl 4):SD30-4. [Google Scholar | PubMed]